Coffee, From A Blood Sugar Management Perspective
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite French biochemist (Jessie Inchauspé) is back, and this time, she’s tackling a topic near and dear to this writer’s heart: coffee ☕💕
What to consider
Depending on how you like your coffee, some or all of these may apply to you:
- Is coffee healthy? Coffee is generally healthy, reducing the risk of type 2 diabetes by improving fat burning in the liver and protecting beta cells in the pancreas.
- Does it spike blood sugars? Usually not so long as it’s black and unsweetened. Black coffee can cause small glucose spikes in some people due to stress-induced glucose release, but only if it contains caffeine.
- When is it best to drink it? Drinking coffee after breakfast, especially after a poor night’s sleep, can actually reduce glucose and insulin spikes.
- What about milk? All milks cause some glucose and insulin spikes. While oat milk is generally healthy, for blood sugar purposes unsweetened nut milks or even whole cow’s milk (but not skimmed; it needs the fat) are better options as they cause smaller spikes.
- What about sweetening? Adding sugar to coffee, especially on an empty stomach, obviously leads to large glucose spikes. Alternative sweeteners like stevia or sweet cinnamon are fine substitutes.
For more details on all of those things, plus why Kenyan coffee specifically may be the best for blood sugars, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Bitter Truth About Coffee (or is it?)
- Caffeine: Cognitive Enhancer Or Brain-Wrecker?
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
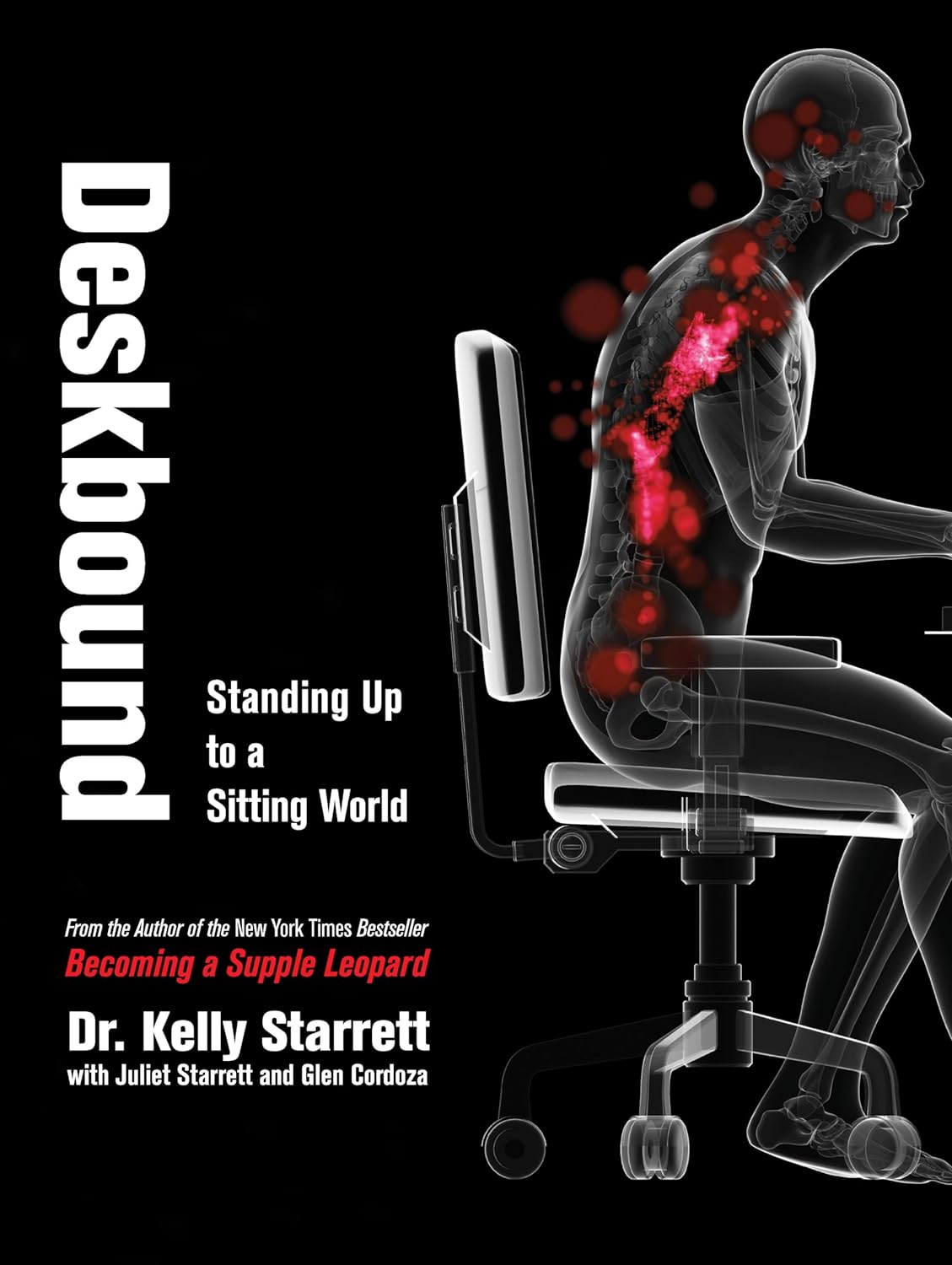
Deskbound – by Kelly Starrett and Glen Cordoza
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard that “sitting is the new smoking”, and whether or not that’s an exaggeration (the jury’s out), one thing that is clear is that sitting is very bad.
Popular advice is “here’s how to sit with good posture and stretch your neck sometimes”… but that advice tends to come from companies that pay people to sit for a long time. They might not be the a very unbiased source.
Starrett and Cordoza offer better. After one opening chapter covering the multifarious ways sitting ruins our health, the rest of the book is all advice, covering:
- The principles of how the body is supposed to be
- The most important movements that we should be doing
- A dynamic workstation setup
- This is great, because “get a standing desk” tends to present more questions than answers, and can cause as much harm as good if done wrong
- The authors also cover how to progressively cut down on sitting, rather than try to go cold-turkey.
- They also recognize that not everyone can stand at all, and…
- Optimizing the sitting position, for when we must sit
- Exercises to maintain our general mobility and compensate about as well as we can for the body-unfriendly nature of modern life.
The book is mostly explanations, so at 682 pages, you can imagine it’s not just “get up, lazybones!”. Rather, things are explained in such detail (and with many high-quality medical diagrams) so that we can truly understand them.
Most of us have gone through life knowing we should have “better posture” and “move more”… but without the details, that can be hard to execute correctly, and worse, we can even sabotage our bodies unknowingly with incorrect form.
This book straightens all that out very comprehensively, and we highly recommend it.
Share This Post
-
Ouch. That ‘Free’ Annual Checkup Might Cost You. Here’s Why.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When Kristy Uddin, 49, went in for her annual mammogram in Washington state last year, she assumed she would not incur a bill because the test is one of the many preventive measures guaranteed to be free to patients under the 2010 Affordable Care Act. The ACA’s provision made medical and economic sense, encouraging Americans to use screening tools that could nip medical problems in the bud and keep patients healthy.
So when a bill for $236 arrived, Uddin — an occupational therapist familiar with the health care industry’s workings — complained to her insurer and the hospital. She even requested an independent review.
“I’m like, ‘Tell me why am I getting this bill?’” Uddin recalled in an interview. The unsatisfying explanation: The mammogram itself was covered, per the ACA’s rules, but the fee for the equipment and the facility was not.
That answer was particularly galling, she said, because, a year earlier, her “free” mammogram at the same health system had generated a bill of about $1,000 for the radiologist’s reading. Though she fought that charge (and won), this time she threw in the towel and wrote the $236 check. But then she dashed off a submission to the KFF Health News-NPR “Bill of the Month” project:
“I was really mad — it’s ridiculous,” she later recalled. “This is not how the law is supposed to work.”
The ACA’s designers might have assumed that they had spelled out with sufficient clarity that millions of Americans would no longer have to pay for certain types of preventive care, including mammograms, colonoscopies, and recommended vaccines, in addition to doctor visits to screen for disease. But the law’s authors didn’t reckon with America’s ever-creative medical billing juggernaut.
Over the past several years, the medical industry has eroded the ACA’s guarantees, finding ways to bill patients in gray zones of the law. Patients going in for preventive care, expecting that it will be fully covered by insurance, are being blindsided by bills, big and small.
The problem comes down to deciding exactly what components of a medical encounter are covered by the ACA guarantee. For example, when do conversations between doctor and patient during an annual visit for preventive services veer into the treatment sphere? What screenings are needed for a patient’s annual visit?
A healthy 30-year-old visiting a primary care provider might get a few basic blood tests, while a 50-year-old who is overweight would merit additional screening for Type 2 diabetes.
Making matters more confusing, the annual checkup itself is guaranteed to be “no cost” for women and people age 65 and older, but the guarantee doesn’t apply for men in the 18-64 age range — though many preventive services that require a medical visit (such as checks of blood pressure or cholesterol and screens for substance abuse) are covered.
No wonder what’s covered under the umbrella of prevention can look very different to medical providers (trying to be thorough) and billers (intent on squeezing more dollars out of every medical encounter) than it does to insurers (who profit from narrower definitions).
For patients, the gray zone has become a billing minefield. Here are a few more examples, gleaned from the Bill of the Month project in just the past six months:
Peter Opaskar, 46, of Texas, went to his primary care doctor last year for his preventive care visit — as he’d done before, at no cost. This time, his insurer paid $130.81 for the visit, but he also received a perplexing bill for $111.81. Opaskar learned that he had incurred the additional charge because when his doctor asked if he had any health concerns, he mentioned that he was having digestive problems but had already made an appointment with his gastroenterologist. So, the office explained, his visit was billed as both a preventive physical and a consultation. “Next year,” Opasker said in an interview, if he’s asked about health concerns, “I’ll say ‘no,’ even if I have a gunshot wound.”
Kevin Lin, a technology specialist in Virginia in his 30s, went to a new primary care provider to take advantage of the preventive care benefit when he got insurance; he had no physical complaints. He said he was assured at check-in that he wouldn’t be charged. His insurer paid $174 for the checkup, but he was billed an additional $132.29 for a “new patient visit.” He said he has made many calls to fight the bill, so far with no luck.
Finally, there’s Yoori Lee, 46, of Minnesota, herself a colorectal surgeon, who was shocked when her first screening colonoscopy yielded a bill for $450 for a biopsy of a polyp — a bill she knew was illegal. Federal regulations issued in 2022 to clarify the matter are very clear that biopsies during screening colonoscopies are included in the no-cost promise. “I mean, the whole point of screening is to find things,” she said, stating, perhaps, the obvious.
Though these patient bills defy common sense, room for creative exploitation has been provided by the complex regulatory language surrounding the ACA. Consider this from Ellen Montz, deputy administrator and director of the Center for Consumer Information and Insurance Oversight at the Centers for Medicare & Medicaid Services, in an emailed response to queries and an interview request on this subject: “If a preventive service is not billed separately or is not tracked as individual encounter data separately from an office visit and the primary purpose of the office visit is not the delivery of the preventive item or service, then the plan issuer may impose cost sharing for the office visit.”
So, if the doctor decides that a patient’s mention of stomach pain does not fall under the umbrella of preventive care, then that aspect of the visit can be billed separately, and the patient must pay?
And then there’s this, also from Montz: “Whether a facility fee is permitted to be charged to a consumer would depend on whether the facility usage is an integral part of performing the mammogram or an integral part of any other preventive service that is required to be covered without cost sharing under federal law.”
But wait, how can you do a mammogram or colonoscopy without a facility?
Unfortunately, there is no federal enforcement mechanism to catch individual billing abuses. And agencies’ remedies are weak — simply directing insurers to reprocess claims or notifying patients they can resubmit them.
In the absence of stronger enforcement or remedies, CMS could likely curtail these practices and give patients the tools to fight back by offering the sort of clarity the agency provided a few years ago regarding polyp biopsies — spelling out more clearly what comes under the rubric of preventive care, what can be billed, and what cannot.
The stories KFF Health News and NPR receive are likely just the tip of an iceberg. And while each bill might be relatively small compared with the stunning $10,000 hospital bills that have become all too familiar in the United States, the sorry consequences are manifold. Patients pay bills they do not owe, depriving them of cash they could use elsewhere. If they can’t pay, those bills might end up with debt-collection agencies and, ultimately, harm their credit score.
Perhaps most disturbing: These unexpected bills might discourage people from seeking preventive screenings that could be lifesaving, which is why the ACA deemed them “essential health benefits” that should be free.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
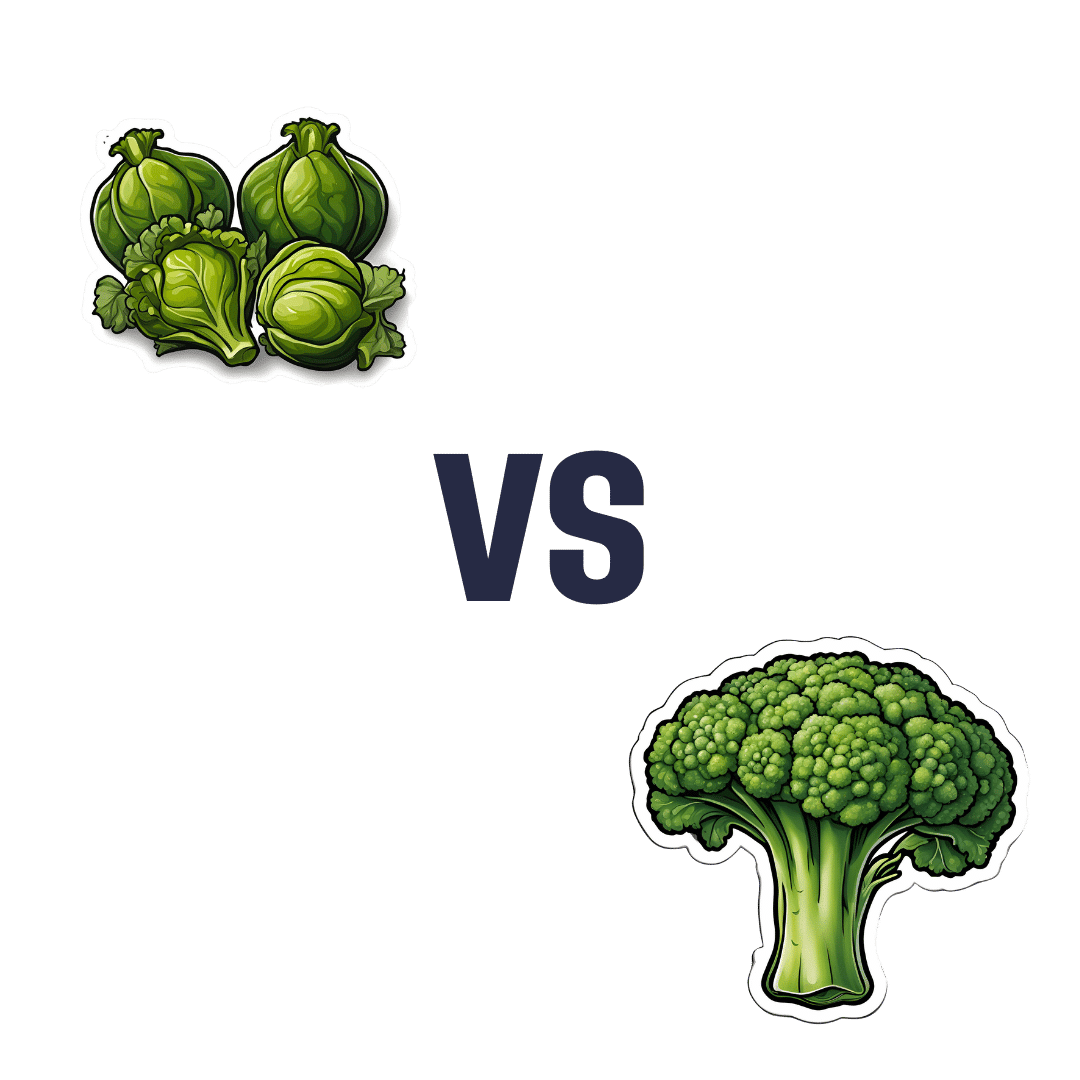
Brussels Sprouts vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sprouts to broccoli, we picked the sprouts.
Why?
First let’s note that we have an interesting comparison today, because these two plants are the exact same species (and indeed, also the exact same species as cabbage, cauliflower. and kale)—just a different cultivar. All of these plants and more are simply cultivars of Brassica oleracea.
Them being the same species notwithstanding, there are nutritional differences:
In terms of macros, sprouts have slightly more protein, carbohydrates, and fiber, whereas broccoli has slightly more water weight. An easy win for sprouts here.
In the category of vitamins, sprouts have more of vitamins A, B1, B3, B6, C, E, and K, while broccoli has more of vitamins B2 and B5. Another easy win for sprouts.
When it comes to minerals, sprouts again lead with more copper, iron, magnesium, manganese, phosphorus, and potassium, while broccoli has more calcium and selenium.
A note on oxalates: while oxalates are not a problem for most people, it is important to be mindful of them if one has kidney problems. You may know that spinach (a fellow green vegetable high in vitamins and minerals, as well as being a fellow oleracea, albeit of a different genus, so not the same species for once) is high in oxalates, but these two Brassica oleracea we compared today are amongst the lowest in oxalates (source 1 | source 2), making them an ideal way to get vitamins, minerals, and fiber on an oxalate-controlled diet.
Since both are also high in polyphenols, especially kaempferol and quercetin, we’ll mention that sprouts have more lignans while broccoli has more flavonoids. In short: they’re both very good, just different.
As ever, enjoy both! But if you’re going to pick one for total best nutritional density, it’s sprouts.
Want to learn more?
You might like to read:
Sprout Your Seeds, Grains, Beans, Etc ← sprout your Brassica oleracea, too!
Take care!
Share This Post
Related Posts
-
Supergreen Superfood Salad Slaw
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to “eating the rainbow”, in principle green should be the easiest color to get in, unless we live in a serious food desert (or serious food poverty). In practice, however, a lot of meals could do with a dash more green. This “supergreen superfood salad slaw” is remarkably versatile, and can be enjoyed as a very worthy accompaniment to almost any main.
You will need
For the bits:
- ½ small green cabbage, finely diced
- 7 oz tenderstem broccoli, finely chopped
- 2 stalks celery, finely chopped (if allergic, simply omit)
- ½ cucumber, diced into small cubes
- 2 oz kale, finely shredded
- 4 green (spring) onions, thinly sliced
For the dressing:
- 1 cup cashews (if allergic, substitute 1 cup roasted chickpeas)
- ½ cup extra virgin olive oil
- 2 oz baby spinach
- 1 oz basil leaves
- 1 oz chives
- ¼ bulb garlic
- 2 tbsp nutritional yeast
- 1 tbsp chia seeds
- Juice of two limes
Method
(we suggest you read everything at least once before doing anything)
1) Combine the ingredients from the “bits” category in a bowl large enough to accommodate them comfortably
2) Blend the ingredients from the “dressing” category in a blender until very smooth (the crux here is you do not want any stringy bits of spinach remaining)
3) Pour the dressing onto the bits, and mix well to combine. Refrigerate, ideally covered, until ready to serve.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Spinach vs Kale – Which is Healthier?
- Brain Food? The Eyes Have It!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Maximize Your Misery! (7 Great Methods)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s imagine that instead of being healthily fulfilled in life, you wanted to spend your days as miserable as possible. What should you do?
Here are a few pointers:
Stay still
Avoid physical activity and/or outdoor exposure, to avoid any mood-lifting neurochemicals. In fact, remain indoors as much as possible, preferably in the same room.
If you want to absolutely maximize your misery, make your bedroom the sole space for all activities that it’s possible to do there.
Disrupt your sleep
Keep an irregular sleep schedule by varying your bedtime and wake-up times frequently. Sleep in as much as possible, and make up for it by staying up late to ensure ongoing exhaustion.
Maximize screentime
Use digital entertainment as much as possible to distract you from meaningful activities and rest—as a bonus, this will also help you to avoid self-reflection.
Begin and end your day with a device in hand.
Fuel negative emotions
If you’re going to focus on something, focus on problems you cannot control, to stoke the fires of anger and angst.
A good way of doing this is by staying informed about distressing events, while avoiding meaningful actions to address them. Contribute only in token gestures, and then lament the lack of change.
Follow your impulses
Act on short-term desires without considering long-term consequences, while avoiding behaviors that you know might improve your mood or wellbeing.
Trust that doing the same things that have not previously resulted in happiness, will continue to reliably deliver unhappiness.
Set goals to miss
It’s important that your goals should be vague, and overly ambitious in their scope and/or deliverability. Ideally you should also disregard any preparatory work that a person would normally do before embarking on such a project.
Bonus tip: you can further sabotage any chances of progress, by waiting for motivation to strike before you take any action.
Pursue happiness
Focus on chasing happiness itself, instead of improving your situation or skills. Treat happiness as an end goal, instead of a by-product of worthwhile activities.
Want to learn more?
If you’d like to know many more ways to be miserable, we featured these 7 from this book of 40, which we haven’t reviewed yet, but probably will one of these days:
How to Be Miserable: 40 Strategies You Already Use – by Dr. Randy Paterson
Alternatively…
If for some strange reason you’d rather not do those things, you might consider a previous article of ours:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Grapefruit vs Orange – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing grapefruit to orange, we picked the orange.
Why?
It’s easy, when guessing which is the healthier out of two things, to guess that the more expensive or perhaps less universally available one is the healthier. But it’s not always so, and today is one of those cases!
In terms of macros, they are very similar fruits, with almost identical levels of carbohydrates, proteins, and fats, as well as water. Looking more carefully, we find that grapefruit’s sugars contain a slightly high proportion of fructose; not enough to make it unhealthy by any means (indeed, no whole unprocessed fruit is unhealthy unless it’s literally poisonous), but it is a thing to note if we’re micro-analysing the macronutrients. Also, oranges have slightly more fiber, which is always a plus.
When it comes to vitamins, oranges stand out with more of vitamins B1, B2, B3, B6, B9, C, and E, while grapefruit boasts more vitamin A (hence its color). Still, we’re calling this category another win for oranges.
In the category of minerals, oranges again sweep with more calcium, copper, iron, magnesium, manganese, potassium, and selenium, while grapefruit has just a little more phosphorus. So, another easy win for oranges.
One final consideration that’s not shown in the nutritional values, is that grapefruit contains furanocoumarin, which can inhibit cytochrome P-450 3A4 isoenzyme and P-glycoptrotein transporters in the intestine and liver—slowing down their drug metabolism capabilities, thus effectively increasing the bioavailability of many drugs manifold. It can also be found in lower quantities in Seville (sour) oranges, and it’s not present (or at least, if it is, it’s in truly tiny quantities) in most oranges.
This may sound superficially like a good thing (improving bioavailability of things we want), but in practice it means that in the case of many drugs, if you take them with (or near in time to) grapefruit or grapefruit juice, then congratulations, you just took an overdose. This happens with a lot of meds for blood pressure, cholesterol (including statins), calcium channel-blockers, anti-depressants, benzo-family drugs, beta-blockers, and more. Oh, and Viagra, too. Which latter might sound funny, but remember, Viagra’s mechanism of action is blood pressure modulation, and that is not something you want to mess around with unduly. So, do check with your pharmacist to know if you’re on any meds that would be affected by grapefruit or grapefruit juice!
All in all, today’s sections add up to an overwhelming win for oranges!
Want to learn more?
You might like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: