What you need to know about FLiRT, an emerging group of COVID-19 variants
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What you need to know
- COVID-19 wastewater levels are currently low, but a recent group of variants called FLiRT is making headlines.
- KP.2 is one of several FLiRT variants, and early lab tests suggest that it’s more infectious than JN.1.
- Getting infected with any COVID-19 variant can cause severe illness, heart problems, and death.
KP.2, a new COVID-19 variant, is now dominant in the United States. Lab tests suggest that it may be more infectious than JN.1, the variant that was dominant earlier this year.
Fortunately, there’s good news: Current wastewater data shows that COVID-19 infection rates are low. Still, experts are closely watching KP.2 to see if it will lead to an uptick in infections.
Read on to learn more about KP.2 and how to stay informed about COVID-19 cases in your area.
Where can I find data on COVID-19 cases in my area?
Hospitals are no longer required to report COVID-19 hospital admissions or hospital capacity to the Department of Health and Human Services. However, wastewater-based epidemiology (WBE) estimates the number of COVID-19 infections in a community based on the amount of COVID-19 viral particles detected in local wastewater.
View this map of wastewater data from the CDC to visualize COVID-19 infection rates throughout the U.S., or look up COVID-19 wastewater trends in your state.
What do we know so far about the new variant?
Early lab tests suggest that KP.2—one of a group of emerging variants called FLiRT—is similar to the previously dominant variant, JN.1, but it may be more infectious. If you had JN.1, you may still get reinfected with KP.2, especially if it’s been several months or longer since your last COVID-19 infection.
A CDC spokesperson said they have no reason to believe that KP.2 causes more severe illness than other variants. Experts are closely watching KP.2 to see if it will lead to an uptick in COVID-19 cases.
How can I protect myself from COVID-19 variants?
Staying up to date on COVID-19 vaccines reduces your risk of severe illness, long COVID, heart problems, and death. The CDC recommends that people 65 and older and immunocompromised people receive an additional dose of the updated COVID-19 vaccine this spring.
Wearing a high-quality, well-fitting mask reduces your risk of contracting COVID-19 and spreading it to others. At indoor gatherings, improving ventilation by opening doors and windows, using high-efficiency particulate air (HEPA) filters, and building your own Corsi-Rosenthal box can also reduce the spread of COVID-19.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dietary Changes for Artery Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝How does your diet change clean out your arteries of the bad cholesterol?❞
There’s good news and bad news here, and they can both be delivered with a one-word reply:
Slowly.
Or rather: what’s being cleaned out is mostly not the LDL (bad) cholesterol, but rather, the result of that.
When our diet is bad for cardiovascular health, our arteries get fatty deposits on their walls. Cholesterol gets stuck here too, but that’s not the main physical problem.
Our body’s natural defenses come into action and try to clean it up, but they (for example macrophages, a kind of white blood cell that consumes invaders and then dies, before being recycled by the next part of the system) often get stuck and become part of the buildup (called atheroma), which can lead to atherosclerosis and (if calcium levels are high) hardening of the arteries, which is the worst end of this.
This can then require medical attention, precisely because the body can’t remove it very well—especially if you are still maintaining a heart-unhealthy diet, thus continuing to add to the mess.
However, if it is not too bad yet, yes, a dietary change alone will reverse this process. Without new material being added to the arterial walls, the body’s continual process of rejuvenation will eventually fix it, given time (free from things making it worse) and resources.
In fact, your arteries can be one of the quickest places for your body to make something better or worse, because the blood is the means by which the body moves most things (good or bad) around the body.
All the more reason to take extra care of it, since everything else depends on it!
You might also like our previous main feature:
Share This Post
-
What Happens To Your Body When You Plank 1 Minute Every Day
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Planks improve strength, flexibility, balance, posture, reduce chronic back pain, lower blood pressure, and enhance physique. But can we really get benefits from just 1 minute per day?
To the core
The benefits that can be expected, according to the science cited in this video, include:
- Within 2–3 weeks, daily planking of just 1 minute per day activates deep core muscles, enhancing balance, which helps in everyday tasks and prevents muscle imbalances.
- Strengthening core muscles through planks also helps alleviate lower back pain, with research supporting its effectiveness within 3 weeks.
- Posture is important for good health, and planks align the spine and hips, improving posture naturally, which also helps alleviate back issues. So, there’s a good kind of synergy to this exercise.
- Of course, many people exercising have the goal of a more toned body; regular planking leads to a toned core, sculpted shoulders, and leaner legs.
- For those who care more about mobility, though, planking enhances flexibility in hamstrings, feet, and toes within 4–6 weeks.
- Anything else? Yes, isometric exercises like planks are highly effective at reducing blood pressure, and, counterintuitively, more so than aerobic exercises.
The video also looks at a study in which participants did 20 minutes per day instead of 1, which predictably also significantly improved strength, endurance, flexibility, and reduced body fat.
However, another study cited gives the stats for just 1 minute daily, and that was not even a whole minute, so much as 30 seconds hold, 1 minute rest, 30 seconds hold—and still showed very good improvements.
For more on all this, plus links to three studies mentioned in the video, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Isometric Exercises That Are Good If You Have Osteoporosis (or if you don’t, but the point is, they are safe and beneficial for people with osteoporosis)
Take care!
Share This Post
-
How To Engage Your Whole Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Stroke Of Insight That Nobody Wants
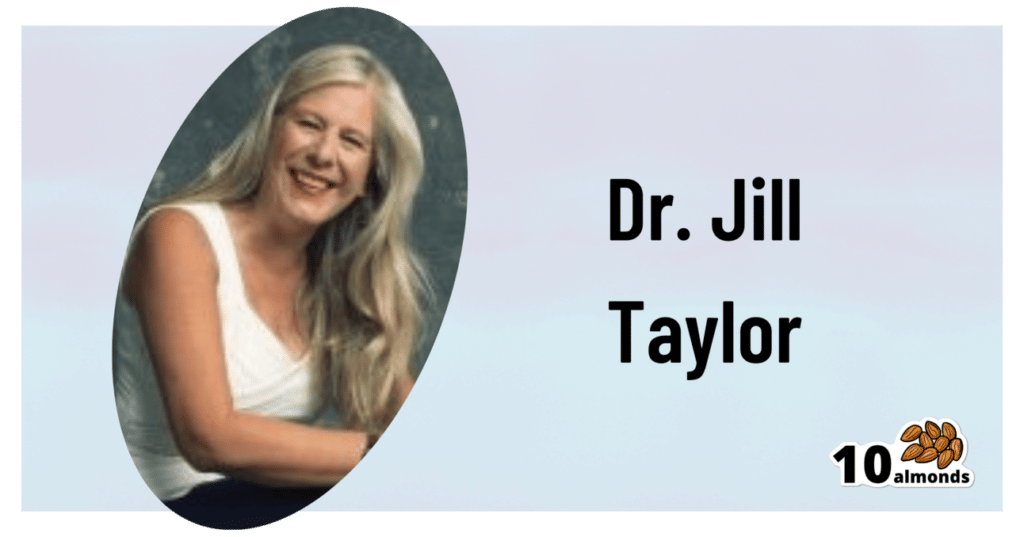
This is Dr. Jill Bolte Taylor. She’s a neuroanatomist, who, at the age of 37 (when she was a post-doctoral fellow at Harvard Medical School), had what she refers to as her “stroke of insight”.
That is to say, she had a massive stroke, and after a major brain surgery to remove a clot the size of a golf ball, she spent the next 8 years re-learning to do everything.
Whereas previously she’d been busy mapping the brain to determine how cells communicate with each other, now she was busy mapping whether socks or shoes should go on first. Needless to say, she got an insight into neuroplasticity that few people would hope for.
What does she want us to know?
Dr. Taylor (now once again a successful scientist, lecturer, and author) advocates for “whole brain living”, which involves not taking parts of our brain for granted.
About those parts…
Dr. Taylor wants us to pay attention to all the parts regardless of size, ranging from the two hemispheres, all the way down to the billions of brain cells, and yet even further, to the “trillions of molecular geniuses”—because each brain cell is itself reliant on countless molecules of the many neurochemicals that make up our brain.
For a quick refresher on some of the key players in that latter category, see our Neurotransmitter Cheatsheet 😎
When it comes to the hemispheres, there has historically been a popular belief that these re divided into:
- The right brain: emotional, imaginative, creative, fluid feeling
- The left brain: intellectual, analytical, calculating, crystal thinking
…which is not true, anatomically speaking, because there are cells on both sides doing their part of both of these broad categories of brain processes.
However, Dr. Taylor found, while one hemisphere of her brain was much more damaged than the other, that nevertheless she could recover some functions more quickly than others, which, once she was able to resume her career, inspired her model of four distinct ways of cogitating that can be switched-between and played with or against each other:
Meet The Four Characters Inside Your Brain
Why this matters
As she was re-learning everything, the way forward was not quick or easy, and she also didn’t know where she was going, because for obvious reasons, she couldn’t remember, much less plan.
Looking backwards after her eventual full recovery, she noted a lot of things that she needed during that recovery, some of which she got and some of which she didn’t.
Most notably for her, she needed the right kind of support that would allow all four of the above “characters” as she puts it, to thrive and grow. And, when we say “grow” here we mean that literally, because of growing new brain cells to replace the lost ones (as well as the simple ongoing process of slowly replacing brain cells).
For more on growing new brain cells, by the way, see:
How To Grow New Brain Cells (At Any Age)
In order to achieve this in all of the required brain areas (i.e., and all of the required brain functions), she also wants us to know… drumroll please…
When to STFU
Specifically, the ability to silence parts of our brain that while useful in general, aren’t necessarily being useful right now. Since it’s very difficult to actively achieve a negative when it comes to brain-stuff (don’t think of an elephant), this means scheduling time for other parts of our brain to be louder. And that includes:
- scheduling time to feel (emotionally)
- scheduling time to feel (gut feelings)
- scheduling time to feel (kinesthetically)
…amongst others.
Note: those three are presented in that order, from least basic to most basic. And why? Because, clever beings that we are, we typically start from a position that’s not remotely basic, such as “overthinking”, for example. So, there’s a wind-down through thinking just the right amount, thinking through simpler concepts, feeling, noticing one’s feelings, noticing noticing one’s feelings, all the way down to what, kinesthetically, are we actually physically feeling.
❝It is interesting to note that although our limbic system fucntions throughout our lifetime, it does not mature. As a result, when our emotional “buttons” are pushed, we retain the ability to react to incoming stimulation as though we were a two-year-old, even when we are adults.❞
~ Dr. Jill Taylor
Of course, sometimes the above is not useful, which is why the ability to switch between brain modes is a very important and useful skill to develop.
And how do we do that? By practising. Which is something that it’s necessary to take up consciously, and pursue consistently. When children are at school, there are (hopefully, ideally) curricula set out to ensure they engage and train all parts of their brain. As adults, this does not tend to get the same amount of focus.
“Children’s brains are still developing”—indeed, and so are adult brains:
The Brain As A Work-In-Progress
Dr. Taylor had the uncommon experience of having to, in many ways, neurologically speaking, redo childhood. And having had a second run at it, she developed an appreciation of the process that most of us didn’t necessarily get when doing childhood just the once.
In other words: take the time to feel stuff; take the time to quiet down your chatty mind, take the time engage your senses, and take it seriously! Really notice, as though for the first time, what the texture of your carpet is like. Really notice, as though for the first time, what it feels like to swallow some water. Really notice, as though for the first time, what it feels like to experience joy—or sadness, or comfort, or anger, or peace. Exercise your imagination. Make some art (it doesn’t have to win awards; it just has to light up your brain!). Make music (again, it’s about wiring your brain in your body, not about outdoing Mozart in composition and/or performance). Make changes! Make your brain work in the ways it’s not in the habit of doing.
If you need a little help switching off parts of your brain that are being too active, so that you can better exercise other parts of your brain that might otherwise have been neglected, you might want to try:
Enjoy!
Share This Post
Related Posts
-
Brain Health Action Plan – by Dr. Teryn Clarke
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is a physician and neurologist, and she brings a lot of science with her when she sets out to Alzheimer’s-proof our brains:
- She talks about brain nourishment, and what things in contrast sabotage our brains, and how.
- She talks intermittent fasting, and optimal scheduling when it comes to food, sleep, exercise, and more.
- She talks about how the rest of our health affects our brain health, and vice versa.
The “action plan” promised by the title includes all of those elements, plus such matters as ongoing education, cognitive stimulation, stress management, dealing with depression, and other mostly-brain-based factors.
As such, it’s not just a “for your information” book, and Dr. Clarke does outline suggested goals, tasks, and habits, advises the use of a streak tracker, provides suggested recipes, and in all ways does what she can to make it easy for the reader to implement the information within.
Bottom line: if you’d like to dodge dementia, this book is quite a comprehensive guide.
Click here to check out Brain Health Action Plan, and enact yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Viruses aren’t always harmful. 6 ways they’re used in health care and pest control
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We tend to just think of viruses in terms of their damaging impacts on human health and lives. The 1918 flu pandemic killed around 50 million people. Smallpox claimed 30% of those who caught it, and survivors were often scarred and blinded. More recently, we’re all too familiar with the health and economic impacts of COVID.
But viruses can also be used to benefit human health, agriculture and the environment.
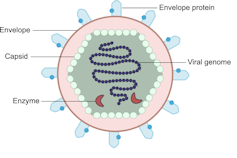
Viruses are comparatively simple in structure, consisting of a piece of genetic material (RNA or DNA) enclosed in a protein coat (the capsid). Some also have an outer envelope.
Viruses get into your cells and use your cell machinery to copy themselves.
Here are six ways we’ve harnessed this for health care and pest control.1. To correct genes
Viruses are used in some gene therapies to correct malfunctioning genes. Genes are DNA sequences that code for a particular protein required for cell function.
If we remove viral genetic material from the capsid (protein coat) we can use the space to transport a “cargo” into cells. These modified viruses are called “viral vectors”.
Viruses consist of a piece of RNA or DNA enclosed in a protein coat called the capsid.
DEXiViral vectors can deliver a functional gene into someone with a genetic disorder whose own gene is not working properly.
Some genetic diseases treated this way include haemophilia, sickle cell disease and beta thalassaemia.
2. Treat cancer
Viral vectors can be used to treat cancer.
Healthy people have p53, a tumour-suppressor gene. About half of cancers are associated with the loss of p53.
Replacing the damaged p53 gene using a viral vector stops the cancerous cell from replicating and tells it to suicide (apoptosis).
Viral vectors can also be used to deliver an inactive drug to a tumour, where it is then activated to kill the tumour cell.
This targeted therapy reduces the side effects otherwise seen with cytotoxic (cell-killing) drugs.
We can also use oncolytic (cancer cell-destroying) viruses to treat some types of cancer.
Tumour cells have often lost their antiviral defences. In the case of melanoma, a modified herpes simplex virus can kill rapidly dividing melanoma cells while largely leaving non-tumour cells alone.
3. Create immune responses
Viral vectors can create a protective immune response to a particular viral antigen.
One COVID vaccine uses a modified chimp adenovirus (adenoviruses cause the common cold in humans) to transport RNA coding for the SARS-CoV-2 spike protein into human cells.
The RNA is then used to make spike protein copies, which stimulate our immune cells to replicate and “remember” the spike protein.
Then, when you are exposed to SARS-CoV-2 for real, your immune system can churn out lots of antibodies and virus-killing cells very quickly to prevent or reduce the severity of infection.
4. Act as vaccines
Viruses can be modified to act directly as vaccines themselves in several ways.
We can weaken a virus (for an attenuated virus vaccine) so it doesn’t cause infection in a healthy host but can still replicate to stimulate the immune response. The chickenpox vaccine works like this.
The Salk vaccine for polio uses a whole virus that has been inactivated (so it can’t cause disease).
Others use a small part of the virus such as a capsid protein to stimulate an immune response (subunit vaccines).
An mRNA vaccine packages up viral RNA for a specific protein that will stimulate an immune response.
5. Kill bacteria
Viruses can – in limited situations in Australia – be used to treat antibiotic-resistant bacterial infections.
Bacteriophages are viruses that kill bacteria. Each type of phage usually infects a particular species of bacteria.
Unlike antibiotics – which often kill “good” bacteria along with the disease-causing ones – phage therapy leaves your normal flora (useful microbes) intact.
Bacteriophages (red) are viruses that kill bacteria (green).
Shutterstock6. Target plant, fungal or animal pests
Viruses can be species-specific (infecting one species only) and even cell-specific (infecting one type of cell only).
This occurs because the proteins viruses use to attach to cells have a shape that binds to a specific type of cell receptor or molecule, like a specific key fits a lock.
The virus can enter the cells of all species with this receptor/molecule. For example, rabies virus can infect all mammals because we share the right receptor, and mammals have other characteristics that allow infection to occur whereas other non-mammal species don’t.
When the receptor is only found on one cell type, then the virus will infect that cell type, which may only be found in one or a limited number of species. Hepatitis B virus successfully infects liver cells primarily in humans and chimps.
We can use that property of specificity to target invasive plant species (reducing the need for chemical herbicides) and pest insects (reducing the need for chemical insecticides). Baculoviruses, for example, are used to control caterpillars.
Similarly, bacteriophages can be used to control bacterial tomato and grapevine diseases.
Other viruses reduce plant damage from fungal pests.
Myxoma virus and calicivirus reduce rabbit populations and their environmental impacts and improve agricultural production.
Just like humans can be protected against by vaccination, plants can be “immunised” against a disease-causing virus by being exposed to a milder version.
Thea van de Mortel, Professor, Nursing, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
An Unexpected Extra Threat Of Alcohol
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If You Could Use Some Exotic Booze…
…then for health reasons, we’re going to have to say “nay”.
We’ve written about alcohol before, and needless to say, it’s not good:
(the answer is “no, we cannot”)
In fact, the WHO (which unlike government regulatory bodies setting “safe” limits on drinking, makes no profit from taxes on alcohol sales) has declared that “the only safe amount of alcohol is zero”:
WHO: No level of alcohol consumption is safe for our health
Up there, where the air is rarefied…
If you’re flying somewhere this summer (Sinatra-style flying honeymoon or otherwise), you might want to skip the alcohol even if you normally do imbibe, because:
❝…even in young and healthy individuals, the combination of alcohol intake with sleeping under hypobaric conditions poses a considerable strain on the cardiac system and might lead to exacerbation of symptoms in patients with cardiac or pulmonary diseases.
These effects might be even greater in older people; cardiovascular symptoms have a prevalence of 7% of inflight medical emergencies, with cardiac arrest causing 58% of aircraft diversions.❞
Source: Alcohol plus cabin pressure at higher altitude may threaten sleeping plane passengers’ heart health
The experiment divided subjects into a control group and a study group; the study group were placed in simulated cabin pressure as though at altitude, which found, when giving some of them two small(we’re talking the kind given on flights) alcoholic drinks:
❝The combination of alcohol and simulated cabin pressure at cruising altitude prompted a fall in SpO2 to an average of just over 85% and a compensatory increase in heart rate to an average of nearly 88 beats/minute during sleep.❞
In contrast, that was 77 beats/minute for those who had alcohol but weren’t at altitude pressure, or 64 beats/minute for those who neither drank nor were at altitude pressure.
Lots more metrics were recorded and the study is interesting to read; if you’ve ever slept on a plane and thought “that sleep was not restful at all”, then know: it wasn’t just the seat’s fault, nor the engine, nor the recycled nature of the air—it was the reduced pressure causing hypoxia (defined as having oxygen levels lower than the healthy clinical norm of 90%) and almost halving your sleep’s effectiveness for a less than 10% drop in available oxygen in the blood (the sleepers not at altitude pressure averaged 96% SpO2, compared to the 85% at altitude).
We say “almost halving” because the deep sleep phase of sleep was reduced from 84 minutes (control) to 67.5 minutes at altitude without alcohol, or 46.5 minutes at altitude with alcohol.
Again, this was a pressure cabin in a lab—so this wasn’t about the other conditions of an airplane (seats, engine hundreds of other people, etc).
Which means: in an actual airplane it’s probably even worse.
Oh, and the study participants? All healthy individuals aged 18–40, so again probably worse for those older (or younger) than that range, or with existing health conditions!
Want to know more?
You can read the study in full here:
Want to drop the drink at any altitude? Check out:
Want to get that vacation feel without alcohol? You’re going to love:
Mocktails – by Moira Clark (book)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: