The Best Menopause Advice You Don’t Want To Hear About
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nutritionist and perimenopause coach Claudia Canu, whom we’ve featured before in our Expert Insights segment, has advice:
Here’s to good health
When it comes to alcohol, the advice is: don’t.
Or at least, cut back, and manage the effects by ensuring good hydration, having an “alcohol curfew” and so forth.
What’s the relation to menopause? Well, alcohol’s not good for anyone at any time of life, but there are some special considerations when it comes to alcohol and estrogenic hormonal health:
- The liver works hard to process the alcohol as a matter of urgency, delaying estrogen processing, which can increase the risk of breast and uterine cancer.
- Alcohol has no positive health effects and is also linked to higher risks of breast and colorectal cancer.
- Alcohol can also trigger some menopausal symptoms, such as night sweats and hot flashes. So, maybe reaching for that “cooling drink” isn’t the remedy it might seem.
- During menopause, the body becomes more insulin-resistant, making it more susceptible to blood sugar spikes caused by alcohol. Also not good.
Common reasons women turn to alcohol include stress, frustration, the need for reward, and social pressure, and all of these can be heightened when undergoing hormonal changes. Yet, alcohol will ultimately only worsen each of those things.
For more on the science of some of the above, plus tips on how to make positive changes with minimum discomfort, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- How To Reduce Or Quit Alcohol
- How To Reduce The Harm Of Drinking (Without Abstaining)
- Where Nutrition Meets Habits! ← our “Expert Insights” spotlight on Canu
- How To Reduce Your Alzheimer’s Risk Early ← particularly important at this life stage
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Soba Noodle Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This Japanese dish is packed with nutrients and takes very little preparation time, involving only one cooked ingredient, and a healthy one at that!
You will need
- 8 oz dried soba noodles
- ½ bulb garlic, finely chopped
- 2 tbsp avocado oil
- 2 tsp soy sauce
- ¼ cucumber, cut into thin batons (don’t peel it first)
- ½ carrot, grated (don’t peel it first)
- 6 cherry tomatoes, halved (you wouldn’t peel these, right? Please don’t)
- ½ red onion, finely sliced (ok, this one you can peel first! Please do)
- 1 tbsp chia seeds
- 1 tsp crushed red chili flakes
- Garnish: fresh parsley, chopped
Method
(we suggest you read everything at least once before doing anything)
1) Cook the soba noodles (boil in water for 10 mins or until soft). Rinse with cold water (which lowers the glycemic index further, and also we want them cold anyway) and set aside.
2) Make the dressing by blending the garlic, avocado oil, and soy cauce. Set it aside.
3) Assemble the salad by thoroughly but gently mixing the noodles with the cucumber, carrot, tomatoes, and onion. Add the dressing, the chia seeds, and the chili flakes, and toss gently to combine.
4) Serve, adding the parsley garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Rice vs Buckwheat – Which is Healthier? ← soba noodles are made from buckwheat, which by the way is also a good source of rutin, which can strengthen blood vessel walls against damage, reducing the risk of atheroma
- Cucumber Extract Beats Glucosamine & Chondroitin… At 1/135th Of The Dose?!
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Chia: The Tiniest Seeds With The Most Value
Take care!
Share This Post
-
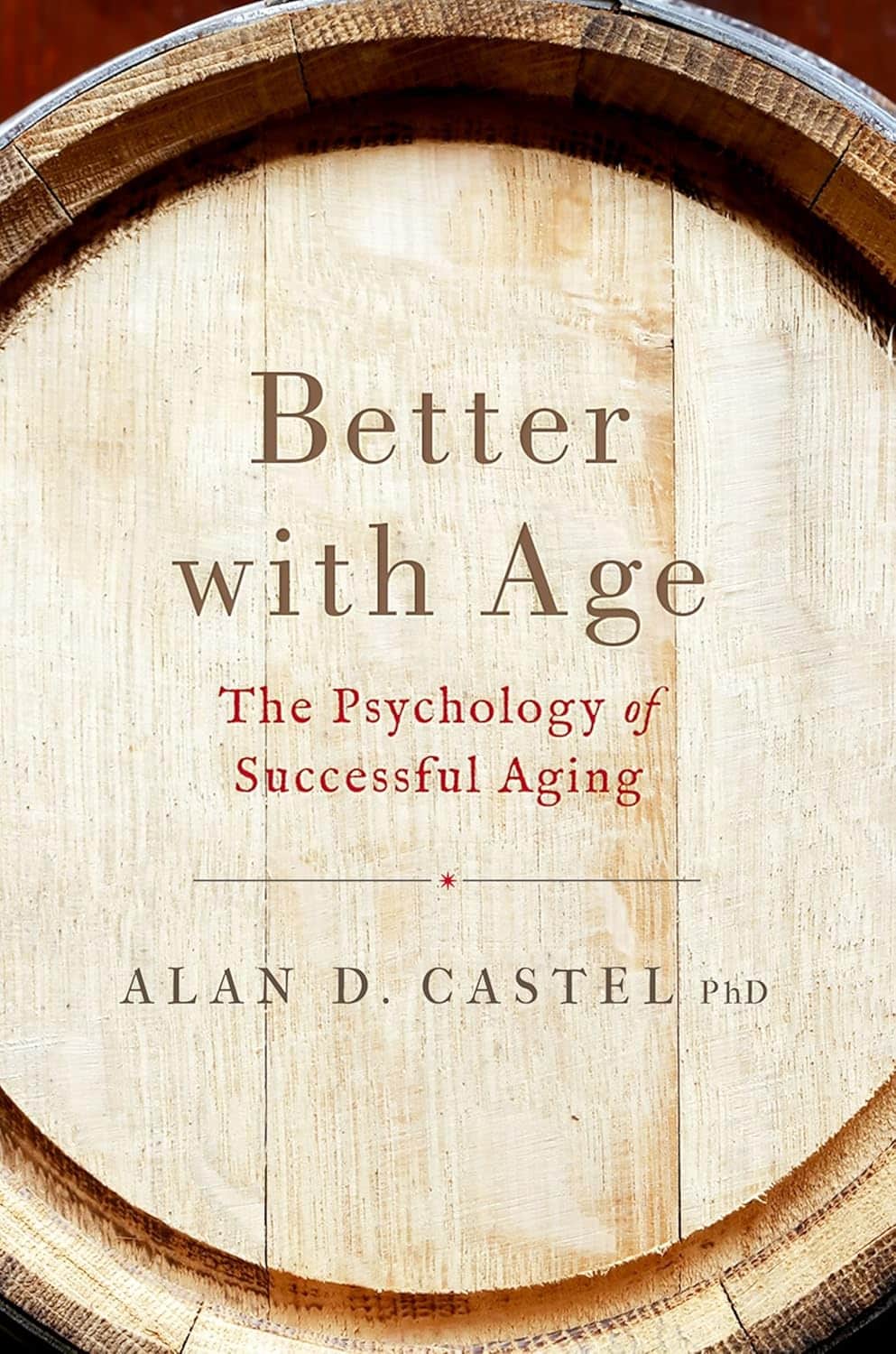
Better With Age – by Dr. Alan Castel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one isn’t about the biology of aging, so much as (as the subtitle promises) the psychology of it.
Dr. Castel first covers the grounds of what “successful aging” is, and the benefits that can be expected from doing it right. Spoiler, it’s not just “reduced decline”, there are numerous things that actually get better, too.
We also learn how our memory works differently—it can be worse, of course, but it can also be just different, in a way that tends to tie in with vastness of the accumulated knowledge over the years, allowing for easiest access to the things the brain thinks are most important—ranging from expertise in a certain field, to life-experience “wisdom”.
There’s a lot of advice that’s mostly not going to be anything new to regular readers of 10almonds, in terms of staying sharp with an active lifestyle and a well-nourished brain.
The style is very soft pop-science; there are citations dotted throughout, but mostly this is more of a “curl up with a book” book, not a textbook.
In the category of subjective criticism, it can be a little repetitive (but for those who like repetition for ease of learning, you will love this), and his name-dropping habit gets quite eyeroll-worthy quite quickly.
Bottom line: if you’d like to learn about the very many ways in which “over the hill” is simply defeatist pessimism, then this book can help you to ensure you do better.
Click here to check out Better With Age, and get better with age!
Share This Post
-
Woman Petitions Health Insurer After Company Approves — Then Rejects — Her Infusions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When KFF Health News published an article in August about the “prior authorization hell” Sally Nix said she went through to secure approval from her insurance company for the expensive monthly infusions she needs, we thought her story had a happy ending.
That’s because, after KFF Health News sent questions to Nix’s insurance company, Blue Cross Blue Shield of Illinois, it retroactively approved $36,000 worth of treatments she thought she owed. Even better, she also learned she would qualify for the infusions moving forward.
Good news all around — except it didn’t last for long. After all, this is the U.S. health care system, where even patients with good insurance aren’t guaranteed affordable care.
To recap: For more than a decade, Nix, of Statesville, North Carolina, has suffered from autoimmune diseases, chronic pain, and fatigue, as well as a condition called trigeminal neuralgia, which is marked by bouts of electric shock-like pain that’s so intense it’s commonly known as the “suicide disease.”
“It is a pain that sends me to my knees,” Nix said in October. “My entire family’s life is controlled by the betrayal of my body. We haven’t lived normally in 10 years.”
Late in 2022, Nix started receiving intravenous immunoglobulin infusions to treat her diseases. She started walking two miles a day with her service dog. She could picture herself celebrating, free from pain, at her daughter’s summer 2024 wedding.
“I was so hopeful,” she said.
But a few months after starting those infusions, she found out that her insurance company wouldn’t cover their cost anymore. That’s when she started “raising Cain about it” on Instagram and Facebook.
You probably know someone like Sally Nix — someone with a chronic or life-threatening illness whose doctor says they need a drug, procedure, or scan, and whose insurance company has replied: No.
Prior authorization was conceived decades ago to rein in health care costs by eliminating duplicative and ineffective treatment. Not only does overtreatment waste billions of dollars every year, but doctors acknowledge it also potentially harms patients.
However, critics worry that prior authorization has now become a way for health insurance companies to save money, sometimes at the expense of patients’ lives. KFF Health News has heard from hundreds of people in the past year relating their prior authorization horror stories.
When we first met Nix, she was battling her insurance company to regain authorization for her infusions. She’d been forced to pause her treatments, unable to afford $13,000 out-of-pocket for each infusion.
Finally, it seemed like months of her hard work had paid off. In July, Nix was told by staff at both her doctor’s office and her hospital that Blue Cross Blue Shield of Illinois would allow her to restart treatment. Her balance was marked “paid” and disappeared from the insurer’s online portal.
But the day after the KFF Health News story was published, Nix said, she learned the message had changed. After restarting treatment, she received a letter from the insurer saying her diagnoses didn’t actually qualify her for the infusions. It felt like health insurance whiplash.
“They’re robbing me of my life,” she said. “They’re robbing me of so much, all because of profit.”
Dave Van de Walle, a spokesperson for Blue Cross Blue Shield of Illinois, said the company would not discuss individual patients’ cases.
“Prior authorization is often a requirement for certain treatments,” Van de Walle said in a written statement, “and BCBSIL administers benefits according to medical policy and the employer’s benefit.”
But Nix is a Southern woman of the “Steel Magnolia” variety. In other words, she’s not going down without a fight.
In September, she called out her insurance company’s tactics in a http://change.org/ campaign that has garnered more than 21,000 signatures. She has also filed complaints against her insurance company with the U.S. Department of Health and Human Services, U.S. Department of Labor, Illinois Department of Insurance, and Illinois attorney general.
Even so, Nix said, she feels defeated.
Not only is she still waiting for prior authorization to restart her immunoglobulin infusions, but her insurance company recently required Nix to secure preapproval for another treatment — routine numbing injections she has received for nearly 10 years to treat the nerve pain caused by trigeminal neuralgia.
“It is reprehensible what they’re doing. But they’re not only doing it to me,” said Nix, who is now reluctantly taking prescription opioids to ease her pain. “They’re doing it to other patients. And it’s got to stop.”
Do you have an experience with prior authorization you’d like to share? Click here to tell your story.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Share This Post
Related Posts
-
Women don’t have a ‘surge’ in fertility before menopause – but surprise pregnancies can happen, even after 45
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Every now and then we see media reports about celebrities in their mid 40s having surprise pregnancies. Or you might hear stories like these from friends or relatives, or see them on TV.
Menopause signals the end of a woman’s reproductive years and happens naturally between age 45 and 55 (the average is 51). After 12 months with no periods, a woman is considered postmenopausal.
While the chance of pregnancy is very low in the years leading up to menopause – the so called menopausal transition or perimenopause – the chance is not zero.
So, what do we know about the chance of conceiving naturally after age 45? And what are the risks?
IKO-studio/Shutterstock Is there a spike in fertility before menopause?
The hormonal changes that accompany perimenopause cause changes to the menstrual cycle pattern, and some have suggested there can be a “surge” in fertility at perimenopause. But there’s no evidence this exists.
In the years leading up to menopause, a woman’s periods often become irregular, and she might have some of the common symptoms of menopause such as hot flushes and night sweats.
This might lead women to think they have hit menopause and can’t get pregnant anymore. But while pregnancy in a woman in her mid 40s is significantly less likely compared to a woman in her 20s or 30s, it’s still possible.
The stats for natural pregnancies after age 45
Although women in their mid- to late 40s sometimes have “miracle babies”, the chance of pregnancy is minimal in the five to ten years leading up to menopause.
The monthly chance of pregnancy in a woman aged 30 is about 20%. By age 40 it’s less than 5% and by age 45 the chance is negligible.
We don’t know exactly how many women become pregnant in their mid to late 40s, as many pregnancies at this age miscarry. The risk of miscarriage increases from 10% in women in their 20s to more than 50% in women aged 45 years or older. Also, for personal or medical reasons some pregnancies are terminated.
According to a review of demographic data on age when women had their final birth across several countries, the median age was 38.6 years. But the range of ages reported for last birth in the reviewed studies showed a small proportion of women give birth after age 45.
Having had many children before seems to increase the odds of giving birth after age 45. A study of 209 women in Israel who had conceived spontaneously and given birth after age 45 found 81% had already had six or more deliveries and almost half had had 11 or more previous deliveries.
Conceiving naturally at age 45 plus is not unheard of. pixelheadphoto digitalskillet/Shutterstock There’s no reliable data on how common births after age 45 are in Australia. The most recent report on births in Australia show that about 5% of babies are born to women aged 40 years or older.
However, most of those were likely born to women aged between 40 and 45. Also, the data includes women who conceive with assisted reproductive technologies, including with the use of donor eggs. For women in their 40s, using eggs donated by a younger woman significantly increases their chance of having a baby with IVF.
What to be aware of if you experience a late unexpected pregnancy
A surprise pregnancy late in life often comes as a shock and deciding what to do can be difficult.
Depending on their personal circumstances, some women decide to terminate the pregnancy. Contrary to the stereotype that abortions are most common among very young women, women aged 40–44 are more likely to have an abortion than women aged 15–19.
This may in part be explained by the fact older women are up to ten times more likely to have a fetus with chromosomal abnormalities.
There are some extra risks involved in pregnancy when the mother is older. More than half of pregnancies in women aged 45 and older end in miscarriage and some are terminated if prenatal testing shows the fetus has the wrong number of chromosomes.
This is because at that age, most eggs have chromosomal abnormalities. For example, the risk of having a pregnancy affected by Down syndrome is one in 86 at age 40 compared to one in 1,250 at age 20.
There are some added risks associated with pregnancy when the mother is older. Natalia Deriabina/Shutterstock Apart from the increased risk of chromosomal abnormalities, advanced maternal age also increases the risk of stillbirth, fetal growth restriction (when the unborn baby doesn’t grow properly), preterm birth, pre-eclampsia, gestational diabetes and caesarean section.
However, it’s important to remember that since the overall risk of all these things is small, even with an increase, the risk is still small and most babies born to older mothers are born healthy.
Multiple births are also more common in older women than in younger women. This is because older women are more likely to release more than one egg if and when they ovulate.
A study of all births in England and Wales found women aged 45 and over were the most likely to have a multiple birth.
The risks of babies being born prematurely and having health complications are higher in twin than singleton pregnancies, and the risks are highest in women of advanced maternal age.
What if you want to become pregnant in your 40s?
If you’re keen to avoid pregnancy during perimenopause, it’s recommended you use contraception.
But if you want to get pregnant in your 40s, there are some things you can do to boost your chance of conceiving and having a healthy baby.
These include preparing for pregnancy by seeing a GP for a preconception health check, taking folic acid and iodine supplements, not smoking, limiting alcohol consumption, maintaining a healthy weight, exercising regularly and having a nutritious diet.
If you get good news, talking to a doctor about what to expect and how to best manage a pregnancy in your 40s can help you be prepared and will allow you to get personalised advice based on your health and circumstances.
Karin Hammarberg, Adjunct Senior Research Fellow, Global and Women’s Health, School of Public Health & Preventive Medicine, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Most adults will gain half a kilo this year – and every year. Here’s how to stop ‘weight creep’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter a new year armed with resolutions to improve our lives, there’s a good chance we’ll also be carrying something less helpful: extra kilos. At least half a kilogram, to be precise.
“Weight creep” doesn’t have to be inevitable. Here’s what’s behind this sneaky annual occurrence and some practical steps to prevent it.
Allgo/Unsplash Small gains add up
Adults tend to gain weight progressively as they age and typically gain an average of 0.5 to 1kg every year.
While this doesn’t seem like much each year, it amounts to 5kg over a decade. The slow-but-steady nature of weight creep is why many of us won’t notice the extra weight gained until we’re in our fifties.
Why do we gain weight?
Subtle, gradual lifestyle shifts as we progress through life and age-related biological changes cause us to gain weight. Our:
- activity levels decline. Longer work hours and family commitments can see us become more sedentary and have less time for exercise, which means we burn fewer calories
- diets worsen. With frenetic work and family schedules, we sometimes turn to pre-packaged and fast foods. These processed and discretionary foods are loaded with hidden sugars, salts and unhealthy fats. A better financial position later in life can also result in more dining out, which is associated with a higher total energy intake
- sleep decreases. Busy lives and screen use can mean we don’t get enough sleep. This disturbs our body’s energy balance, increasing our feelings of hunger, triggering cravings and decreasing our energy
Insufficient sleep can increase our appetite. Craig Adderley/Pexels - stress increases. Financial, relationship and work-related stress increases our body’s production of cortisol, triggering food cravings and promoting fat storage
- metabolism slows. Around the age of 40, our muscle mass naturally declines, and our body fat starts increasing. Muscle mass helps determine our metabolic rate, so when our muscle mass decreases, our bodies start to burn fewer calories at rest.
We also tend to gain a small amount of weight during festive periods – times filled with calorie-rich foods and drinks, when exercise and sleep are often overlooked. One study of Australian adults found participants gained 0.5 kilograms on average over the Christmas/New Year period and an average of 0.25 kilograms around Easter.
Why we need to prevent weight creep
It’s important to prevent weight creep for two key reasons:
1. Weight creep resets our body’s set point
Set-point theory suggests we each have a predetermined weight or set point. Our body works to keep our weight around this set point, adjusting our biological systems to regulate how much we eat, how we store fat and expend energy.
When we gain weight, our set point resets to the new, higher weight. Our body adapts to protect this new weight, making it challenging to lose the weight we’ve gained.
But it’s also possible to lower your set point if you lose weight gradually and with an interval weight loss approach. Specifically, losing weight in small manageable chunks you can sustain – periods of weight loss, followed by periods of weight maintenance, and so on, until you achieve your goal weight.
Holidays can also come with weight gain. Zan Lazarevic/Unsplash 2. Weight creep can lead to obesity and health issues
Undetected and unmanaged weight creep can result in obesity which can increase our risk of heart disease, strokes, type 2 diabetes, osteoporosis and several types of cancers (including breast, colorectal, oesophageal, kidney, gallbladder, uterine, pancreatic and liver).
A large study examined the link between weight gain from early to middle adulthood and health outcomes later in life, following people for around 15 years. It found those who gained 2.5 to 10kg over this period had an increased incidence of type 2 diabetes, heart disease, strokes, obesity-related cancer and death compared to participants who had maintained a stable weight.
Fortunately, there are steps we can take to build lasting habits that will make weight creep a thing of the past.
7 practical steps to prevent weight creep
1. Eat from big to small
Aim to consume most of your food earlier in the day and taper your meal sizes to ensure dinner is the smallest meal you eat.
A low-calorie or small breakfast leads to increased feelings of hunger, specifically appetite for sweets, across the course of the day.
We burn the calories from a meal 2.5 times more efficiently in the morning than in the evening. So emphasising breakfast over dinner is also good for weight management.
Aim to consume bigger breakfasts and smaller dinners. Michael Burrows/Pexels 2. Use chopsticks, a teaspoon or an oyster fork
Sit at the table for dinner and use different utensils to encourage eating more slowly.
This gives your brain time to recognise and adapt to signals from your stomach telling you you’re full.
3. Eat the full rainbow
Fill your plate with vegetables and fruits of different colours first to support eating a high-fibre, nutrient-dense diet that will keep you feeling full and satisfied.
Meals also need to be balanced and include a source of protein, wholegrain carbohydrates and healthy fat to meet our dietary needs – for example, eggs on wholegrain toast with avocado.
4. Reach for nature first
Retrain your brain to rely on nature’s treats – fresh vegetables, fruit, honey, nuts and seeds. In their natural state, these foods release the same pleasure response in the brain as ultra-processed and fast foods, helping you avoid unnecessary calories, sugar, salt and unhealthy fats.
5. Choose to move
Look for ways to incorporate incidental activity into your daily routine – such as taking the stairs instead of the lift – and boost your exercise by challenging yourself to try a new activity.
Just be sure to include variety, as doing the same activities every day often results in boredom and avoidance.
Try new activities or sports to keep your interest up. Cottonbro Studio/Pexels 6. Prioritise sleep
Set yourself a goal of getting a minimum of seven hours of uninterrupted sleep each night, and help yourself achieve it by avoiding screens for an hour or two before bed.
7. Weigh yourself regularly
Getting into the habit of weighing yourself weekly is a guaranteed way to help avoid the kilos creeping up on us. Aim to weigh yourself on the same day, at the same time and in the same environment each week and use the best quality scales you can afford.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Clinical Trials Director, Department of Endocrinology, RPA Hospital, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Age of Scientific Wellness – by Dr. Leroy Hood & Dr. Nathan Price
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t usually do an author bio beyond mentioning their professional background, but in this case it’s worth mentioning that the first-listed author, Dr. Leroy Hood, is the one who invented the automated gene sequencing technology that made the Human Genome Project possible. In terms of awards, he’s won everything short of a Nobel Prize, and that’s probably less a snub and more a matter of how there isn’t a Nobel Prize for Engineering—his field is molecular biotechnology, but what he solved was an engineering problem.
In this book, the authors set out to make the case that “find it and fix it” medicine has done a respectable job of getting us where we are, but what we need now is P4 medicine:
- Predict
- Prevent
- Personalize
- Participate
The idea is that with adequate data (genomic, phenomic, and digital), we can predict the course of health sufficiently well to interrupt the process of disease at its actual (previously unseen) starting point, instead of waiting for symptoms to show up, thus preventing it proactively. The personalization is because this will not be a “one size fits all” approach, since our physiologies are different, our markers of health and disease will be somewhat too. And the participatory aspect? That’s because the only way to get enough data to do this for an entire population is with—more or less—an entire population’s involvement.
This is what happens when, for example, your fitness tracker asks if it can share anonymized health metrics for research purposes and you allow it—you are becoming part of the science (a noble and worthy act!).
You may be wondering whether this book has health advice, or is more about the big picture. And, the answer is both. It’s mostly about the big picture but it does have a lot of (data-driven!) health advice too, especially towards the end.
The style is largely narrative, talking the reader through the progresses (and setbacks) that have marked the path so far, and projecting the next part of the journey, in the hope that we can avoid being part of a generation born just too late to take advantage of this revolutionary approach to health.
Bottom line: this isn’t a very light read, but it is a worthwhile one, and it’ll surely inspire you to increase the extent to which you are proactive about your health!
Click here to check out The Age Of Scientific Wellness, and be part of it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: