Red-dy For Anything Polyphenol Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
So, you’ve enjoyed your Supergreen Superfood Salad Slaw, and now you’re ready for another slice of the rainbow. Pigments in food aren’t just for decoration—they each contain unique benefits! Today’s focus is on some red foods that, combined, make a deliciously refreshing salad that’s great for the gut, heart, and brain.
You will need
- 1 cup crème fraîche or sour cream (if vegan, use our Plant-Based Healthy Cream Cheese recipe, and add the juice of 1 lime)
- ½ small red cabbage, thinly sliced
- 1 red apple, cored and finely chopped
- 1 red onion, thinly sliced
- 10 oz red seedless grapes, halved
- 10 oz red pomegranate seeds
- 1 tsp red chili flakes
Method
(we suggest you read everything at least once before doing anything)
1) Combine all the red ingredients in a big bowl.
2) Add the crème fraîche and mix gently but thoroughly.
3) If you have time, let it sit in the fridge for 48 hours before enjoying, as its colors will intensify and its polyphenols will become more bioavailable. But if you want/need, you can serve immediately; that’s fine too.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Resveratrol & Healthy Aging
- Tasty Polyphenols For Your Heart And Brain
- Pomegranate vs Cherries – Which is Healthier?
- Capsaicin For Weight Loss And Against Inflammation
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
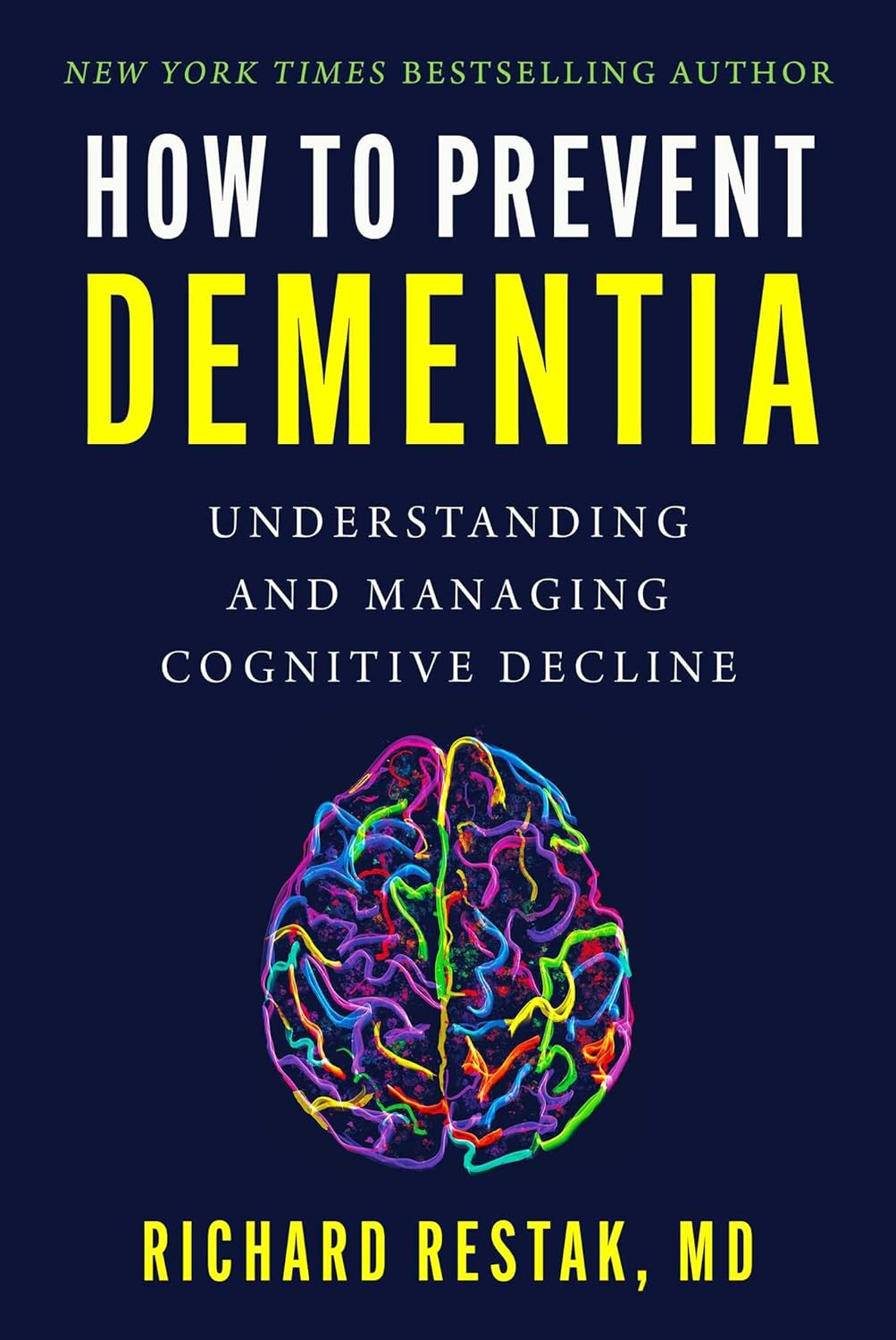
How to Prevent Dementia – by Dr. Richard Restak
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve written about this topic here, we know. But there’s a lot more we can do to be on guard against, and pre-emptively strengthen ourselves against, dementia.
The author, a neurologist, takes us on a detailed exploration of dementia in general, with a strong focus on Alzheimer’s in particular, as that accounts for more than half of all dementia cases.
But what if you can’t avoid it? It could be that with the wrong genes and some other factor(s) outside of your control, it will get you if something else doesn’t get you first.
Rather than scaremongering, Dr. Restak tackles this head-on too, and discusses how symptoms can be managed, to make the illness less anxiety-inducing, and look to maintain quality of life as much as possible.
The style of the book is… it reads a lot like an essay compilation. Good essays, then organized and arranged in a sensible order for reading, but distinct self-contained pieces. There are ten or eleven chapters (depending on how we count them), each divided into few or many sections. All this makes for:
- A very “read a bit now and a bit later and a bit the next day” book, if you like
- A feeling of a very quick pace, if you prefer to sit down and read it in one go
Either way, it’s a very informative read.
Bottom line: if you’d like to better understand the many-headed beast that is dementia, this book gives a far more comprehensive overview than we could here, and also explains the prophylactic interventions available.
Share This Post
-
The Many Health Benefits Of Garlic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Many Health Benefits of Garlic
We’re quite confident you already know what garlic is, so we’re going to leap straight in there with some science today:
First, let’s talk about allicin
Allicin is a compound in garlic that gives most of its health benefits. A downside of allicin is that it’s not very stable, so what this means is:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
- So while doing the paperwork isn’t fun, buying it as bulbs is better than buying it as granules or similar
- Allicin also breaks down somewhat in cooking, so raw garlic is best
- Our philosophy is: still use it in cooking as well; just use more!
- Supplements (capsule form etc) use typically use extracts and potency varies (from not great to actually very good)
Read more about that:
- Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts
- Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods
Now, let’s talk benefits…
Benefits to heart health
Garlic has been found to be as effective as the drug Atenolol at reducing blood pressure:
It also lowers LDL (bad cholesterol):
Benefits to the gut
We weren’t even looking for this, but as it turns out, as an add-on to the heart benefits…
Benefits to the immune system
Whether against the common cold or bringing out the heavy guns, garlic is a booster:
- Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey
- Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention
Benefits to the youthfulness of body and brain
Garlic is high in antioxidants that, by virtue of reducing oxidative stress, help slow aging. This effect, combined with the cholesterol and blood pressure benefits, means it may also reduce the risk of Alzheimer’s and other forms of dementia:
- Antioxidant health effects of aged garlic extract
- Effects of garlic consumption on plasma and erythrocyte antioxidant parameters in elderly subjects
- Garlic reduces heart disease and dementia risk
There are more benefits too…
That’s all we have time to dive into study-wise today, but for the visually-inclined, here are yet more benefits to garlic (at a rate of 3–4 cloves per day):
An incredible awesome recipe using lots of garlic:
- Take small potatoes (still in their skins), cut in half
- Add enough peeled cloves of garlic so that you have perhaps a 1:10 ratio of garlic to potato by mass
- Boil (pressure-cooking is ideal) until soft, and drain
- Keeping them in the pan, add a lashing of olive oil, and any additional seasonings per your preference (consider black pepper, rosemary, thyme, parsley)
- Put a lid on the pan, and holding it closed, shake the pan vigorously
- Note: if you didn’t leave the skins on, or you chopped much larger potatoes smaller instead of cutting in half, the potatoes will break up into a rough mash now. This is actually also fine and still tastes (and honestly, looks) great, but it is different, so just be aware, so that you get the outcome you want.
- The garlic, which—unlike the potatoes—didn’t have a skin to hold it together, will now have melted over the potatoes like butter
You can serve like this (it’s delicious already) or finish up in the oven or air-fryer or under the grill, if you prefer a roasted style dish (an amazing option too).
Share This Post
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
-
Why 7 Hours Sleep Is Not Enough
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Sleep-Deprived Are You, Really?
This is Dr. Matthew Walker. He’s a neuroscientist and sleep specialist, and is the Director of the Center for Human Sleep Science at UC Berkeley’s Department of Psychology. He’s also the author of the international bestseller “Why We Sleep”.
What does he want us to know?
Sleep deprivation is more serious than many people think it is. After about 16 hours without sleep, the brain begins to fail, and needs more than 7 hours of sleep to “reset” cognitive performance.
Note: note “seven or more”, but “more than seven”.
After ten days with only 7 hours sleep (per day), Dr. Walker points out, the brain is as dysfunctional as it would be after going without sleep for 24 hours.
Here’s the study that sparked a lot of Dr. Walker’s work:
Importantly, in Dr. Walker’s own words:
❝Three full nights of recovery sleep (i.e., more nights than a weekend) are insufficient to restore performance back to normal levels after a week of short sleeping❞
~ Dr. Matthew Walker
See also: Why You Probably Need More Sleep
Furthermore: the sleep-deprived mind is unaware of how sleep-deprived it is.
You know how a drunk person thinks they can drive safely? It’s like that.
You do not know how sleep-deprived you are, when you are sleep-deprived!
For example:
❝(60.7%) did not signal sleepiness before a sleep fragment occurred in at least one of the four MWT trials❞
Source: Sleepiness is not always perceived before falling asleep in healthy, sleep-deprived subjects
Sleep efficiency matters
With regard to the 7–9 hours band for optimal health, Dr. Walker points out that the sleep we’re getting is not always the sleep we think we’re getting:
❝Assuming you have a healthy sleep efficiency (85%), to sleep 9 hours in terms of duration (i.e. to be a long-sleeper), you would need to be consistently in bed for 10 hours and 36 minutes a night. ❞
~ Dr. Matthew Walker
At the bottom end of that, by the way, doing the same math: to get only the insufficient 7 hours sleep discussed earlier, a with a healthy 85% sleep efficiency, you’d need to be in bed for 8 hours and 14 minutes per night.
The unfortunate implication of this: if you are consistently in bed for 8 hours and 14 minutes (or under) per night, you are not getting enough sleep.
“But what if my sleep efficiency is higher than 85%?”
It shouldn’t be.If your sleep efficiency is higher than 85%, you are sleep-deprived and your body is having to enforce things.
Want to know what your sleep efficiency is?
We recommend knowing this, by the way, so you might want to check out:
Head-To-Head Comparison of Google and Apple’s Top Sleep-Monitoring Apps
(they will monitor your sleep and tell you your sleep efficiency, amongst other things)
Want to know more?
You might like his book:
Why We Sleep: Unlocking the Power of Sleep and Dreams
…and/or his podcast:
…and for those who like videos, here’s his (very informative) TED talk:
Prefer text? Click here to read the transcript
Want to watch it, but not right now? Bookmark it for later
Enjoy!
Share This Post
Related Posts
-
The Complete Anti-Inflammatory Diet for Beginners – by Dorothy Calimeris and Lulu Cook
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, about the authors: notwithstanding the names, Calimeris is the cook, and Cook is the nutritionist (and an RDN at that).
As for the book: we get a good primer on the science of inflammation, what it is, why it happens, what things are known to cause/trigger it, and what things are known to fight it. They do also go outside of nutrition a bit for this, speaking briefly on other lifestyle factors too, but the main focus is of course nutrition.
As for the recipes: while distinctly plants-forward (as one might expect of an anti-inflammatory eating book), it’s not outright vegan or even vegetarian, indeed, in the category of main dishes, there are sections for:
- Vegetarian and vegan
- Fish and shellfish
- Poultry and meat
…as well as, before and after those, sections for breakfast and brunch and snacks and sweets. As well as a not-to-be-underestimated section, for sauces, condiments, and dressings. This is important, because those are quite often the most inflammatory parts of an otherwise healthy meal! So being able to make anti-inflammatory versions is a real boon.
The recipes are mostly not illustrated, but the steps are very clearly described and easy to follow.
Bottom line: if inflammation is currently on your to-tackle list, this book will be an excellent companion in the kitchen.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Holy Basil: What Does (And Doesn’t) It Do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, a quick clarification:
- Ocimum sanctum is the botanical name given to what in English we call holy basil, and is what we will be discussing today. It’s also called “tulsi“, so if you see that name around, it is the same plant.
- Ocimum basilicum is the botanical name given to culinary basil, the kind you will find in your local supermarket. This one looks similar, but it has a different taste (culinary basil is sweeter) and a different phytochemical profile, and is certainly not the same plant.
We have touched on holy basil before, in our article:
Herbs For Evidence-Based Health & Healing
…where we listed that it helps boost immunity, per:
It’s popularly also consumed in the hopes of getting many other benefits, including:
- Calming effects on the mood (anti-stress)
- Accelerated wound-healing
- Anticancer activity
So, does it actually do those things?
Against stress
We literally couldn’t find anything. It’s often listed as being adaptogenic (reduces stress) in the preamble part of a given paper’s abstract, but we could find no study in any reputable journal that actually tested its effects against stress, and any citations for the claim just link to other papers that also include it in the preamble—and while “no original research” is a fine policy for, say, Wikipedia, it’s not a great policy when it comes to actual research science.
So… It might! There’s also no research (that we could find) showing that it doesn’t work. But one cannot claim something works on the basis of “we haven’t proved it doesn’t”.
For wound healing
Possibly! We found one (1) paper with a small (n=29) sample, and the results were promising, but that sample size of 29 was divided between three groups: a placebo control, holy basil, and another herb (which latter worked less well). So the resultant groups were tiny, arguably to the point of statistical insignificance. However, taking the study at face value and ignoring the small sample size, the results were very promising, as the holy basil group enjoyed a recovery in 4 weeks, rather than the 5 weeks recovery time of the control group:
Herbal remedies for mandibular fracture healing
An extra limitation that’s worth noting, though, is that healing bone is not necessarily the same as healing other injuries in all ways, so the same results might not be replicated in, say, organ or tissue injuries.
Against cancer
This time, there’s lots of evidence! Its mechanism of action appears to be severalfold:
- Anti-inflammatory
- Antioxidant
- Antitumor
- Chemopreventive
Because of the abundance of evidence (including specifically against skin cancer, lung cancer, breast cancer, and more), we could list studies all day here, but instead we’ll just link this one really good research review that has a handy navigation menu on the right, where you can see how it works in each of the stated ways.
Here’s the paper:
An Update on the Therapeutic Anticancer Potential of Ocimum sanctum L.: “Elixir of Life”
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pine Nuts vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pine nuts to pecans, we picked the pine nuts.
Why?
Both have their merits!
In terms of macros, pine nuts have more protein while pecans have more fiber. They’re about equal on fats, although pine nuts have more polyunsaturated fat and pecans have more monounsaturated fat, of which, both are healthy. They’re also about equal on carbs. So really it comes down to the subjective choice between prioritizing protein and prioritizing fiber. On principle, we pick fiber, which gives the win to pecans, but your preference in this regard may differ; prioritizing the protein would give the win to pine nuts.
In the category of vitamins, pine nuts have more of vitamins B2, B3, B9, E, K, and choline, while pecans have more of vitamins A, B1, B5, B6, and C. Thus, a 6:5 marginal win for pine nuts.
Looking at the minerals, pine nuts have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while pecans have more calcium and selenium. An easy win for pine nuts this time.
Adding up the sections makes for a win for pine nuts, but of course, enjoy either or (preferably) both; diversity is good!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: