Syphilis Is Killing Babies. The U.S. Government Is Failing to Stop the Disease From Spreading.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
Karmin Strohfus, the lead nurse at a South Dakota jail, punched numbers into a phone like lives depended on it. She had in her care a pregnant woman with syphilis, a highly contagious, potentially fatal infection that can pass into the womb. A treatment could cure the woman and protect her fetus, but she couldn’t find it in stock at any pharmacy she called — not in Hughes County, not even anywhere within an hour’s drive.
Most people held at the jail where Strohfus works are released within a few days. “What happens if she gets out before I’m able to treat her?” she worried. Exasperated, Strohfus reached out to the state health department, which came through with one dose. The treatment required three. Officials told Strohfus to contact the federal Centers for Disease Control and Prevention for help, she said. The risks of harm to a developing baby from syphilis are so high that experts urge not to delay treatment, even by a day.
Nearly three weeks passed from when Strohfus started calling pharmacies to when she had the full treatment in hand, she said, and it barely arrived in time. The woman was released just days after she got her last shot.
Last June, Pfizer, the lone U.S. manufacturer of the injections, notified the Food and Drug Administration of an “impending stock out” that it anticipated would last a year. The company blamed “an increase in syphilis infection rates as well as competitive shortages.”
Across the country, physicians, clinic staff and public health experts say that the shortage is preventing them from reining in a surge of syphilis and that the federal government is downplaying the crisis. State and local public health authorities, which by law are responsible for controlling the spread of infectious diseases, report delays getting medicine to pregnant people with syphilis. This emergency was predictable: There have been shortages of this drug in eight of the last 20 years.
Yet federal health authorities have not prevented the drug shortages in the past and aren’t doing much to prevent them in the future.
Syphilis, which is typically spread during sex, can be devastating if it goes untreated in pregnancy: About 40% of babies born to women with untreated syphilis can be stillborn or die as newborns, according to the CDC. Infants that survive can suffer from deformed bones, excruciating pain or brain damage, and some struggle to hear, see or breathe. Since this is entirely preventable, a baby born with syphilis is a shameful sign of a failing public health system.
In 2022, the most recent year for which the CDC has data available, more than 3,700 babies were infected with syphilis, including nearly 300 who were stillborn or died as infants. More than 50% of these cases occurred because, even though the pregnant parent was diagnosed with syphilis, they were never properly treated.
That year, there were 200,000 cases identified in the U.S., a 79% increase from five years before. Infection rates among pregnant people and babies increased by more than 250% in that time; South Dakota, where Strohfus works, had the highest rates — including a more than 400% increase among pregnant women. Statewide, the rate of babies born with the disease, a condition known as congenital syphilis, jumped more than 40-fold in just five years.
And that was before the current shortage of shots.
In Mississippi, the state with the second highest rate of syphilis in pregnant women, Dr. Caroline Weinberg started having trouble this summer finding treatments for her clinic’s patients, most of whom are uninsured, live in poverty or lack transportation. She began spending hours each month scouring medicine suppliers’ websites for available doses of the shots, a form of penicillin sold under the brand name Bicillin L-A.
“The way people do it for Taylor Swift, that’s how I’ve been with the Bicillin shortage,” Weinberg said. “Desperately checking the websites to see what I can snag.”
The shortage is driving up infection rates even further.
In a November survey by the National Coalition of STD Directors, 68% of health departments that responded said the drug shortage will cause syphilis rates in their area to increase, further crushing the nation’s most disadvantaged populations.
“This is the most basic medicine,” said Meghan O’Connell, chief public health officer for the Great Plains Tribal Leaders’ Health Board, which represents 18 tribal communities in South Dakota and three other states. “We allow ourselves to continue to not have enough, and it impacts so many people.”
ProPublica examined what the federal government has done to manage the crisis and the ways in which experts say it has fallen short.
The government could pressure Pfizer to be more transparent.
Twenty years ago, there were at least three manufacturers of the syphilis shot. Then Pfizer, one of the manufacturers, purchased the other two companies and became the lone U.S. supplier.
Pfizer’s supply has fallen short since then. In 2016, the company announced a shortage due to a manufacturing issue; it lasted two years. Even during times when Pfizer had not notified the FDA of an official shortage, clinics across the country told ProPublica, the shots were often hard to get.
Several health officials said they would like to see the government use its power as the largest purchaser of the drug to put pressure on Pfizer to produce adequate supplies and to be more transparent about how much of the drug they have on hand, when it will be widely available and how stable the supply will be going forward.
In response to questions, Pfizer said there are two reasons its supply is falling short. One, the company said, was a surge in use of the pediatric form of the drug after a shortage of a different antibiotic last winter. Pfizer also blamed a 70% increase in demand for the adult shots since last February, which it described as unexpected.
Public health experts say the increase in cases and subsequent rise in demand was easy to see coming. Officials have been raising the alarm about skyrocketing syphilis cases for years. “If Pfizer was truly caught completely off guard, it raises significant questions about the competency of the company to forecast obvious infectious disease trends,” a coalition of organizations wrote to the White House Drug Shortage Task Force in September.
Pfizer said it is consistently communicating with the CDC and FDA about its supply and that it has been transparent with public health groups and policymakers.
The FDA has a group dedicated to addressing drug shortages. But Valerie Jensen, associate director of that staff, said the FDA can’t force manufacturers to make more of a drug. “It is up to manufacturers to decide how to respond to that increased demand.” she said. “What we’re here to do is help with those plans.”
Pfizer said it had a target of increasing production by about 20% in 2023 but faced delays toward the end of the year. The company did not explain the reason for those delays.
The company said it has invested $38 million in the last five years in the Michigan facility where it makes the shots and that it is increasing production capacity. It also said it is adding evening shifts at the facility and actively recruiting and training new workers. Pfizer said it also reduced manufacturing time from 110 to 50 days. By the end of June, the company expects the supply to recover, which it described as having eight weeks of inventory based on its forecast demands with no disruptions in sight.
The government could manufacture the drug itself.
Having only one supplier for a drug, especially one of public health importance, makes the country vulnerable to shortages. With just one manufacturer, any disruption — contamination at a plant, a shortage of raw materials, a severe weather event or a flawed prediction of demand — can put lives at risk. What’s ultimately needed, public health experts say, is another manufacturer.
Congressional Democrats recently introduced a bill that would authorize the U.S. Department of Health and Human Services to manufacture generic drugs in exactly this scenario, when there are few manufacturers and regular shortages. Called the Affordable Drug Manufacturing Act, it would also establish an office of drug manufacturing.
This same bill was introduced in 2018, but it didn’t have bipartisan support and was never taken up for a vote. Sen. Elizabeth Warren, the Massachusetts Democrat who introduced the bill in the Senate, said she’s hopeful this time will be different. Lawmakers from both parties understand the risks created by drug shortages, and COVID-19 helped everyone understand the role the government can play to boost manufacturing.
Still, it’s unlikely to be passed with the current gridlock in Congress.
The government could reserve syphilis drugs for infected patients.
Responding to the shortage of shots to treat the disease, the CDC in July asked health care providers nationwide to preserve the scarce remaining doses for people who are pregnant. The shots are considered the gold standard treatment for anyone with syphilis, faster and with fewer side effects than an alternative pill regimen. And for people who are pregnant, the pills are not an option; the shots are the only safe treatment.
Despite that call, the military is giving shots to new recruits who don’t have syphilis, to prevent outbreaks of severe bacterial respiratory infections. The Army has long administered this treatment at boot camps held at Fort Leonard Wood, Fort Moore and Fort Sill. The Army has been unable to obtain the shots several times in the past few years, according to the U.S. Army Center for Initial Military Training. But the Defense Health Agency’s pharmacy operations center has been working with Pfizer to ensure military sites can get them, a spokesperson for the Defense Health Agency said.
“Until we think about public health the way we think about our military, we’re not going to see a difference,” said Dr. John Vanchiere, chief of pediatric infectious diseases at Louisiana State University Health Shreveport.
Some public health officials, including Alaska’s chief medical officer, Dr. Anne Zink, questioned whether the military should be using scarce shots for prevention.
“We should ask if that’s the best use,” she said.
Using antibiotics to prevent streptococcal outbreaks is a well-established, evidence-based public health practice that’s also used by other branches of the armed services, said Lt. Col. Randy Ready, a public affairs officer with the Army’s Initial Military Training center. “The Army continues to work with the CDC and the entire medical community in regards to public health while also taking into account the unique missions and training environments our Soldiers face,” including basic training, Ready said in a written statement.
The government isn’t stockpiling syphilis drugs.
In rare instances, the federal government has created stockpiles of drugs considered key to public health. In 2018, confronting shortages of various drugs to treat tuberculosis, the CDC created a small stockpile of them. And the federal Administration for Strategic Preparedness and Response keeps a national stockpile of supplies necessary for public health emergencies, including vaccines, medical supplies and antidotes needed in case of a chemical warfare attack.
In November, the Biden administration announced it was creating a new syphilis task force. When asked why the federal government doesn’t stockpile syphilis treatments, Adm. Rachel Levine, the HHS official who leads the task force, said officials don’t routinely stockpile drugs, because they have expiration dates.
In a written statement, an HHS spokesperson said that Bicillin has a shelf life of two years and that the Strategic National Stockpile “does not deploy products that are commercially available.” In general, the spokesperson wrote, stockpiles are most effective before a national shortage begins and can’t overcome the problems of limited suppliers or fragile supply chains. “There is also a risk that stockpiles can exacerbate shortages, particularly when supply is already low, by removing drugs from circulation that would have otherwise been available,” the spokesperson wrote.
Stephanie Pang, a senior director with the coalition of STD directors, said that given the critical role of this drug and the severe access concerns, she thinks a stockpile is necessary. “I don’t have another solution that actually gets drugs to patients,” Pang said.
The government could declare a federal emergency.
Some public health officials say the federal government needs to treat the syphilis crisis the way it did Ebola or monkeypox.
Declare a federal emergency, said Dr. Michael Dube, an infectious disease specialist for more than 30 years. That would free up money for more public health staff and fund more creative approaches that could lead to a long-term solution to the near-constant shortages, he said. “I’d hate to have to wait for some horrible anecdotes to get out there in order to get the public’s and the policymakers’ minds on it,” said Dube, who oversees medical care for AIDS Healthcare Foundation wellness clinics across the country.
Citing an alarming surge in syphilis cases, the Great Plains Tribes wrote to the HHS secretary last week asking that the agency declare a public health emergency in their areas. In the request, they asked HHS to work globally to find adequate syphilis treatment and send the needed medicine to the Great Plains region.
During the 2014 outbreak of Ebola in West Africa, Congress gave hundreds of millions of dollars to HHS to help develop new rapid tests and vaccines. Facing a global outbreak of monkeypox in 2022, a White House task force deployed more than a million vaccines, regularly briefed the public and sent extra resources to Pride parades and other places where people at risk were gathered.
Levine, leader of the federal syphilis task force, countered that declaring an emergency wouldn’t make much of a difference. The government, she said, already has a “dramatic and coordinated response” involving several agencies.
The FDA recently approved an emergency import of a similar syphilis treatment made by a French manufacturer that had plenty on hand. According to the company, Provepharm, the imported shots are enough to cover approximately one or two months of typical use by all people in the U.S. (The FDA would not say how many doses Provepharm sent, and the company said it was not allowed to reveal that number under the federal rules governing such emergency imports.)
Clinics applaud that development. But many of them can’t afford the imported shots.
The government could do more to rein in the cost.
Clinics and hospitals that primarily serve low-income patients often qualify for a federal program that allows them to purchase drugs at steeply discounted prices. Pharmaceutical companies that want Medicaid to cover their outpatient drugs must participate in the program.
One factor in determining the discount price is whether a pharmaceutical company has raised the price of a drug by more than the rate of inflation. Because Pfizer has hiked the price of its Bicillin shots significantly over the years, the government requires that it be sold to qualifying clinics for just pennies a dose. Otherwise, a single Pfizer shot can retail for upwards of $500. The French shots are comparable in retail price and not eligible for the discount program.
Several clinic directors also said they worried that drug distributors were reserving the limited supply of the Pfizer shot for organizations that could pay full price. For several days in January, for example, the website of Henry Schein, a medical supplier, showed doses of the shot available at full price, while doses at the penny pricing were out of stock, according to screenshots shared with ProPublica. When asked whether it was only selling shots at full price, a spokesperson for Henry Schein did not respond to the question.
Local health departments that qualify for the discount program told ProPublica they’ve had to pay full price at other distributors, because it was the only stock available.
The Health Resources and Services Administration, the federal agency that regulates the discount program, said that a drug manufacturer is ultimately responsible for ensuring that when supplies are available, they are available at the discounted price. When asked about this, Pfizer said that it has “one inventory that is distributed to our trade partners” and that hospitals and clinics that qualify for the discount program are “responsible for ensuring compliance with the program and orders through the wholesaler accordingly.” The company added, “Pfizer plays no part in this process.”
In October, on Weinberg’s regular search for shots for her Mississippi clinic, she found doses of Bicillin for sale at the discounted price and purchased 40. “The idea that we’re supposed to be hoarding treatment is a horrific compact,” she said. Word got out that the clinic, called Plan A, has some shots, and other clinics began sending pregnant patients there.
The clinic’s supply is dwindling. Weinberg is happy to get the shots to patients who need them. But she’s not sure how much longer her reserve will last — or if she’ll be able to find more when they’re gone.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Origin of Everyday Moods – by Dr. Robert Thayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First of all, what does this title mean by “everyday moods”? By this the author is referring to the kinds of moods we have just as a matter of the general wear-and-tear of everyday life—not the kind that come from major mood disorders and/or serious trauma.
The latter kinds of mood take less explaining, in any case. Dr. Thayer, therefore, spends his time on the less obvious ones—which in turn are the ones that affect most of the most, every day.
Critical to Dr. Thayer’s approach is the mapping of moods by four main quadrants:
- High energy, high tension
- High energy, low tension
- Low energy, high tension
- Low energy, low tension
…though this can be further divided into 25 sectors, if we rate each variable on a scale of 0–4. But for the first treatment, it suffices to look at whether energy and tension are high or low, respectively, and which we’d like to have more or less of.
Then (here be science) how to go about achieving that in the most efficient, evidence-based ways. So, it’s not just a theoretical book; it has great practical value too.
The style of the book is accessible, and walks a fine line between pop-science and hard science, which makes it a great book for laypersons and academics alike.
Bottom line: if you’d like the cheat codes to improve your moods and lessen the impact of bad ones, this is the book for you.
Click here to check out The Origin of Everyday Moods, and manage yours!
Share This Post
-
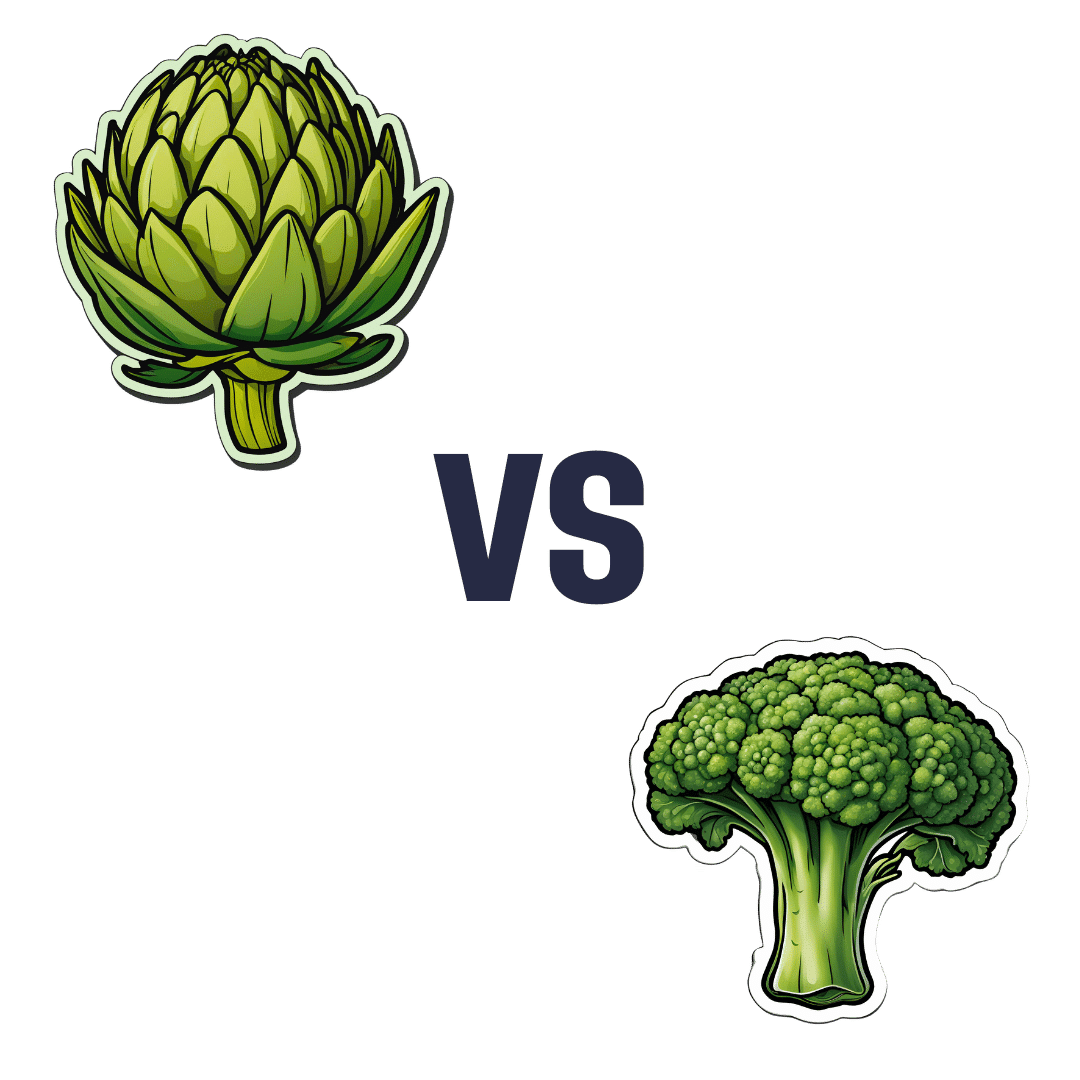
Artichoke vs Broccoli – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to broccoli, we picked the artichoke.
Why?
Both have their strengths, and it was close! But…
In terms of macros, artichoke has about 2x the fiber (which is lots, because broccoli is already good for this) and more protein, for only slightly more carbs, making it the nutrient dense choice in all respects, and especially in the case of fiber.
In the category of vitamins, artichoke has more of vitamins B3, B9, and choline, while broccoli has more of vitamins A, B2, B5, B6, C, E, and K, thus winning this round.
When it comes to minerals, artichoke has more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc, while broccoli has more calcium and selenium, handing artichoke the win again here.
Looking at polyphenols, both have an abundance; artichoke has more by total mass (in terms of mg/100g) and is especially rich in luteolin and phenolic acids, but broccoli has some that artichoke doesn’t have (such as quercetin and kaempferol). We could reasonably call this a tie or a win for artichoke on strength of numbers; either way, it doesn’t change the end result:
Adding up the sections makes for an overall win for artichoke, but of course, by all means enjoy either or both; diversity is good!
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
Self-Compassion In A Relationship (Positives & Pitfalls)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Practise Self-Compassion In Your Relationship (But Watch Out!)
Let’s make clear up-front: this is not about “…but not too much”.
With that in mind…
Now let’s set the scene: you, a happily-partnered person, have inadvertently erred and upset your partner. They may or may not have already forgiven you, but you are still angry at yourself.
Likely next steps include all or any of:
- continuing to apologise and try to explain
- self-deprecatory diatribes
- self-flagellation, probably not literally but in the sense of “I don’t deserve…” and acting on that feeling
- self-removal, because you don’t want to further inflict your bad self on your partner
As you might guess, these are quite varied in their degree of healthiness:
- apologising is good, as even is explaining, but once it’s done, it’s done; let it go
- self-deprecation is pretty much never useful, let alone healthy
- self-flagellation likewise; it is not only inherently self-destructive, but will likely create an additional problem for your partner too
- self-removal can be good or bad depending on the manner of that removal: there’s a difference between just going cold and distant on your partner, and saying “I’m sorry; this is my fault not yours, I don’t want to take it out on you, so please give me half an hour by myself to regain my composure, and I will come back with love then if that’s ok with you”
About that last: mentioning the specific timeframe e.g. “half an hour” is critical, by the way—don’t leave your partner hanging! And then do also follow through on that; come back with love after the half-hour elapses. We suggest mindfulness meditation in the interim (here’s our guide to how), if you’re not sure what to do to get you there.
To Err Is Human; To Forgive, Healthy (Here’s How To Do It) ← this goes for when the forgiveness in question is for yourself, too—and we do write about that there (and how)!
This is important, by the way; not forgiving yourself can cause more serious issues down the line:
If, by the way, you’re hand-wringing over “but was my apology good enough really, or should I…” then here is how to do it. Basically, do this, and then draw a line under it and consider it done:
The Apology Checklist ← you’ll want to keep a copy of this, perhaps in the notes app on your phone, or a screenshot if you prefer
(the checklist is at the bottom of that page)
The catch
It’s you, you’re the catch 👈👈😎
Ok, that being said, there is actually a catch in the less cheery sense of the word, and it is:
“It is important to be compassionate about one’s occasional failings in a relationship” does not mean “It is healthy to be neglectful of one’s partner’s emotional needs; that’s self-care, looking after #1; let them take care of themself too”
…because that’s simply not being a couple at all.
Think about it this way: the famous airline advice,
“Put on your own oxygen mask before helping others with theirs”
…does not mean “Put on your own oxygen mask and then watch those kids suffocate; it’s everyone for themself”
So, the same goes in relationships too. And, as ever, we have science for this. There was a recent (2024) study, involving hundreds of heterosexual couples aged 18–73, which looked at two things, each measured with a scaled questionnaire:
- Subjective levels of self-compassion
- Subjective levels of relationship satisfaction
For example, questions included asking participants to rate, from 1–5 depending on how much they felt the statements described them, e.g:
In my relationship with my partner, I:
- treat myself kindly when I experience sorrow and suffering.
- accept my faults and weaknesses.
- try to see my mistakes as part of human nature.
- see difficulties as part of every relationship that everyone goes through once.
- try to get a balanced view of the situation when something unpleasant happens.
- try to keep my feelings in balance when something upsets me.
Note: that’s not multiple choice! It’s asking participants to rate each response as applicable or not to them, on a scale of 1–5.
And…
❝Women’s self-compassion was also positively linked with men’s total relationship satisfaction. Thus, men seem to experience overall satisfaction with the relationship when their female partner is self-kind and self-caring in difficult situations.
Unexpectedly, however, we found that men’s relationship-specific self-compassion was negatively associated with women’s fulfillment.
Baker and McNulty (2011) reported that, only for men, a Self-Compassion x Conscientiousness interaction explained whether the positive effects of self-compassion on the relationship emerged, but such an interaction was not found for women.
Highly self-compassionate men who were low in conscientiousness were less motivated than others to remedy interpersonal mistakes in their romantic relationships, and this tendency was in turn related to lower relationship satisfaction❞
~ Dr. Astrid Schütz et al. (2024)
And if you’d like to read the cited older paper from 2011, here it is:
Read in full: Self-compassion and relationship maintenance: the moderating roles of conscientiousness and gender
The take-away here is not: “men should not practice self-compassion”
(rather, they absolutely should)
The take-away is: we must each take responsibility for managing our own mood as best we are able; practice self-forgiveness where applicable and forgive our partner where applicable (and communicate that!)…. And then go consciously back to the mutual care on which the relationship is hopefully founded.
Which doesn’t just mean love-bombing, by the way, it also means listening:
The Problem With Active Listening (And How To Do Better)
To close… We say this often, but we mean it every time: take care!
Share This Post
Related Posts
-
The Many Health Benefits Of Garlic
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Many Health Benefits of Garlic
We’re quite confident you already know what garlic is, so we’re going to leap straight in there with some science today:
First, let’s talk about allicin
Allicin is a compound in garlic that gives most of its health benefits. A downside of allicin is that it’s not very stable, so what this means is:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
- So while doing the paperwork isn’t fun, buying it as bulbs is better than buying it as granules or similar
- Allicin also breaks down somewhat in cooking, so raw garlic is best
- Our philosophy is: still use it in cooking as well; just use more!
- Supplements (capsule form etc) use typically use extracts and potency varies (from not great to actually very good)
Read more about that:
- Short-term heating reduces the anti-inflammatory effects of fresh raw garlic extracts
- Allicin Bioavailability and Bioequivalence from Garlic Supplements and Garlic Foods
Now, let’s talk benefits…
Benefits to heart health
Garlic has been found to be as effective as the drug Atenolol at reducing blood pressure:
It also lowers LDL (bad cholesterol):
Benefits to the gut
We weren’t even looking for this, but as it turns out, as an add-on to the heart benefits…
Benefits to the immune system
Whether against the common cold or bringing out the heavy guns, garlic is a booster:
- Preventing the common cold with a garlic supplement: a double-blind, placebo-controlled survey
- Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention
Benefits to the youthfulness of body and brain
Garlic is high in antioxidants that, by virtue of reducing oxidative stress, help slow aging. This effect, combined with the cholesterol and blood pressure benefits, means it may also reduce the risk of Alzheimer’s and other forms of dementia:
- Antioxidant health effects of aged garlic extract
- Effects of garlic consumption on plasma and erythrocyte antioxidant parameters in elderly subjects
- Garlic reduces heart disease and dementia risk
There are more benefits too…
That’s all we have time to dive into study-wise today, but for the visually-inclined, here are yet more benefits to garlic (at a rate of 3–4 cloves per day):
An incredible awesome recipe using lots of garlic:
- Take small potatoes (still in their skins), cut in half
- Add enough peeled cloves of garlic so that you have perhaps a 1:10 ratio of garlic to potato by mass
- Boil (pressure-cooking is ideal) until soft, and drain
- Keeping them in the pan, add a lashing of olive oil, and any additional seasonings per your preference (consider black pepper, rosemary, thyme, parsley)
- Put a lid on the pan, and holding it closed, shake the pan vigorously
- Note: if you didn’t leave the skins on, or you chopped much larger potatoes smaller instead of cutting in half, the potatoes will break up into a rough mash now. This is actually also fine and still tastes (and honestly, looks) great, but it is different, so just be aware, so that you get the outcome you want.
- The garlic, which—unlike the potatoes—didn’t have a skin to hold it together, will now have melted over the potatoes like butter
You can serve like this (it’s delicious already) or finish up in the oven or air-fryer or under the grill, if you prefer a roasted style dish (an amazing option too).
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Garlic is best fresh—allicin breaks down soon after garlic is cut/crushed
-
7 Healthy Gut Habits For Women Over 40 – by Lara West
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With regard to the titular 7 healthy gut habits for women over 40, a chapter is devoted to each one of those habits, and she goes into quite some detail in each category, more than you might expect.
As for the 7 things, we’ll not keep them a mystery; they are:
- Intermittent fasting
- Prebiotics & probiotics
- Mindful eating
- Understanding ingredients
- Movement
- Sleep
- Stress management
Of course, all of these things are good regardless of one’s age or gender, but West is writing with women over 40 in mind, and as such, she will focus on things that are especially relevant to those of us who are indeed women over 40.
You may be wondering: what if I’m a long way over 40, and menopause is a distant memory? In that case, 90% of this will still be relevant to you; the only parts that won’t be, are those that pertain specifically to the menopausal transitional phase itself, rather than the post-menopause state.
You may also be wondering: what if I’m a man, and menopause is just not in the cards for me? In that case, maybe about 70% of this will still be relevant to you, because of the broad applicability of most of the advice. That said, if it’s just for yourself, you’d probably do better with a book of which 100% is relevant to you, rather than this one.
The style is conversational pop-science, with personal anecdotes mixed in with references to science. It’s definitely on the light/easy-reading end of books that we’ve reviewed on the topic.
Bottom line: if you’re a woman over 40 who would like to improve your gut health, this book was written for you.
Click here to check out 7 Healthy Gut Habits For Women Over 40, and rediscover vitality!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Origin of Everyday Moods – by Dr. Robert Thayer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First of all, what does this title mean by “everyday moods”? By this the author is referring to the kinds of moods we have just as a matter of the general wear-and-tear of everyday life—not the kind that come from major mood disorders and/or serious trauma.
The latter kinds of mood take less explaining, in any case. Dr. Thayer, therefore, spends his time on the less obvious ones—which in turn are the ones that affect most of the most, every day.
Critical to Dr. Thayer’s approach is the mapping of moods by four main quadrants:
- High energy, high tension
- High energy, low tension
- Low energy, high tension
- Low energy, low tension
…though this can be further divided into 25 sectors, if we rate each variable on a scale of 0–4. But for the first treatment, it suffices to look at whether energy and tension are high or low, respectively, and which we’d like to have more or less of.
Then (here be science) how to go about achieving that in the most efficient, evidence-based ways. So, it’s not just a theoretical book; it has great practical value too.
The style of the book is accessible, and walks a fine line between pop-science and hard science, which makes it a great book for laypersons and academics alike.
Bottom line: if you’d like the cheat codes to improve your moods and lessen the impact of bad ones, this is the book for you.
Click here to check out The Origin of Everyday Moods, and manage yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: