When You “Can’t Complain”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Bone To Pick… Up And Then Put Back Where We Found It
In today’s Psychology Sunday feature, we’re going to be flipping the narrative on gratitude, by tackling it from the other end.
We have, by the way, written previously about gratitude, and what mistakes to avoid, in one of our pieces on positive psychology:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
“Can’t complain”
Your mission, should you choose to accept it (and come on, who doesn’t like a challenge?) is to go 21 days without complaining (to anyone, including yourself, about anything). If you break your streak, that’s ok, just start again!
Why?
Complaining is (unsurprisingly) inversely correlated with happiness, in a self-perpetuating cycle:
Pet Peeves and Happiness: How Do Happy People Complain?
And if a stronger motivation is required, there’s a considerable inverse correlation between all-cause happiness and all-cause mortality, even when potential confounding factors (e.g., chronic health conditions, socioeconomic status, etc) are controlled for, and especially as we get older:
Investing in Happiness: The Gerontological Perspective
How?
You may have already formulated some objections by this point, for example:
- Am I supposed to tell my doctor/therapist “I’m fine thanks; how are you?”
- Some things are worthy of complaint; should I be silent?
But both of these issues (communication, and righteousness) have answers:
On communication:
There is a difference between complaining, and giving the necessary information in answer to a question—or even volunteering such information.
For example, when our site went down yesterday, some of you wrote to us to let us know the links weren’t working. There is a substantive difference (semantic, ontological, and teleological) between:
- ❝The content was great but the links in “you may have missed” did not work.❞ ← a genuine piece of feedback we received (thank you!)
- ❝Wasted my time, couldn’t read your articles! Unsubscribing, and I hope your socks get wet tomorrow!❞ ← nobody said this; our subscribers are lovely (thank you)
- Note that the former wasn’t a complaint, it was genuinely helpful feedback, without which we might not have noticed the problem and fixed it.
- The latter was a complaint, and also (like many complaints) didn’t even address the actual problem usefully.
What makes it a complaint or not is not the information conveyed, but the tone and intention. So for example:
“You’ve only done half the job I asked you to!” → “Thank you for doing the first half of this job, could you please do the other half now?”
Writer’s anecdote: my washing machine needs a part replaced; the part was ordered two weeks ago and I was told it would take a week to arrive. It’s been two weeks, so tomorrow I will not complain, but I will politely ask whether they have any information about the delay, and a new estimated time of arrival. Because you know what? Whatever the delay is, complaining won’t make it arrive last week!
On righteousness:
Indeed, some things are very worthy of complaint. But are you able to effect a solution by complaining? If not, then it’s just hot air. And venting isn’t without its own merits (we touched on the benefits of emotional catharsis recently), but that should be a mindful choice when you choose to do that, not a matter of reactivity.
Complaining is a subset of criticizing, and criticizing can be done without the feeling and intent of complaining. However, it too should definitely be measured and considered, responsive, not reactive. This itself could be the topic for another main feature, but for now, here’s a Psychology Today article that at least explains the distinction in more words than we have room for here:
React vs Respond: What’s the difference?
This, by the way, also goes the same for engaging in social and political discourse. It’s easy to get angry and reactive, but it’s good to take a moment to pick your battles, and by all means fight for what you believe in, and/but also do so responsively rather than reactively.
Not only will your health thank you, but you’re also more likely to “win friends and influence people” and all that!
What gets measured, gets done
Find a way of tracking your streak. There are apps for that, like this one, or you could find a low-tech method you prefer.
Bonus tip: if you do mess up and complain, and you realize as you’re doing it, take a moment to take a breath and correct yourself in the moment.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
8 Signs Of Iodine Deficiency You Might Not Expect
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Coach Kait (BSc Nutrition & Exercise) is a certified health and nutrition coach, and today she’s here to talk about iodine—which is important for many of our body functions, from thyroid hormone production to metabolic regulation to heart rate management, as well as more superficial-but-important-too things like our skin and hair.
Kait’s hitlist
Here’s what she recommends we look out for:
- Swollen neck: even a slightly swollen neck might indicate low iodine levels (this is because that’s where the thyroid glands are)
- Hair loss: iodine is needed for healthy hair growth, so a deficiency can lead to hair loss / thinning hair
- Dry and flaky skin: with iodine’s role in our homeostatic system not being covered, our skin can dry out as a result
- Feeling cold all the time: because of iodine’s temperature-regulating activities
- Slow heart rate: A metabolic slump due to iodine deficiency can slow down the heart rate, leading to fatigue and weakness (and worse, if it persists)
- Brain fog: trouble focusing can be a symptom of the same metabolic slump
- Fatigue: this is again more or less the same thing, but she said eight signs, so we’re giving you the eight!
- Irregular period (if you normally have such, of course): because iodine affects reproductive hormones too, an imbalance can disrupt menstrual cycles.
For more on each of these, as well as how to get more iodine in your diet, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
You might also like to read:
- A Fresh Take On Hypothyroidism
- Foods For Managing Hypothyroidism (incl. Hashimoto’s)
- Eat To Beat Hyperthyroidism!
Take care!
Share This Post
-
Procrastination, and how to pay off the to-do list debt
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Procrastination, and how pay off the to-do list debt
Sometimes we procrastinate because we feel overwhelmed by the mountain of things we are supposed to be doing. If you look at your to-do list and it shows 60 overdue items, it’s little wonder if you want to bury your head in the sand!
“What difference does it make if I do one of these things now; I will still have 59 which feels as bad as having 60”
So, treat it like you might a financial debt, and make a repayment plan. Now, instead of 60 overdue items today, you have 1/day for the next 60 days, or 2/day for the next 30 days, or 3/day for the next 20 days, etc. Obviously, you may need to work out whether some are greater temporal priorities and if so, bump those to the top of the list. But don’t sweat the minutiae; your list doesn’t have to be perfectly ordered, just broadly have more urgent things to the top and less urgent things to the bottom.
Note: this repayment plan means having set repayment dates.
Up front, sit down and assign each item a specific calendar date on which you will do that thing.
This is not a deadline! It is your schedule. You’ll not try to do it sooner, and you won’t postpone it for later. You will just do that item on that date.
A productivity app like ToDoist can help with this, but paper is fine too.
What’s important here, psychologically, is that each day you’re looking not at 60 things and doing the top item; you’re just looking at today’s item (only!) and doing it.
Debt Reduction/Cancellation
Much like you might manage a financial debt, you can also look to see if any of your debts could be reduced or cancelled.
We wrote previously about the “Getting Things Done” system. It’s a very good system if you want to do that; if not, no worries, but you might at least want to borrow this one idea….
Sort your items into:
Do / Defer / Delegate / Ditch
- Do: if it can be done in under 2 minutes, do it now.
- Defer: defer the item to a specific calendar date (per the repayment plan idea we just talked about)
- Delegate: could this item be done by someone else? Get it off your plate if you reasonably can.
- Ditch: sometimes, it’s ok to realize “you know what, this isn’t that important to me anymore” and scratch it from the list.
As a last resort, consider declaring bankruptcy
Towards the end of the dot-com boom, there was a fellow who unintentionally got his 5 minutes of viral fame for “declaring email bankruptcy”.
Basically, he publicly declared that his email backlog had got so far out of hand that he would now not reply to emails from before the declaration.
He pledged to keep on top of new emails only from that point onwards; a fresh start.
We can’t comment on whether he then did, but if you need a fresh start, that can be one way to get it!
In closing…
Procrastination is not usually a matter of laziness, it’s usually a matter of overwhelm. Hopefully the above approach will help reframe things, and make things more manageable.
Sometimes procrastination is a matter of perfectionism, and not starting on tasks because we worry we won’t do them well enough, and so we get stuck in a pseudo-preparation rut. If that’s the case, our previous main feature on perfectionism may help:
Share This Post
-
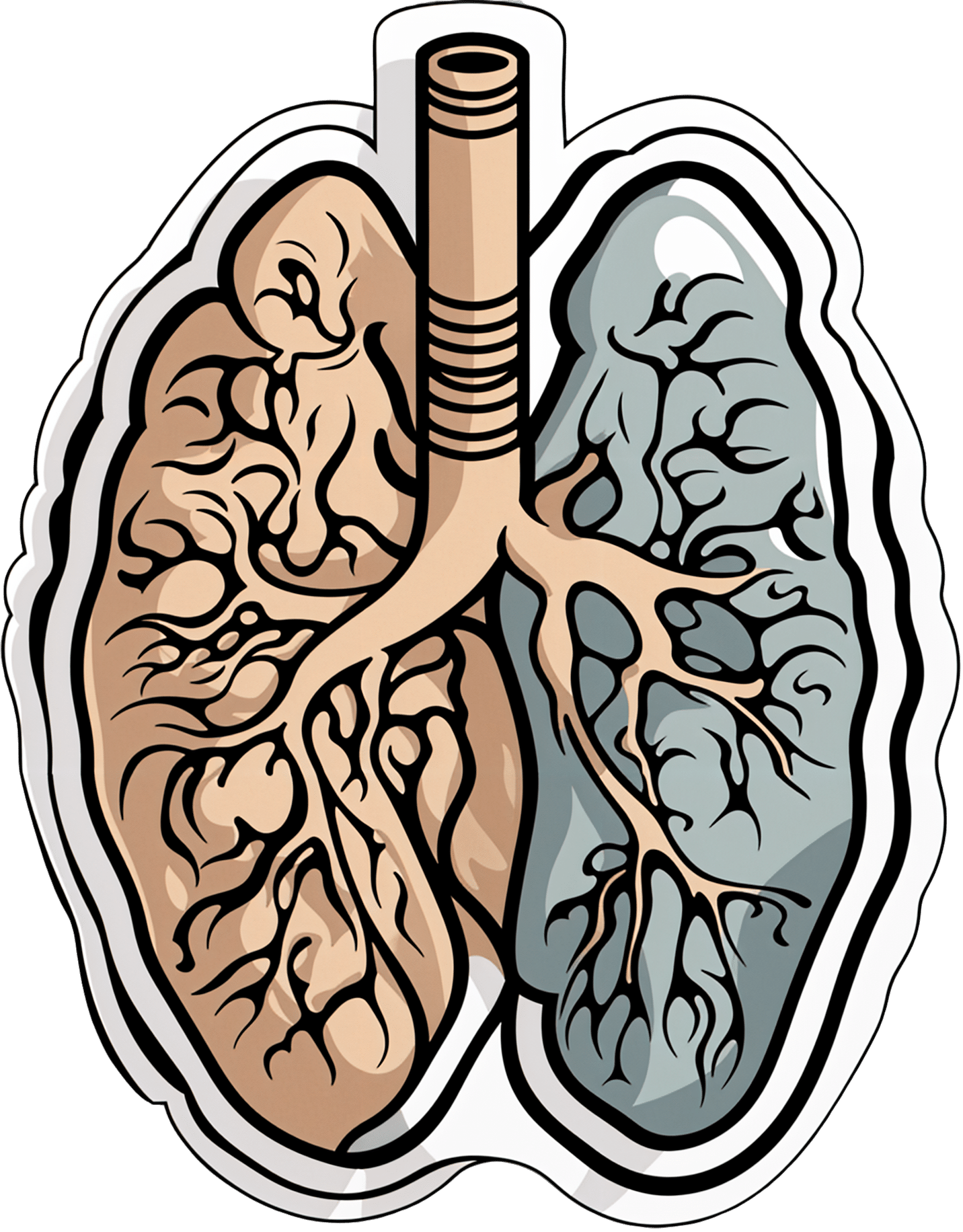
Early Detection May Help Kentucky Tamp Down Its Lung Cancer Crisis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Anthony Stumbo’s heart sank after the doctor shared his mother’s chest X-ray.
“I remember that drive home, bringing her back home, and we basically cried,” said the internal medicine physician, who had started practicing in eastern Kentucky near his childhood home shortly before his mother began feeling ill. “Nobody wants to get told they’ve got inoperable lung cancer. I cried because I knew what this meant for her.”
Now Stumbo, whose mother died the following year, in 1997, is among a group of Kentucky clinicians and researchers determined to rewrite the script for other families by promoting training and boosting awareness about early detection in the state with the highest lung cancer death rate. For the past decade, Kentucky researchers have promoted lung cancer screening, first recommended by the U.S. Preventive Services Task Force in 2013. These days the Bluegrass State screens more residents who are at high risk of developing lung cancer than any state except Massachusetts — 10.6% of eligible residents in 2022, more than double the national rate of 4.5% — according to the most recent American Lung Association analysis.
The effort has been driven by a research initiative called the Kentucky LEADS (Lung Cancer Education, Awareness, Detection, and Survivorship) Collaborative, which in 2014 launched to improve screening and prevention, to identify more tumors earlier, when survival odds are far better. The group has worked with clinicians and hospital administrators statewide to boost screening rates both in urban areas and regions far removed from academic medical centers, such as rural Appalachia. But, a decade into the program, the researchers face an ongoing challenge as they encourage more people to get tested, namely the fear and stigma that swirl around smoking and lung cancer.
Lung cancer kills more Americans than any other malignancy, and the death rates are worst in a swath of states including Kentucky and its neighbors Tennessee and West Virginia, and stretching south to Mississippi and Louisiana, according to data from the Centers for Disease Control and Prevention.
It’s a bit early to see the impact on lung cancer deaths because people may still live for years with a malignancy, LEADS researchers said. Plus, treatment improvements and other factors may also help reduce death rates along with increased screening. Still, data already shows that more cancers in Kentucky are being detected before they become advanced, and thus more difficult to treat, they said. Of total lung cancer cases statewide, the percentage of advanced cases — defined as cancers that had spread to the lymph nodes or beyond — hovered near 81% between 2000 and 2014, according to Kentucky Cancer Registry data. By 2020, that number had declined to 72%, according to the most recent data available.
“We are changing the story of families. And there is hope where there has not been hope before,” said Jennifer Knight, a LEADS principal investigator.
Older adults in their 60s and 70s can hold a particularly bleak view of their mortality odds, given what their loved ones experienced before screening became available, said Ashley Shemwell, a nurse navigator for the lung cancer screening program at Owensboro Health, a nonprofit health system that serves Kentucky and Indiana.
“A lot of them will say, ‘It doesn’t matter if I get lung cancer or not because it’s going to kill me. So I don’t want to know,’” said Shemwell. “With that generation, they saw a lot of lung cancers and a lot of deaths. And it was terrible deaths because they were stage 4 lung cancers.” But she reminds them that lung cancer is much more treatable if caught before it spreads.
The collaborative works with several partners, including the University of Kentucky, the University of Louisville, and GO2 for Lung Cancer, and has received grant funding from the Bristol Myers Squibb Foundation. Leaders have provided training and other support to 10 hospital-based screening programs, including a stipend to pay for resources such as educational materials or a nurse navigator, Knight said. In 2022, state lawmakers established a statewide lung cancer screening program based in part on the group’s work.
Jacob Sands, a lung cancer physician at Boston’s Dana-Farber Cancer Institute, credits the LEADS collaborative with encouraging patients to return for annual screening and follow-up testing for any suspicious nodules. “What the Kentucky LEADS program is doing is fantastic, and that is how you really move the needle in implementing lung screening on a larger scale,” said Sands, who isn’t affiliated with the Kentucky program and serves as a volunteer spokesperson for the American Lung Association.
In 2014, Kentucky expanded Medicaid, increasing the number of lower-income people who qualified for lung cancer screening and any related treatment. Adults 50 to 80 years old are advised to get a CT scan every year if they have accumulated at least 20 pack years and still smoke or have quit within the past 15 years, according to the latest task force recommendation, which widened the pool of eligible adults. (To calculate pack years, multiply the packs of cigarettes smoked daily by years of smoking.) The lung association offers an online quiz, called “Saved By The Scan,” to figure out likely eligibility for insurance coverage.
Half of U.S. patients aren’t diagnosed until their cancer has spread beyond the lungs and lymph nodes to elsewhere in the body. By then, the five-year survival rate is 8.2%.
But regular screening boosts those odds. When a CT scan detects lung cancer early, patients have an 81% chance of living at least 20 years, according to data published in November in the journal Radiology.
Some adults, like Lisa Ayers, didn’t realize lung cancer screening was an option. Her family doctor recommended a CT scan last year after she reported breathing difficulties. Ayers, who lives in Ohio near the Kentucky border, got screened at UK King’s Daughters, a hospital in far eastern Kentucky. The scan didn’t take much time, and she didn’t have to undress, the 57-year-old said. “It took me longer to park,” she quipped.
She was diagnosed with a lung carcinoid tumor, a type of neuroendocrine cancer that can grow in various parts of the body. Her cancer was considered too risky for surgery, Ayers said. A biopsy showed the cancer was slow-growing, and her doctors said they would monitor it closely.
Ayers, a lifelong smoker, recalled her doctor said that her type of cancer isn’t typically linked to smoking. But she quit anyway, feeling like she’d been given a second chance to avoid developing a smoking-related cancer. “It was a big wake-up call for me.”
Adults with a smoking history often report being treated poorly by medical professionals, said Jamie Studts, a health psychologist and a LEADS principal investigator, who has been involved with the research from the start. The goal is to avoid stigmatizing people and instead to build rapport, meeting them where they are that day, he said.
“If someone tells us that they’re not ready to quit smoking but they want to have lung cancer screening, awesome; we’d love to help,” Studts said. “You know what? You actually develop a relationship with an individual by accepting, ‘No.’”
Nationally, screening rates vary widely. Massachusetts reaches 11.9% of eligible residents, while California ranks last, screening just 0.7%, according to the lung association analysis.
That data likely doesn’t capture all California screenings, as it may not include CT scans done through large managed care organizations, said Raquel Arias, a Los Angeles-based associate director of state partnerships at the American Cancer Society. She cited other 2022 data for California, looking at lung cancer screening for eligible Medicare fee-for-service patients, which found a screening rate of 1%-2% in that population.
But, Arias said, the state’s effort is “nowhere near what it needs to be.”
The low smoking rate in California, along with its image as a healthy state, “seems to have come with the unintended consequence of further stigmatizing people who smoke,” said Arias, citing one of the findings from a 2022 report looking at lung cancer screening barriers. For instance, eligible patients may be reluctant to share prior smoking habits with their health provider, she said.
Meanwhile, Kentucky screening efforts progress, scan by scan.
At Appalachian Regional Healthcare, 3,071 patients were screened in 2023, compared with 372 in 2017. “We’re just scratching the surface of the potential lives that we can have an effect on,” said Stumbo, a lung cancer screening champion at the health system, which includes 14 hospitals, most located in eastern Kentucky.
The doctor hasn’t shed his own grief about what his family missed after his mother died at age 51, long before annual screening was recommended. “Knowing that my children were born, and never knowing their grandmother,” he said, “just how sad is that?”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
Related Posts
-
All In Your Head (Which Is Where It’s Supposed To Be)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today’s news is all about things above the neck, and mostly in the brain. From beating depression to beating cognitive decline, from mindfulness against pain to dentistry nightmares to avoid:
Transcranial ultrasound stimulation
Transcranial magnetic stimulation is one of those treatments that sounds like it’s out of a 1950s sci-fi novel, and yet, it actually works (it’s very well-evidenced against treatment-resistant depression, amongst other things). However, a weakness of it is that it’s difficult to target precisely, making modulation of most neurological disorders impossible. Using ultrasound instead of a magnetic field allows for much more finesse, with very promising initial results across a range of neurological disorders
Read in full: Transcranial ultrasound stimulation: a new frontier in non-invasive brain therapy
Related: Antidepressants: Personalization Is Key!
This may cause more pain and damage, but at least it’s more expensive too…
While socialized healthcare systems sometimes run into the problem of not wanting to spend money where it actually is needed, private healthcare systems have the opposite problem: there’s a profit incentive to upsell to more expensive treatments. Here’s how that’s played out in dentistry:
Read in full: Dentists are pulling healthy and treatable teeth to profit from implants, experts warn
Related: Tooth Remineralization: How To Heal Your Teeth Naturally
Mindfulness vs placebo, for pain
It can be difficult with some “alternative therapies” to test against placebo, for example “and control group B will merely believe that they are being pierced with needles”, etc. However, in this case, mindfulness meditation was tested as an analgesic vs sham meditation (just deep breathing) and also vs placebo analgesic cream, vs distraction (listening to an audiobook). Mindfulness meditation beat all of the other things:
Read in full: Mindfulness meditation outperforms placebo in reducing pain
Related: No-Frills, Evidence-Based Mindfulness
Getting personal with AI doctors
One of the common reasons that people reject AI doctors is the “lack of a human touch”. However, human and AI doctors may be meeting in the middle nowadays, as humans are pressed to see more patients in less time, and AI is trained to be more personal—not just a friendlier affect, but also, such things as remembering the patient’s previous encounters (again, something with which overworked human doctors sometimes struggle). This makes a big difference to patient satisfaction:
Read in full: Personalization key to patient satisfaction with AI doctors
Related: AI: The Doctor That Never Tires?
Combination brain therapy against cognitive decline
This study found that out of various combinations trialled, the best intervention against cognitive decline was a combination of 1) cognitive remediation (therapeutic interventions designed to improve cognitive functioning, like puzzles and logic problems), and 2) transcranial direct current stimulation (tDCS), a form of non-invasive direct brain stimulation, similar to the magnetic or ultrasound methods we mentioned earlier today. Here’s how it worked:
Read in full: Study reveals effective combination therapy to slow cognitive decline in older adults
Related: How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Health Tips for Males Too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Articles are very informative and helpful. Maybe it’s me but things seem to lean more toward females. That being said don’t forget us males❞
Rest assured, we could never forget you! We try to make as much as possible of our content applicable to as many as possible of our readers, but of course not everything can be relevant for everyone.
This is, presumably, in response to our recent feature on menopausal health, because previous to that, our next-most-recent main feature that centred women’s health was a month ago—that was about breast cancer, and did have a section on breast cancer in men too. You might also enjoy the book we reviewed recently about prostate health, or our regular sponsor offering testosterone therapy. Please feel free to check out our articles on saw palmetto against male pattern baldness and BPH, as well as mental health issues that disproportionally affect men.
And of course, if you have specific questions/requests about men’s health (or any other health topic) we’re only ever an email away (or use the handy feedback widget, as you did to make this request)!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pistachios vs Almonds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to almonds, we picked the almonds.
Why?
It was very close! And those who’ve been following our “This or That” comparisons might be aware that pistachios and almonds have both been winning their respective comparisons with other nuts so far, so today we put them head-to-head.
In terms of macros, almonds have a little more protein and a little more fiber—as well as slightly more fat, though the fats are healthy. Pistachios, meanwhile, are higher in carbs. A moderate win for almonds on the macro front.
When it comes to vitamins, pistachios have more of vitamins A, B1, and B6, while almonds have more of vitamins B2, B3, and E. We could claim a slight victory for pistachios, based on the larger margins, or else a slight victory for almonds, based on vitamin E being a more common nutritional deficiency than vitamin A, and therefore the more useful vitamin to have more of. We’re going to call this category a tie.
In the category of minerals, almonds lead with more calcium, magnesium, manganese, and zinc, while pistachios boast more copper, potassium, and selenium, though the margins are more modest for pistachios. A moderate win for almonds on minerals, therefore.
Adding up the sections gives a win for almonds, but of course, do enjoy both, because both are excellent in their own right.
Want to learn more?
You might like to read:
- Why You Should Diversify Your Nuts!
- Pistachios vs Walnuts – Which is Healthier?
- Almonds vs Cashews – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: