Is Aspartame’s Reputation Well-Deserved?
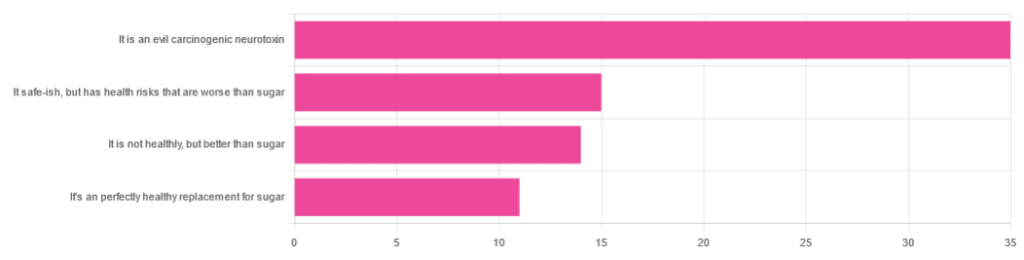
In Tuesday’s newsletter, we asked you for your health-related opinions on aspartame, and got the above-depicted, below-described, set of responses:
- About 47% said “It is an evil carcinogenic neurotoxin”
- 20% said “It is safe-ish, but has health risks that are worse than sugar”
- About 19% said “It is not healthy, but better than sugar”
- About 15% said “It’s a perfectly healthy replacement for sugar”
But what does the science say?
Aspartame is carcinogenic: True or False?
False, assuming consuming it in moderation. In excess, almost anything can cause cancer (oxygen is a fine example). But for all meaningful purposes, aspartame does not appear to be carcinogenic. For example,
❝The results of these studies showed no evidence that these sweeteners cause cancer or other harms in people.❞
~ NIH | National Cancer Institute
Source: Artificial Sweeteners and Cancer
Plenty of studies and reviews have also confirmed this; here are some examples:
- Evaluation of aspartame cancer epidemiology studies based on quality appraisal criteria
- Aspartame, low-calorie sweeteners and disease: Regulatory safety and epidemiological issues
- Aspartame: A review of genotoxicity data
Why then do so many people believe it causes cancer, despite all the evidence against it?
Well, there was a small study involving giving megadoses to rats, which did increase their cancer risk. So of course, the popular press took that and ran with it.
But those results have not been achieved outside of rats, and human studies great and small have all been overwhelmingly conclusive that moderate consumption of aspartame has no effect on cancer risk.
Aspartame is a neurotoxin: True or False?
False, again assuming moderate consumption. If you’re a rat being injected with a megadose, your experience may vary. But a human enjoying a diet soda, the aspartame isn’t the part that’s doing you harm, so far as we know.
For example, the European Food Safety Agency’s scientific review panel concluded:
❝there is still no substantive evidence that aspartame can induce such effects❞
~ Dr. Atkin et al (it was a pan-European team of 21 experts in the field)
Source: Report on the Meeting on Aspartame with National Experts
See also,
❝The data from the extensive investigations into the possibility of neurotoxic effects of aspartame, in general, do not support the hypothesis that aspartame in the human diet will affect nervous system function, learning or behavior.
The weight of existing evidence is that aspartame is safe at current levels of consumption as a nonnutritive sweetener.❞
and
❝The safety testing of aspartame has gone well beyond that required to evaluate the safety of a food additive.
When all the research on aspartame, including evaluations in both the premarketing and postmarketing periods, is examined as a whole, it is clear that aspartame is safe, and there are no unresolved questions regarding its safety under conditions of intended use.❞
Source: Regulatory Toxicology & Pharmacology | Aspartame: Review of Safety
Why then do many people believe it is a neurotoxin? This one can be traced back to a chain letter hoax from about 26 years ago; you can read it here, but please be aware it is an entirely debunked hoax:
Urban Legends | Aspartame Hoax
Take care!





