Terminal lucidity: why do loved ones with dementia sometimes ‘come back’ before death?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is often described as “the long goodbye”. Although the person is still alive, dementia slowly and irreversibly chips away at their memories and the qualities that make someone “them”.
Dementia eventually takes away the person’s ability to communicate, eat and drink on their own, understand where they are, and recognise family members.
Since as early as the 19th century, stories from loved ones, caregivers and health-care workers have described some people with dementia suddenly becoming lucid. They have described the person engaging in meaningful conversation, sharing memories that were assumed to have been lost, making jokes, and even requesting meals.
It is estimated 43% of people who experience this brief lucidity die within 24 hours, and 84% within a week.
Why does this happen?
Terminal lucidity or paradoxical lucidity?
In 2009, researchers Michael Nahm and Bruce Greyson coined the term “terminal lucidity”, since these lucid episodes often occurred shortly before death.
But not all lucid episodes indicate death is imminent. One study found many people with advanced dementia will show brief glimmers of their old selves more than six months before death.
Lucidity has also been reported in other conditions that affect the brain or thinking skills, such as meningitis, schizophrenia, and in people with brain tumours or who have sustained a brain injury.
Moments of lucidity that do not necessarily indicate death are sometimes called paradoxical lucidity. It is considered paradoxical as it defies the expected course of neurodegenerative diseases such as dementia.
But it’s important to note these episodes of lucidity are temporary and sadly do not represent a reversal of neurodegenerative disease.

Why does terminal lucidity happen?
Scientists have struggled to explain why terminal lucidity happens. Some episodes of lucidity have been reported to occur in the presence of loved ones. Others have reported that music can sometimes improve lucidity. But many episodes of lucidity do not have a distinct trigger.
A research team from New York University speculated that changes in brain activity before death may cause terminal lucidity. But this doesn’t fully explain why people suddenly recover abilities that were assumed to be lost.
Paradoxical and terminal lucidity are also very difficult to study. Not everyone with advanced dementia will experience episodes of lucidity before death. Lucid episodes are also unpredictable and typically occur without a particular trigger.
And as terminal lucidity can be a joyous time for those who witness the episode, it would be unethical for scientists to use that time to conduct their research. At the time of death, it’s also difficult for scientists to interview caregivers about any lucid moments that may have occurred.
Explanations for terminal lucidity extend beyond science. These moments of mental clarity may be a way for the dying person to say final goodbyes, gain closure before death, and reconnect with family and friends. Some believe episodes of terminal lucidity are representative of the person connecting with an afterlife.
Why is it important to know about terminal lucidity?
People can have a variety of reactions to seeing terminal lucidity in a person with advanced dementia. While some will experience it as being peaceful and bittersweet, others may find it deeply confusing and upsetting. There may also be an urge to modify care plans and request lifesaving measures for the dying person.
Being aware of terminal lucidity can help loved ones understand it is part of the dying process, acknowledge the person with dementia will not recover, and allow them to make the most of the time they have with the lucid person.
For those who witness it, terminal lucidity can be a final, precious opportunity to reconnect with the person that existed before dementia took hold and the “long goodbye” began.
Yen Ying Lim, Associate Professor, Turner Institute for Brain and Mental Health, Monash University and Diny Thomson, PhD (Clinical Neuropsychology) Candidate and Provisional Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Avoid Carer Burnout (Without Dropping Care)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Avoid Carer Burnout
Sometimes in life we find ourselves in a caregiving role.
Maybe we chose it. For example, by becoming a professional carer, or even just by being a parent.
Oftentimes we didn’t. Sometimes because our own parents now need care from us, or because a partner becomes disabled.
Philosophical note: an argument could be made for that latter also having been a pre-emptive choice; we probably at some point said words to the effect of “in sickness and in health”, hopefully with free will, and hopefully meant it. And of course, sometimes we enter into a relationship with someone who is already disabled.
But, we are not a philosophy publication, and will henceforth keep to the practicalities.
First: are you the right person?
Sometimes, a caregiving role might fall upon you unasked-for, and it’s worth considering whether you are really up for it. Are you in a position to be that caregiver? Do you want to be that caregiver?
It may be that you do, and would actively fight off anyone or anything that tried to stop you. If so, great, now you only need to make sure that you are actually in a position to provide the care in question.
It may be that you do want to, but your circumstances don’t allow you to do as good a job of it as you’d like, or it means you have to drop other responsibilities, or you need extra help. We’ll cover these things later.
It may be that you don’t want to, but you feel obliged, or “have to”. If that’s the case, it will be better for everyone if you acknowledge that, and find someone else to do it. Nobody wants to feel a burden, and nobody wants someone providing care to be resentful of that. The result of such is two people being miserable; that’s not good for anyone. Better to give the job to someone who actually wants to (a professional, if necessary).
So, be honest (first with yourself, then with whoever may be necessary) about your own preferences and situation, and take steps to ensure you’re only in a caregiving role that you have the means and the will to provide.
Second: are you out of your depth?
Some people have had a life that’s prepared them for being a carer. Maybe they worked in the caring profession, maybe they have always been the family caregiver for one reason or another.
Yet, even if that describes you… Sometimes someone’s care needs may be beyond your abilities. After all, not all care needs are equal, and someone’s condition can (and more often than not, will) deteriorate.
So, learn. Learn about the person’s condition(s), medications, medical equipment, etc. If you can, take courses and such. The more you invest in your own development in this regard, the more easily you will handle the care, and the less it will take out of you.
And, don’t be afraid to ask for help. Maybe the person knows their condition better than you, and certainly there’s a good chance they know their care needs best. And certainly, there are always professionals that can be contacted to ask for advice.
Sometimes, a team effort may be required, and there’s no shame in that either. Whether it means enlisting help from family/friends or professionals, sometimes “many hands make light work”.
Check out: Caregiver Action Network: Organizations Near Me
A very good resource-hub for help, advice, & community
Third: put your own oxygen mask on first
Like the advice to put on one’s own oxygen mask first before helping others (in the event of a cabin depressurization in an airplane), the rationale is the same here. You can’t help others if you are running on empty yourself.
As a carer, sometimes you may have to put someone else’s needs above yours, both in general and in the moment. But, you do have needs too, and cannot neglect them (for long).
One sleepless night looking after someone else is… a small sacrifice for a loved one, perhaps. But several in a row starts to become unsustainable.
Sometimes it will be necessary to do the best you can, and accept that you cannot do everything all the time.
There’s a saying amongst engineers that applies here too: “if you don’t schedule time for maintenance, your equipment will schedule it for you”.
In other words: if you don’t give your body rest, your body will break down and oblige you to rest. Please be aware this goes for mental effort too; your brain is just another organ.
So, plan ahead, schedule breaks, find someone to take over, set up your cared-for-person with the resources to care for themself as well as possible (do this anyway, of course—independence is generally good so far as it’s possible), and make the time/effort to get you what you need for you. Sleep, distraction, a change of scenery, whatever it may be.
Lastly: what if it’s you?
If you’re reading this and you’re the person who has the higher care needs, then firstly:all strength to you. You have the hardest job here; let’s not forget that.
About that independence: well-intentioned people may forget that, so don’t be afraid to remind them when “I would prefer to do that myself”. Maintaining independence is generally good for the health, even if sometimes it is more work for all concerned than someone else doing it for you. The goal, after all, is your wellbeing, so this shouldn’t be cast aside lightly.
On the flipside: you don’t have to be strong all the time; nobody should.
Being disabled can also be quite isolating (this is probably not a revelation to you), so if you can find community with other people with the same or similar condition(s), even if it’s just online, that can go a very, very long way to making things easier. Both practically, in terms of sharing tips, and psychologically, in terms of just not feeling alone.
See also: How To Beat Loneliness & Isolation
Share This Post
-
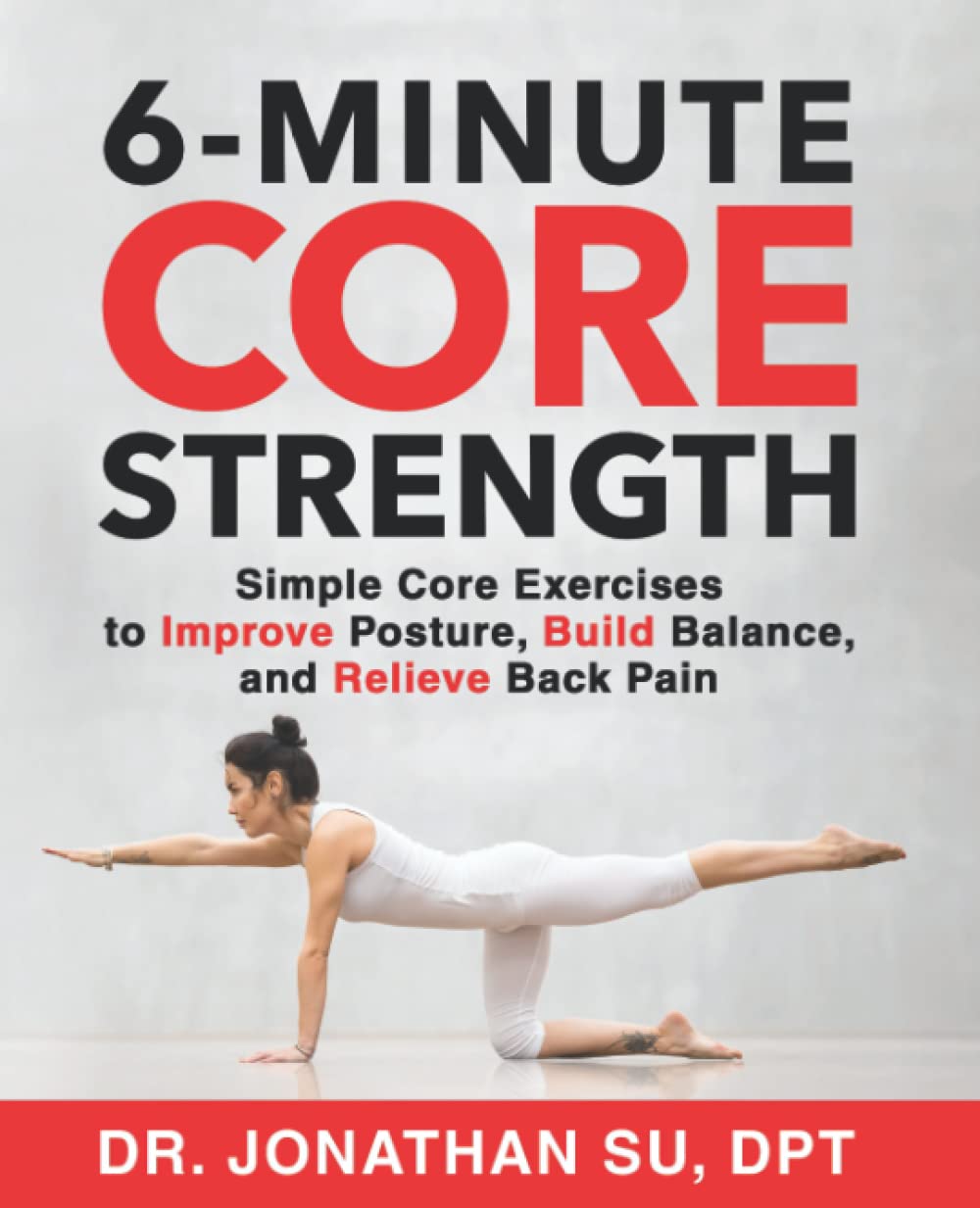
6-Minute Core Strength – by Dr. Jonathan Su
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We don’t normally do author biographies here, but in this case it’s worth noting that Dr. Su is a physiotherapist, military rehab expert, and an IAYT yoga therapist. So, these things together certainly do lend weight to his advice.
About the “6-minute” thing: this is in the style of the famous “7-minute workout” and “5 Minutes’ Physical Fitness” etc, and refers to how long each exercise session should take. The baseline is one such session per day, though of course doing more than one set of 6 minutes each time is a bonus if you wish to do so.
The exercises are focused on core strength, but they also include hip and shoulder exercises, since these are after all attached to the core, and hip and shoulder mobility counts for a lot.
A particular strength of the book is in troubleshooting mistakes of the kind that aren’t necessarily visible from photos; in this case, Dr. Su explains what you need to go for in a certain exercise, and how to know if you are doing it correctly. This alone is worth the cost of the book, in this reviewer’s opinion.
Bottom line: if you want core strength and want it simple yet comprehensive, this book can guide you.
Click here to check out 6-Minute Core Strength, and strengthen yours!
Share This Post
-
‘Sleep tourism’ promises the trip of your dreams. Beyond the hype plus 5 tips for a holiday at home
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Imagine arriving at your hotel after a long flight and being greeted by your own personal sleep butler. They present you with a pillow menu and invite you to a sleep meditation session later that day.
You unpack in a room kitted with an AI-powered smart bed, blackout shades, blue light-blocking glasses and weighted blankets.
Holidays are traditionally for activities or sightseeing – eating Parisian pastry under the Eiffel tower, ice skating at New York City’s Rockefeller Centre, lying by the pool in Bali or sipping limoncello in Sicily. But “sleep tourism” offers vacations for the sole purpose of getting good sleep.
The emerging trend extends out of the global wellness tourism industry – reportedly worth more than US$800 billion globally (A$1.2 trillion) and expected to boom.
Luxurious sleep retreats and sleep suites at hotels are popping up all over the world for tourists to get some much-needed rest, relaxation and recovery. But do you really need to leave home for some shuteye?
RossHelen/Shutterstock Not getting enough
The rise of sleep tourism may be a sign of just how chronically sleep deprived we all are.
In Australia more than one-third of adults are not achieving the recommended 7–9 hours of sleep per night, and the estimated cost of this inadequate sleep is A$45 billion each year.
Inadequate sleep is linked to long-term health problems including poor mental health, heart disease, metabolic disease and deaths from any cause.
Can a fancy hotel give you a better sleep?
Many of the sleep services available in the sleep tourism industry aim to optimise the bedroom for sleep. This is a core component of sleep hygiene – a series of healthy sleep practices that facilitate good sleep including sleeping in a comfortable bedroom with a good mattress and pillow, sleeping in a quiet environment and relaxing before bed.
The more people follow sleep hygiene practices, the better their sleep quality and quantity.
When we are staying in a hotel we are also likely away from any stressors we encounter in everyday life (such as work pressure or caring responsibilities). And we’re away from potential nighttime disruptions to sleep we might experience at home (the construction work next door, restless pets, unsettled children). So regardless of the sleep features hotels offer, it is likely we will experience improved sleep when we are away.
Being away from home also means being away from domestic disruptions. Makistock/Shutterstock What the science says about catching up on sleep
In the short-term, we can catch up on sleep. This can happen, for example, after a short night of sleep when our brain accumulates “sleep pressure”. This term describes how strong the biological drive for sleep is. More sleep pressure makes it easier to sleep the next night and to sleep for longer.
But while a longer sleep the next night can relieve the sleep pressure, it does not reverse the effects of the short sleep on our brain and body. Every night’s sleep is important for our body to recover and for our brain to process the events of that day. Spending a holiday “catching up” on sleep could help you feel more rested, but it is not a substitute for prioritising regular healthy sleep at home.
All good things, including holidays, must come to an end. Unfortunately the perks of sleep tourism may end too.
Our bodies do not like variability in the time of day that we sleep. The most common example of this is called “social jet lag”, where weekday sleep (getting up early to get to work or school) is vastly different to weekend sleep (late nights and sleep ins). This can result in a sleepy, grouchy start to the week on Monday. Sleep tourism may be similar, if you do not come back home with the intention to prioritise sleep.
So we should be mindful that as well as sleeping well on holiday, it is important to optimise conditions at home to get consistent, adequate sleep every night.
Good sleep hygiene doesn’t require a passport. Maridav/Shutterstock 5 tips for having a sleep holiday at home
An AI-powered mattress and a sleep butler at home might be the dream. But these features are not the only way we can optimise our sleep environment and give ourselves the best chance to get a good night’s sleep. Here are five ideas to start the night right:
1. avoid bright artificial light in the evening (such as bright overhead lights, phones, laptops)
2. make your bed as comfortable as possible with fresh pillows and a supportive mattress
3. use black-out window coverings and maintain a cool room temperature for the ideal sleeping environment
4. establish an evening wind-down routine, such as a warm shower and reading a book before bed or even a “sleepy girl mocktail”
5. use consistency as the key to a good sleep routine. Aim for a similar bedtime and wake time – even on weekends.
Charlotte Gupta, Senior postdoctoral research fellow, Appleton Institute, HealthWise research group, CQUniversity Australia and Dean J. Miller, Adjunct Research Fellow, Appleton Institute of Behavioural Science, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Are You Stuck Playing These Three Roles in Love?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The psychology of Transactional Analysis holds that our interpersonal dynamics can be modelled in the following fashion:
The roles
- Child: vulnerable, trusting, weak, and support-seeking
- Parent: strong, dominant, responsible—but also often exhausted and critical
- Adult: balanced, thoughtful, creative, and kind
Ideally we’d be able to spend most of our time in “Adult” mode, and occasionally go into “Child” or “Parent” mode when required, e.g. child when circumstances have rendered us vulnerable and we need help; parent when we need to go “above and beyond” in the pursuit of looking after others. That’s all well and good and healthy.
However, in relationships, often it happens that partners polarize themselves and/or each other, with one shouldering all of the responsibility, and the other willfully losing their own agency.
The problem lies in that either role can be seductive—on the one hand, it’s nice to be admired and powerful and it’s a good feeling to look after one’s partner; on the other hand, it’s nice to have someone who will meet your every need. What love and trust!
Only, it becomes toxic when these roles stagnate, and each forgets how to step out of them. Each can become resentful of the other (for not pulling their weight, on one side, and for not being able to effortlessly solve all life problems unilaterally and provide endlessly in both time and substance, on the other), digging in to their own side and exacerbating the less healthy qualities.
As to the way out? It’s about self-exploration and mutual honesty—and mutual support:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
While we haven’t (before today) written about TA per se, we have previously written about AT (Attachment Theory), and on this matter, the two can overlap, where certain attachment styles can result in recreating parent/child/adult dynamics:
How To Leverage Attachment Theory In Your Relationship ← this is about understanding and recognizing attachment styles, and then making sure that both you and your partner(s) are armed with the necessary knowledge and understanding to meet each other’s needs.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Broccoli Pesto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cruciferous vegetables have many health benefits of their own (especially: a lot of anticancer benefits). But, it can be hard to include them in every day’s menu, so this is just one more way that’ll broaden your options! It’s delicious mixed into pasta, or served as a dip, or even on toast.
You will need
- 4 cups small broccoli florets
- 1 cup fresh basil leaves
- ½ cup pine nuts
- ¼ bulb garlic
- 3 tbsp extra virgin olive oil
- 2 tbsp nutritional yeast
- 1 tbsp lemon juice
- 2 tsp black pepper, coarse ground
- 1 tsp red pepper flakes
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Steam the broccoli for 3–5 minutes. Allow to cool.
2) Blend the pine nuts, garlic, lemon juice, and nutritional yeast.
3) Add the broccoli, basil, olive oil, black pepper, red pepper, and MSG or salt, and blend in the food processor again until well-combined.
4) Serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Broccoli vs Cauliflower – Which is Healthier?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Herbs for (Evidence-Based) Health & Healing ← Basil features here! It’s easy to think that medicinal herbs have to be some kind of arcane obscurity, but it’s often not so.
- Our Top 5 Spices: How Much Is Enough For Benefits? ← Black pepper, red pepper, and garlic all feature here
- All About Olive Oil: Is “Extra Virgin” Worth It?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Self-Compassion In A Relationship (Positives & Pitfalls)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Practise Self-Compassion In Your Relationship (But Watch Out!)
Let’s make clear up-front: this is not about “…but not too much”.
With that in mind…
Now let’s set the scene: you, a happily-partnered person, have inadvertently erred and upset your partner. They may or may not have already forgiven you, but you are still angry at yourself.
Likely next steps include all or any of:
- continuing to apologise and try to explain
- self-deprecatory diatribes
- self-flagellation, probably not literally but in the sense of “I don’t deserve…” and acting on that feeling
- self-removal, because you don’t want to further inflict your bad self on your partner
As you might guess, these are quite varied in their degree of healthiness:
- apologising is good, as even is explaining, but once it’s done, it’s done; let it go
- self-deprecation is pretty much never useful, let alone healthy
- self-flagellation likewise; it is not only inherently self-destructive, but will likely create an additional problem for your partner too
- self-removal can be good or bad depending on the manner of that removal: there’s a difference between just going cold and distant on your partner, and saying “I’m sorry; this is my fault not yours, I don’t want to take it out on you, so please give me half an hour by myself to regain my composure, and I will come back with love then if that’s ok with you”
About that last: mentioning the specific timeframe e.g. “half an hour” is critical, by the way—don’t leave your partner hanging! And then do also follow through on that; come back with love after the half-hour elapses. We suggest mindfulness meditation in the interim (here’s our guide to how), if you’re not sure what to do to get you there.
To Err Is Human; To Forgive, Healthy (Here’s How To Do It) ← this goes for when the forgiveness in question is for yourself, too—and we do write about that there (and how)!
This is important, by the way; not forgiving yourself can cause more serious issues down the line:
If, by the way, you’re hand-wringing over “but was my apology good enough really, or should I…” then here is how to do it. Basically, do this, and then draw a line under it and consider it done:
The Apology Checklist ← you’ll want to keep a copy of this, perhaps in the notes app on your phone, or a screenshot if you prefer
(the checklist is at the bottom of that page)
The catch
It’s you, you’re the catch 👈👈😎
Ok, that being said, there is actually a catch in the less cheery sense of the word, and it is:
“It is important to be compassionate about one’s occasional failings in a relationship” does not mean “It is healthy to be neglectful of one’s partner’s emotional needs; that’s self-care, looking after #1; let them take care of themself too”
…because that’s simply not being a couple at all.
Think about it this way: the famous airline advice,
“Put on your own oxygen mask before helping others with theirs”
…does not mean “Put on your own oxygen mask and then watch those kids suffocate; it’s everyone for themself”
So, the same goes in relationships too. And, as ever, we have science for this. There was a recent (2024) study, involving hundreds of heterosexual couples aged 18–73, which looked at two things, each measured with a scaled questionnaire:
- Subjective levels of self-compassion
- Subjective levels of relationship satisfaction
For example, questions included asking participants to rate, from 1–5 depending on how much they felt the statements described them, e.g:
In my relationship with my partner, I:
- treat myself kindly when I experience sorrow and suffering.
- accept my faults and weaknesses.
- try to see my mistakes as part of human nature.
- see difficulties as part of every relationship that everyone goes through once.
- try to get a balanced view of the situation when something unpleasant happens.
- try to keep my feelings in balance when something upsets me.
Note: that’s not multiple choice! It’s asking participants to rate each response as applicable or not to them, on a scale of 1–5.
And…
❝Women’s self-compassion was also positively linked with men’s total relationship satisfaction. Thus, men seem to experience overall satisfaction with the relationship when their female partner is self-kind and self-caring in difficult situations.
Unexpectedly, however, we found that men’s relationship-specific self-compassion was negatively associated with women’s fulfillment.
Baker and McNulty (2011) reported that, only for men, a Self-Compassion x Conscientiousness interaction explained whether the positive effects of self-compassion on the relationship emerged, but such an interaction was not found for women.
Highly self-compassionate men who were low in conscientiousness were less motivated than others to remedy interpersonal mistakes in their romantic relationships, and this tendency was in turn related to lower relationship satisfaction❞
~ Dr. Astrid Schütz et al. (2024)
And if you’d like to read the cited older paper from 2011, here it is:
Read in full: Self-compassion and relationship maintenance: the moderating roles of conscientiousness and gender
The take-away here is not: “men should not practice self-compassion”
(rather, they absolutely should)
The take-away is: we must each take responsibility for managing our own mood as best we are able; practice self-forgiveness where applicable and forgive our partner where applicable (and communicate that!)…. And then go consciously back to the mutual care on which the relationship is hopefully founded.
Which doesn’t just mean love-bombing, by the way, it also means listening:
The Problem With Active Listening (And How To Do Better)
To close… We say this often, but we mean it every time: take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: