How Useful Is Peppermint, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Peppermint For Digestion & Against Nausea
Peppermint is often enjoyed to aid digestion, and sometimes as a remedy for nausea, but what does the science say about these uses?
Peppermint and digestion
In short: it works! (but beware)
Most studies on peppermint and digestion, that have been conducted with humans, have been with regard to IBS, but its efficacy seems quite broad:
❝Peppermint oil is a natural product which affects physiology throughout the gastrointestinal tract, has been used successfully for several clinical disorders, and appears to have a good safety profile.❞
However, and this is important: if your digestive problem is GERD, then you may want to skip it:
❝The univariate logistic regression analysis showed the following risk factors: eating 1–2 meals per day (OR = 3.50, 95% CI: 1.75–6.98), everyday consumption of peppermint tea (OR = 2.00, 95% CI: 1.14–3.50), and eating one, big meal in the evening instead of dinner and supper (OR = 1.80, 95% CI: 1.05–3.11).
The multivariate analysis confirmed that frequent peppermint tea consumption was a risk factor (OR = 2.00, 95% CI: 1.08–3.70).❞
~ Dr. Jarosz & Dr. Taraszewska
Source: Risk factors for gastroesophageal reflux disease: the role of diet
Peppermint and nausea
Peppermint is also sometimes recommended as a nausea remedy. Does it work?
The answer is: maybe
The thing with nausea is it is a symptom with a lot of possible causes, so effectiveness of remedies may vary. But for example:
- Aromatherapy for treatment of postoperative nausea and vomiting ← no better than placebo
- The Effect of Combined Inhalation Aromatherapy with Lemon and Peppermint on Nausea and Vomiting of Pregnancy: A Double-Blind, Randomized Clinical Trial ← initially no better than placebo, then performed better on subsequent days
- The Effects of Peppermint Oil on Nausea, Vomiting and Retching in Cancer Patients Undergoing Chemotherapy: An Open Label Quasi-Randomized Controlled Pilot Study ← significant benefit immediately
Summary
Peppermint is useful against wide variety of gastrointestinal disorders, including IBS, but very definitely excluding GERD (in the case of GERD, it may make things worse)
Peppermint may help with nausea, depending on the cause.
Where can I get some?
Peppermint tea, and peppermint oil, you can probably find in your local supermarket (as well as fresh mint leaves, perhaps).
For the “heavy guns” that is peppermint essential oil, here’s an example product on Amazon for your convenience
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The CBT Workbook for Mental Health – by Dr. Simon Rego & Sarah Fader
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have often reviewed psychology books here with a note saying “and no, it’s not just a book of the standard CBT techniques that you probably already know”.
So today, this one’s for anyone who was ever thinking “but I don’t know the standard CBT techniques and I would like to know them!”.
The authors outline specific solutions to many common quantifiable problems, with simple exercises that are well-explained and easy to implement.
Cognitive Behavioral Therapy (CBT) is not a panacea, but for the things it can be used for, it’s very effective and is a very good “first thing to reach for” to see if it works, because its success rate for a lot of problems is very high.
What kinds of things is this book most likely to help with? A lot of common forms of stress, anxiety, self-esteem issues, cravings, shame, and relationship issues. Other things too, but we can’t list everything and that list already covers a lot of very high-incidence stuff.
Bottom line: if CBT isn’t something already in your toolbox, this book will help you add all its best tips and tricks.
Click here to check out The CBT Workbook for Mental Health, and get tooled up!
Share This Post
-
Dealing With Waking Up In The Night
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I’m now in my sixties and find that I invariably wake up at least once during the night. Is this normal? Even if it is, I would still like, once in a while, to sleep right through like a teenager. How might this be achieved, without pills?❞
Most people wake up briefly between sleep cycles, and forget doing so. But waking up for more than a brief moment is indeed best avoided. In men of your age, if you’re waking to pee (especially if it’s then not actually that easy to pee), it can be a sign of an enlarged prostate. Which is again a) normal b) not optimal.
By “without pills” we’ll assume you mean “without sleeping pills”. There are options to treat an enlarged prostate, including well-established supplements. We did a main feature on this:
Prostate Health: What You Should Know
If the cause of waking up is something else, then again this is common for everyone as we get older, and again it’s not optimal. But since there are so many possible causes (and thus solutions), it’s more than we can cover in less than a main feature, so we’ll have to revisit this later.
Meanwhile, take care!
Share This Post
-
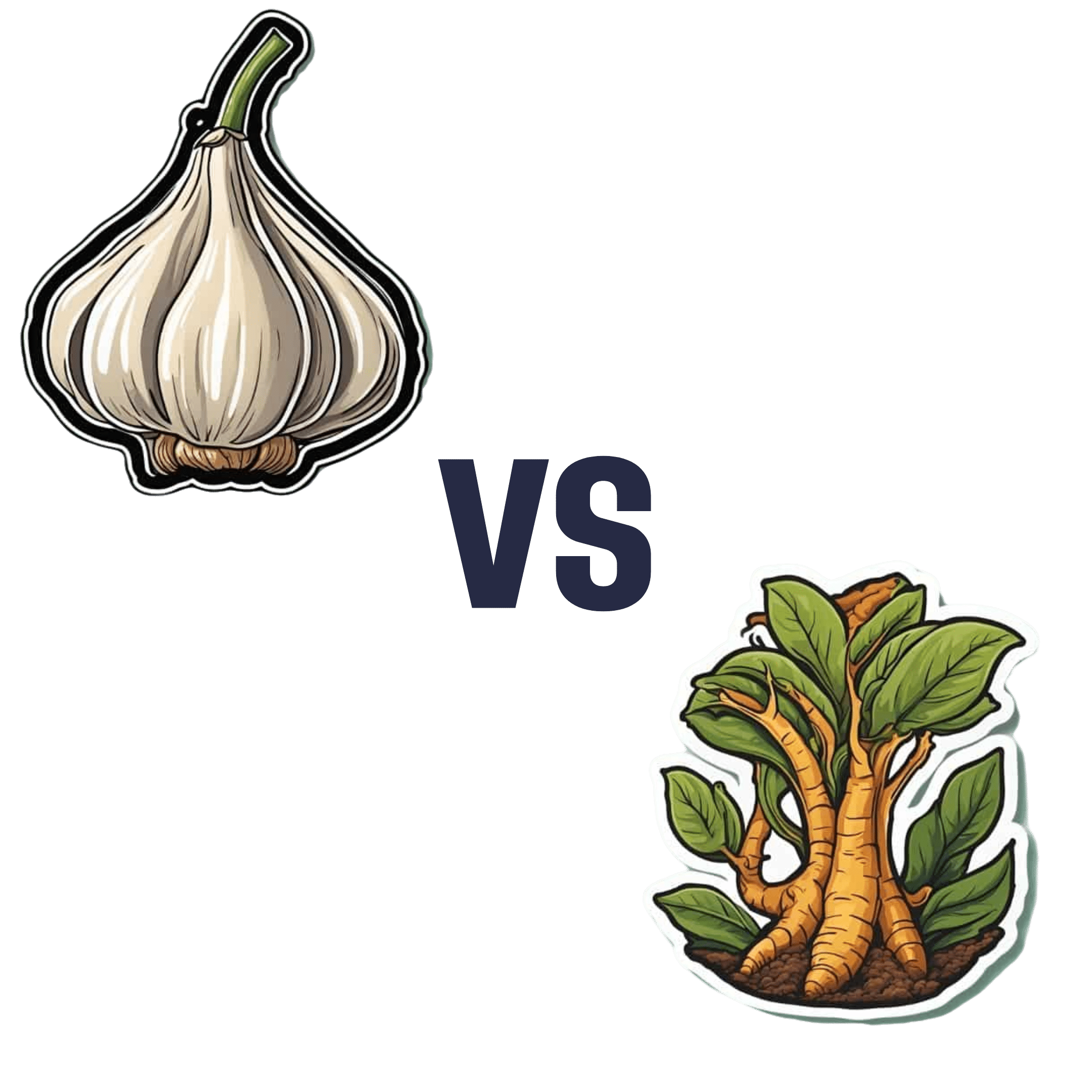
Garlic vs Ginger – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing garlic to ginger, we picked the ginger.
Why?
Both are great, and it is close!
Notwithstanding that (almost?) nobody eats garlic or ginger for the macros, let’s do a moment’s due diligence on that first: garlic has more than 3x the protein and about 2x the fiber (and slightly higher carbs). But, given the small quantities in which people usually consume these foods, these numbers aren’t too meaningful.
In the category of micronutrients, garlic has a lot more vitamins and minerals. We’ll not do a full breakdown for this though, because again, unless you’re eating it by the cupful, this won’t make a huge difference.
Which means that so far, we have two nominal wins for garlic.
Both plants have many medicinal properties. They are both cardioprotective and anticancer, and both full of antioxidants. The benefits of both are comparable in these regards.
Both have antidiabetic action also, but ginger’s effects are stronger when compared head-to head.
So that’s an actual practical win for ginger.
Each plant’s respective effects on the gastrointestinal tract sets them further apart—ginger has antiemetic effects and can be used for treating nausea and vomiting from a variety of causes. Garlic, meanwhile, can cause adverse gastrointestinal effects in some people—but it’s usually neutral for most people in this regard.
Another win for ginger in practical terms.
Want to learn more?
You might like to read:
Take care!
Share This Post
Related Posts
-
Yes, blue light from your phone can harm your skin. A dermatologist explains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Social media is full of claims that everyday habits can harm your skin. It’s also full of recommendations or advertisements for products that can protect you.
Now social media has blue light from our devices in its sights.
So can scrolling on our phones really damage your skin? And will applying creams or lotions help?
Here’s what the evidence says and what we should really be focusing on.
Max kegfire/Shutterstock Remind me, what actually is blue light?
Blue light is part of the visible light spectrum. Sunlight is the strongest source. But our electronic devices – such as our phones, laptops and TVs – also emit it, albeit at levels 100-1,000 times lower.
Seeing as we spend so much time using these devices, there has been some concern about the impact of blue light on our health, including on our eyes and sleep.
Now, we’re learning more about the impact of blue light on our skin.
How does blue light affect the skin?
The evidence for blue light’s impact on skin is still emerging. But there are some interesting findings.
1. Blue light can increase pigmentation
Studies suggest exposure to blue light can stimulate production of melanin, the natural skin pigment that gives skin its colour.
So too much blue light can potentially worsen hyperpigmentation – overproduction of melanin leading to dark spots on the skin – especially in people with darker skin.
Blue light can worsen dark spots on the skin caused by overproduction of melanin. DUANGJAN J/Shutterstock 2. Blue light can give you wrinkles
Some research suggests blue light might damage collagen, a protein essential for skin structure, potentially accelerating the formation of wrinkles.
A laboratory study suggests this can happen if you hold your device one centimetre from your skin for as little as an hour.
However, for most people, if you hold your device more than 10cm away from your skin, that would reduce your exposure 100-fold. So this is much less likely to be significant.
3. Blue light can disrupt your sleep, affecting your skin
If the skin around your eyes looks dull or puffy, it’s easy to blame this directly on blue light. But as we know blue light affects sleep, what you’re probably seeing are some of the visible signs of sleep deprivation.
We know blue light is particularly good at suppressing production of melatonin. This natural hormone normally signals to our bodies when it’s time for sleep and helps regulate our sleep-wake cycle.
By suppressing melatonin, blue light exposure before bed disrupts this natural process, making it harder to fall asleep and potentially reducing the quality of your sleep.
The stimulating nature of screen content further disrupts sleep. Social media feeds, news articles, video games, or even work emails can keep our brains active and alert, hindering the transition into a sleep state.
Long-term sleep problems can also worsen existing skin conditions, such as acne, eczema and rosacea.
Sleep deprivation can elevate cortisol levels, a stress hormone that breaks down collagen, the protein responsible for skin’s firmness. Lack of sleep can also weaken the skin’s natural barrier, making it more susceptible to environmental damage and dryness.
Can skincare protect me?
The beauty industry has capitalised on concerns about blue light and offers a range of protective products such as mists, serums and lip glosses.
From a practical perspective, probably only those with the more troublesome hyperpigmentation known as melasma need to be concerned about blue light from devices.
This condition requires the skin to be well protected from all visible light at all times. The only products that are totally effective are those that block all light, namely mineral-based suncreens or some cosmetics. If you can’t see the skin through them they are going to be effective.
But there is a lack of rigorous testing for non-opaque products outside laboratories. This makes it difficult to assess if they work and if it’s worth adding them to your skincare routine.
What can I do to minimise blue light then?
Here are some simple steps you can take to minimise your exposure to blue light, especially at night when it can disrupt your sleep:
- use the “night mode” setting on your device or use a blue-light filter app to reduce your exposure to blue light in the evening
- minimise screen time before bed and create a relaxing bedtime routine to avoid the types of sleep disturbances that can affect the health of your skin
- hold your phone or device away from your skin to minimise exposure to blue light
- use sunscreen. Mineral and physical sunscreens containing titanium dioxide and iron oxides offer broad protection, including from blue light.
In a nutshell
Blue light exposure has been linked with some skin concerns, particularly pigmentation for people with darker skin. However, research is ongoing.
While skincare to protect against blue light shows promise, more testing is needed to determine if it works.
For now, prioritise good sun protection with a broad-spectrum sunscreen, which not only protects against UV, but also light.
Michael Freeman, Associate Professor of Dermatology, Bond University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Federal Panel Prescribes New Mental Health Strategy To Curb Maternal Deaths
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BRIDGEPORT, Conn. — Milagros Aquino was trying to find a new place to live and had been struggling to get used to new foods after she moved to Bridgeport from Peru with her husband and young son in 2023.
When Aquino, now 31, got pregnant in May 2023, “instantly everything got so much worse than before,” she said. “I was so sad and lying in bed all day. I was really lost and just surviving.”
Aquino has lots of company.
Perinatal depression affects as many as 20% of women in the United States during pregnancy, the postpartum period, or both, according to studies. In some states, anxiety or depression afflicts nearly a quarter of new mothers or pregnant women.
Many women in the U.S. go untreated because there is no widely deployed system to screen for mental illness in mothers, despite widespread recommendations to do so. Experts say the lack of screening has driven higher rates of mental illness, suicide, and drug overdoses that are now the leading causes of death in the first year after a woman gives birth.
“This is a systemic issue, a medical issue, and a human rights issue,” said Lindsay R. Standeven, a perinatal psychiatrist and the clinical and education director of the Johns Hopkins Reproductive Mental Health Center.
Standeven said the root causes of the problem include racial and socioeconomic disparities in maternal care and a lack of support systems for new mothers. She also pointed a finger at a shortage of mental health professionals, insufficient maternal mental health training for providers, and insufficient reimbursement for mental health services. Finally, Standeven said, the problem is exacerbated by the absence of national maternity leave policies, and the access to weapons.
Those factors helped drive a 105% increase in postpartum depression from 2010 to 2021, according to the American Journal of Obstetrics & Gynecology.
For Aquino, it wasn’t until the last weeks of her pregnancy, when she signed up for acupuncture to relieve her stress, that a social worker helped her get care through the Emme Coalition, which connects girls and women with financial help, mental health counseling services, and other resources.
Mothers diagnosed with perinatal depression or anxiety during or after pregnancy are at about three times the risk of suicidal behavior and six times the risk of suicide compared with mothers without a mood disorder, according to recent U.S. and international studies in JAMA Network Open and The BMJ.
The toll of the maternal mental health crisis is particularly acute in rural communities that have become maternity care deserts, as small hospitals close their labor and delivery units because of plummeting birth rates, or because of financial or staffing issues.
This week, the Maternal Mental Health Task Force — co-led by the Office on Women’s Health and the Substance Abuse and Mental Health Services Administration and formed in September to respond to the problem — recommended creating maternity care centers that could serve as hubs of integrated care and birthing facilities by building upon the services and personnel already in communities.
The task force will soon determine what portions of the plan will require congressional action and funding to implement and what will be “low-hanging fruit,” said Joy Burkhard, a member of the task force and the executive director of the nonprofit Policy Center for Maternal Mental Health.
Burkhard said equitable access to care is essential. The task force recommended that federal officials identify areas where maternity centers should be placed based on data identifying the underserved. “Rural America,” she said, “is first and foremost.”
There are shortages of care in “unlikely areas,” including Los Angeles County, where some maternity wards have recently closed, said Burkhard. Urban areas that are underserved would also be eligible to get the new centers.
“All that mothers are asking for is maternity care that makes sense. Right now, none of that exists,” she said.
Several pilot programs are designed to help struggling mothers by training and equipping midwives and doulas, people who provide guidance and support to the mothers of newborns.
In Montana, rates of maternal depression before, during, and after pregnancy are higher than the national average. From 2017 to 2020, approximately 15% of mothers experienced postpartum depression and 27% experienced perinatal depression, according to the Montana Pregnancy Risk Assessment Monitoring System. The state had the sixth-highest maternal mortality rate in the country in 2019, when it received a federal grant to begin training doulas.
To date, the program has trained 108 doulas, many of whom are Native American. Native Americans make up 6.6% of Montana’s population. Indigenous people, particularly those in rural areas, have twice the national rate of severe maternal morbidity and mortality compared with white women, according to a study in Obstetrics and Gynecology.
Stephanie Fitch, grant manager at Montana Obstetrics & Maternal Support at Billings Clinic, said training doulas “has the potential to counter systemic barriers that disproportionately impact our tribal communities and improve overall community health.”
Twelve states and Washington, D.C., have Medicaid coverage for doula care, according to the National Health Law Program. They are California, Florida, Maryland, Massachusetts, Michigan, Minnesota, Nevada, New Jersey, Oklahoma, Oregon, Rhode Island, and Virginia. Medicaid pays for about 41% of births in the U.S., according to the Centers for Disease Control and Prevention.
Jacqueline Carrizo, a doula assigned to Aquino through the Emme Coalition, played an important role in Aquino’s recovery. Aquino said she couldn’t have imagined going through such a “dark time alone.” With Carrizo’s support, “I could make it,” she said.
Genetic and environmental factors, or a past mental health disorder, can increase the risk of depression or anxiety during pregnancy. But mood disorders can happen to anyone.
Teresa Martinez, 30, of Price, Utah, had struggled with anxiety and infertility for years before she conceived her first child. The joy and relief of giving birth to her son in 2012 were short-lived.
Without warning, “a dark cloud came over me,” she said.
Martinez was afraid to tell her husband. “As a woman, you feel so much pressure and you don’t want that stigma of not being a good mom,” she said.
In recent years, programs around the country have started to help doctors recognize mothers’ mood disorders and learn how to help them before any harm is done.
One of the most successful is the Massachusetts Child Psychiatry Access Program for Moms, which began a decade ago and has since spread to 29 states. The program, supported by federal and state funding, provides tools and training for physicians and other providers to screen and identify disorders, triage patients, and offer treatment options.
But the expansion of maternal mental health programs is taking place amid sparse resources in much of rural America. Many programs across the country have run out of money.
The federal task force proposed that Congress fund and create consultation programs similar to the one in Massachusetts, but not to replace the ones already in place, said Burkhard.
In April, Missouri became the latest state to adopt the Massachusetts model. Women on Medicaid in Missouri are 10 times as likely to die within one year of pregnancy as those with private insurance. From 2018 through 2020, an average of 70 Missouri women died each year while pregnant or within one year of giving birth, according to state government statistics.
Wendy Ell, executive director of the Maternal Health Access Project in Missouri, called her service a “lifesaving resource” that is free and easy to access for any health care provider in the state who sees patients in the perinatal period.
About 50 health care providers have signed up for Ell’s program since it began. Within 30 minutes of a request, the providers can consult over the phone with one of three perinatal psychiatrists. But while the doctors can get help from the psychiatrists, mental health resources for patients are not as readily available.
The task force called for federal funding to train more mental health providers and place them in high-need areas like Missouri. The task force also recommended training and certifying a more diverse workforce of community mental health workers, patient navigators, doulas, and peer support specialists in areas where they are most needed.
A new voluntary curriculum in reproductive psychiatry is designed to help psychiatry residents, fellows, and mental health practitioners who may have little or no training or education about the management of psychiatric illness in the perinatal period. A small study found that the curriculum significantly improved psychiatrists’ ability to treat perinatal women with mental illness, said Standeven, who contributed to the training program and is one of the study’s authors.
Nancy Byatt, a perinatal psychiatrist at the University of Massachusetts Chan School of Medicine who led the launch of the Massachusetts Child Psychiatry Access Program for Moms in 2014, said there is still a lot of work to do.
“I think that the most important thing is that we have made a lot of progress and, in that sense, I am kind of hopeful,” Byatt said.
Cheryl Platzman Weinstock’s reporting is supported by a grant from the National Institute for Health Care Management Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Easing Election Stress & Anxiety
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At the time of writing, the US is about to have a presidential election. Most of our readers are Americans, and in any case, what the US does tends to affect most of the world, so certainly many readers in other countries will be experiencing stress and anxiety about it too.
We’re a health science publication, not a political outlet, so we’ll refrain from commenting on any candidates or campaign policies, and we’d also like to be clear we are not urging you to any particular action politically—our focus today is simply about mental health.
First, CBT what can be CBT’d
Cognitive Behavioral Therapy (CBT) is far from a panacea, but it’s often a very good starting point. And when it seems the stakes are high, it’s easy to fall into such cognitive distortions as “crystal ball” and “catastrophization”, that is to say, predicting the future and feeling the impact of that (probably undesired version of the) future, and also feeling like it will be the end of the world.
Recognizing these processes and how they work, is the first step to managing our feelings about them.
Learn more: The Art of Being Unflappable (Tricks For Daily Life)
Next, DBT what can be DBT’d
A lot of CBT hinges on the assumption that our assumptions are incorrect. For example, that our friend does not secretly despise us, that our spouse is not about to leave us, that the symptoms we are experiencing are not cancer, and in this case, that the election outcome will not go badly, and if it does, the consequences will be less severe than imagined.
But… What if our concerns are, in fact, fully justified? Here’s where Dialectic Behavior Therapy (DBT) comes in, and with it, what therapists call “radical acceptance”.
In other words, we accept up front the idea that maybe it’s going to be terrible and that will truly suck, and then either:
- there’s nothing we can reasonably do about it now (so worrying just means you’ll suffer twice), or
- there is something we can reasonably do about it now (so we can go do that thing)
After doing the thing (if appropriate), defer processing the outcome of the election until after the election. There is no point in wasting energy to worry before then. In a broadly two-party system where things are usually close between those two largest parties, there’s something close to a 50% chance of an outcome that’s, at least, not the worst you feared.
Learn more: CBT, DBT, & Radical Acceptance
Lastly, empower yourself with Behavioral Activation (BA)
Whatever the outcome of any given election, the world will keep turning, and the individual battles about any given law or policy or such will continue to go on. That’s not to say an election won’t change things—it will—but there will always still be stuff to do on a grassroots level to make the world a better place, no matter what politician has been elected.
Being involved in doing things on a community level will not only help banish any feelings of despair (and if you got the election outcome you wanted, it’ll help you feel involved), but also, it can give you a sense of control, and can even form a part of the “ikigai” that is often talked about as one of the pillars of healthy longevity.
Learn more: What’s Your Ikigai?
And if you like videos, then enjoy this one (narrated by the ever soothing-voiced Alain de Botton):
Watch now: How To Escape From A Despairing Mood (4:46) ← it also has a text version if you prefer that
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: