America’s Health System Isn’t Ready for the Surge of Seniors With Disabilities
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The number of older adults with disabilities — difficulty with walking, seeing, hearing, memory, cognition, or performing daily tasks such as bathing or using the bathroom — will soar in the decades ahead, as baby boomers enter their 70s, 80s, and 90s.
But the health care system isn’t ready to address their needs.
That became painfully obvious during the covid-19 pandemic, when older adults with disabilities had trouble getting treatments and hundreds of thousands died. Now, the Department of Health and Human Services and the National Institutes of Health are targeting some failures that led to those problems.
One initiative strengthens access to medical treatments, equipment, and web-based programs for people with disabilities. The other recognizes that people with disabilities, including older adults, are a separate population with special health concerns that need more research and attention.
Lisa Iezzoni, 69, a professor at Harvard Medical School who has lived with multiple sclerosis since her early 20s and is widely considered the godmother of research on disability, called the developments “an important attempt to make health care more equitable for people with disabilities.”
“For too long, medical providers have failed to address change in society, changes in technology, and changes in the kind of assistance that people need,” she said.
Among Iezzoni’s notable findings published in recent years:
Most doctors are biased. In survey results published in 2021, 82% of physicians admitted they believed people with significant disabilities have a worse quality of life than those without impairments. Only 57% said they welcomed disabled patients.
“It’s shocking that so many physicians say they don’t want to care for these patients,” said Eric Campbell, a co-author of the study and professor of medicine at the University of Colorado.
While the findings apply to disabled people of all ages, a larger proportion of older adults live with disabilities than younger age groups. About one-third of people 65 and older — nearly 19 million seniors — have a disability, according to the Institute on Disability at the University of New Hampshire.
Doctors don’t understand their responsibilities. In 2022, Iezzoni, Campbell, and colleagues reported that 36% of physicians had little to no knowledge of their responsibilities under the 1990 Americans With Disabilities Act, indicating a concerning lack of training. The ADA requires medical practices to provide equal access to people with disabilities and accommodate disability-related needs.
Among the practical consequences: Few clinics have height-adjustable tables or mechanical lifts that enable people who are frail or use wheelchairs to receive thorough medical examinations. Only a small number have scales to weigh patients in wheelchairs. And most diagnostic imaging equipment can’t be used by people with serious mobility limitations.
Iezzoni has experienced these issues directly. She relies on a wheelchair and can’t transfer to a fixed-height exam table. She told me she hasn’t been weighed in years.
Among the medical consequences: People with disabilities receive less preventive care and suffer from poorer health than other people, as well as more coexisting medical conditions. Physicians too often rely on incomplete information in making recommendations. There are more barriers to treatment and patients are less satisfied with the care they do get.
Egregiously, during the pandemic, when crisis standards of care were developed, people with disabilities and older adults were deemed low priorities. These standards were meant to ration care, when necessary, given shortages of respirators and other potentially lifesaving interventions.
There’s no starker example of the deleterious confluence of bias against seniors and people with disabilities. Unfortunately, older adults with disabilities routinely encounter these twinned types of discrimination when seeking medical care.
Such discrimination would be explicitly banned under a rule proposed by HHS in September. For the first time in 50 years, it would update Section 504 of the Rehabilitation Act of 1973, a landmark statute that helped establish civil rights for people with disabilities.
The new rule sets specific, enforceable standards for accessible equipment, including exam tables, scales, and diagnostic equipment. And it requires that electronic medical records, medical apps, and websites be made usable for people with various impairments and prohibits treatment policies based on stereotypes about people with disabilities, such as covid-era crisis standards of care.
“This will make a really big difference to disabled people of all ages, especially older adults,” said Alison Barkoff, who heads the HHS Administration for Community Living. She expects the rule to be finalized this year, with provisions related to medical equipment going into effect in 2026. Medical providers will bear extra costs associated with compliance.
Also in September, NIH designated people with disabilities as a population with health disparities that deserves further attention. This makes a new funding stream available and “should spur data collection that allows us to look with greater precision at the barriers and structural issues that have held people with disabilities back,” said Bonnielin Swenor, director of the Johns Hopkins University Disability Health Research Center.
One important barrier for older adults: Unlike younger adults with disabilities, many seniors with impairments don’t identify themselves as disabled.
“Before my mom died in October 2019, she became blind from macular degeneration and deaf from hereditary hearing loss. But she would never say she was disabled,” Iezzoni said.
Similarly, older adults who can’t walk after a stroke or because of severe osteoarthritis generally think of themselves as having a medical condition, not a disability.
Meanwhile, seniors haven’t been well integrated into the disability rights movement, which has been led by young and middle-aged adults. They typically don’t join disability-oriented communities that offer support from people with similar experiences. And they don’t ask for accommodations they might be entitled to under the ADA or the 1973 Rehabilitation Act.
Many seniors don’t even realize they have rights under these laws, Swenor said. “We need to think more inclusively about people with disabilities and ensure that older adults are fully included at this really important moment of change.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Resistance Beyond Weights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Resistance, Your Way
We’ve talked before about the importance of resistance training:
Resistance Is Useful! (Especially As We Get Older)
And we’ve even talked about how to make resistance training more effective:
(High Intensity Interval Training, but make it High Intensity Resistance Training)
Which resistance training exercises are best?
There are two reasonable correct answers here:
- The resistance training exercises that you will actually do (because it’s no good knowing the best exercise ever if you’re not going to do it because it is in some way offputting to you)
- The resistance training exercises that will prevent you from getting a broken bone in the event of some accident or incident
This latter is interesting, because when people think resistance training, the usually immediate go-to exercises are often things like the bench press, or the chest machine in the gym.
But ask yourself: how often do we hear about some friend or relative who in their old age has broken their humerus?
It can happen, for sure, but it’s not as often as breaking a hip, a tarsal (ankle bones), or a carpal (wrist bones).
So, how can we train to make those bones strong?
Strong bones grow under strong muscles
When archaeologists dig up a skeleton from a thousand years ago, one of the occupations that’s easy to recognize is an archer. Why?
An archer has an unusual frequent exercise: pushing with their left arm while pulling with their right arm. This will strengthen different muscles on each side, and thus, increase bone density in different places on each arm. The left first metacarpal and right first and second metacarpals and phalanges are also a giveaway.
This is because: one cannot grow strong muscles on weak bones (or else the muscles would just break the bones), so training muscles will force the body to strengthen the relevant bones.
So: if you want strong bones, train the muscles attached to those bones
This answers the question of “how am I supposed to exercise my hips” etc.
Weights, bodyweight, resistance bands
If you go to the gym, there’s a machine for everything, and a member of gym staff will be able to advise which of their machines will strengthen which muscles.
If you train with free weights at home:
- Wrist curls (forearm supported and stationary, lifting a dumbbell in your hand, palm-upwards) will strengthen the wrist
- The farmer’s walk (carrying a heavy weight in each hand) will also strengthen your wrist
- A modified version of this involves holding the weight with just your fingertips, and then raising and lowering it by curling and uncurling your fingers)
- Lateral leg raises (you will need ankle-weights for this) will strengthen your ankles and your hips, as will hip abductions (as in today’s featured video), especially with a weight attached.
- Ankle raises (going up on your tip-toes and down again, repeat) while holding weights in your hands will strengthen your ankles
If you don’t like weights:
- Press-ups will strengthen your wrists
- Fingertip press-ups are even better: to do these, do your press-ups as normal, except that the only parts of your hands in contact with the ground are your fingertips
- This same exercise can be done the other way around, by doing pull-ups
- And that same “even better” works by doing pull-ups, but holding the bar only with one’s fingertips, and curling one’s fingers to raise oneself up
- Lateral leg raises and hip abductions can be done with a resistance band instead of with weights. The great thing about these is that whereas weights are a fixed weight, resistance bands will always provide the right amount of resistance (because if it’s too easy, you just raise your leg further until it becomes difficult again, since the resistance offered is proportional to how much tension the band is under).
Remember, resistance training is still resistance training even if “all” you’re resisting is gravity!
If it fells like work, then it’s working
As for the rest of preparing to get older?
Check out:
Training Mobility Ready For Later Life
Take care!
Share This Post
-
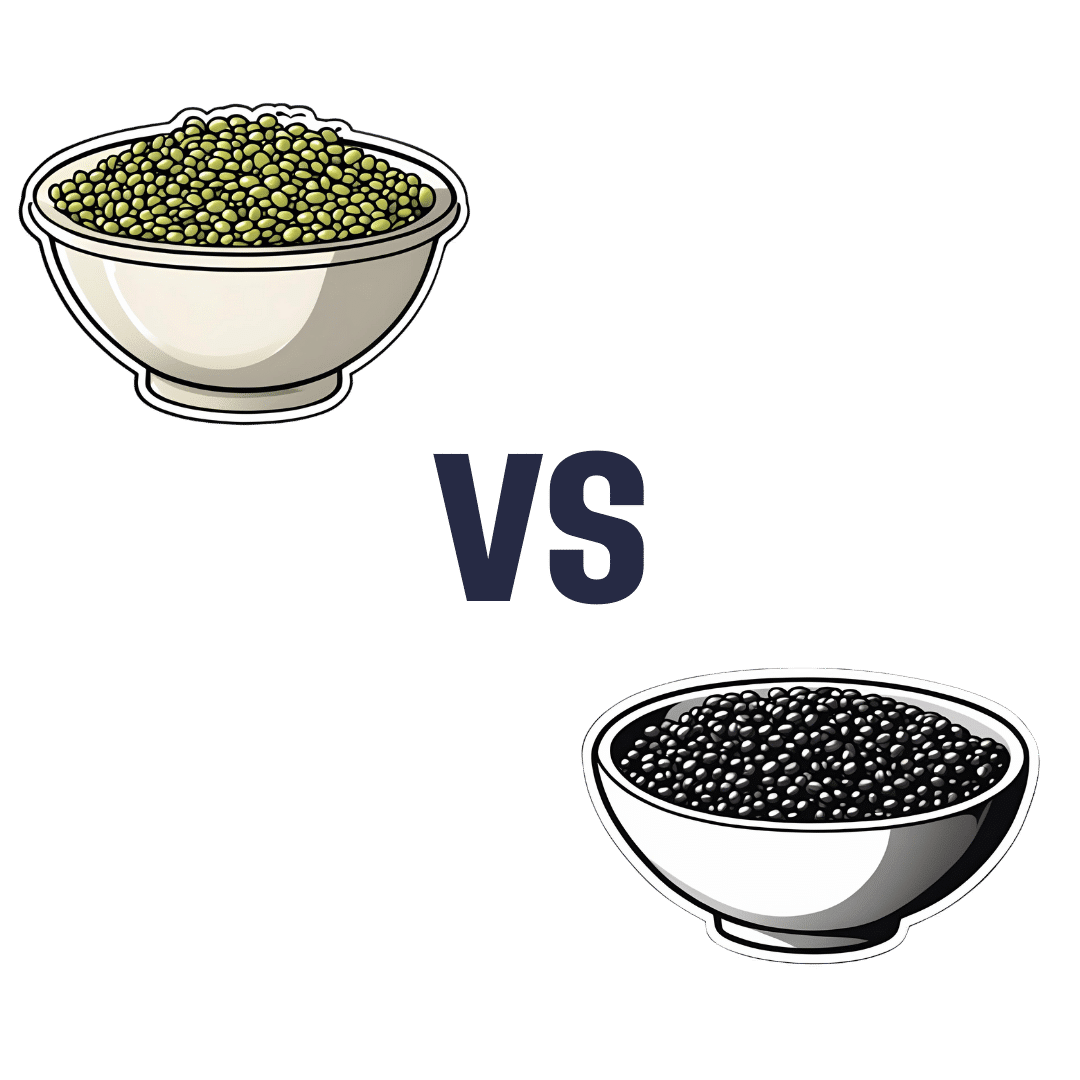
Mung Beans vs Black Gram – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing mung beans to black gram, we picked the black gram.
Why?
Both are great, and it was close!
In terms of macros, the main difference is that mung beans have slightly more fiber, while black gram has slightly more protein. So, it comes down to which we prioritize out of those two, and we’re going to call it fiber and thus hand the win in this category to mung beans—but it’s very close in either case.
In the category of vitamins, mung beans have more of vitamins B1, B6, and B9, while black gram has more of vitamins A, B2, B3, and B5. They’re equal on vitamins C, E, K, and choline. So, a marginal victory by the numbers for black gram here.
When it comes to minerals, mung beans have more copper and potassium, while black gram has more calcium, iron, magnesium, manganese, and phosphorus. They’re equal on selenium and zinc. Another win for black gram.
Adding up the sections makes for an overall win for black gram, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
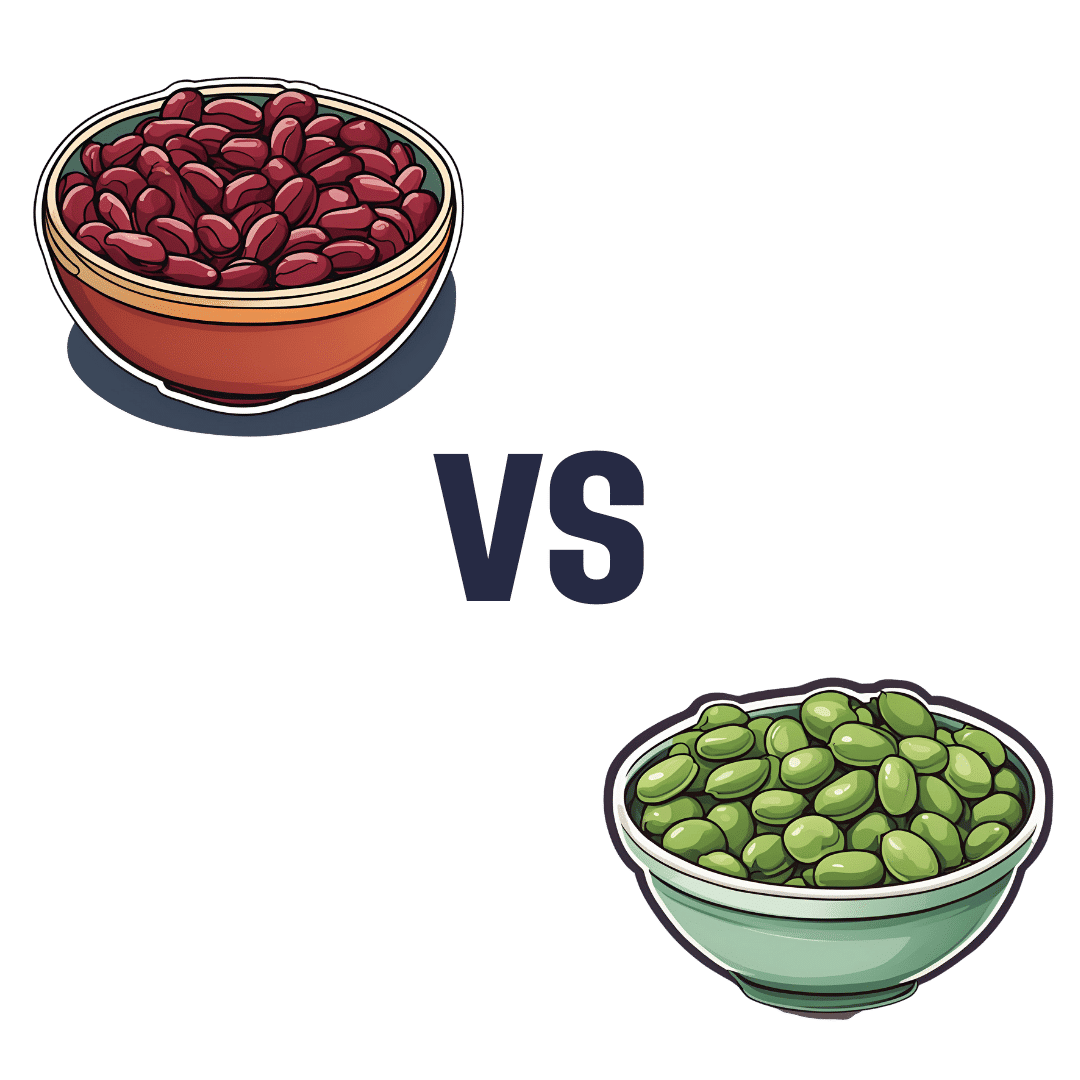
Kidney Beans vs Fava Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to fava beans, we picked the kidney beans.
Why?
It’s a simple and straightforward one today!
The macronutrient profiles are mostly comparable, but kidney beans do have a little more protein and a little more fiber.
In the category of vitamins, kidney beans have more of vitamins B1, B5, B6, B9, C, E, & K, while fava beans boast only more of vitamins B2 and B3. They are both equally good sources of choline, but the general weight of vitamins is very much in kidney beans’ favor, with a 7:2 lead, most of which have generous margins.
When it comes to minerals, kidney beans have more iron, phosphorus, and potassium, while fava beans have more copper and selenium. They’re both equally good sources of other minerals they both contain. Still, a 3:2 victory for kidney beans on the mineral front.
Adding up the moderate victory on macros, the strong victory on vitamins, and the slight victory on minerals, all in all makes for a clear win for kidney beans.
Still, enjoy both! Diversity is healthy.
Want to learn more?
You might like to read:
Chickpeas vs Black Beans – Which is Healthier?
Take care!
Share This Post
Related Posts
-
An Apple (Cider Vinegar) A Day…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
An Apple (Cider Vinegar) A Day…
You’ve probably heard of people drinking apple cider vinegar for its health benefits. It’s not very intuitive, so today we’re going to see what the science has to say…
Apple cider vinegar for managing blood sugars
Whether diabetic, prediabetic, or not at all, blood sugar spikes aren’t good for us, so anything that evens that out is worth checking out. As for apple cider vinegar…
Diabetes Control: Is Vinegar a Promising Candidate to Help Achieve Targets?
…the answer found by this study was “yes”, but their study was small, and they concluded that more research would be worthwhile. So…
…was also a small study, with the same (positive) results.
But! We then found a much larger systematic review was conducted, examining 744 previously-published papers, adding in another 14 they found via those. After removing 47 duplicates, and removing another 15 for not having a clinical trial or not having an adequate control, they concluded:
❝In this systematic review and meta-analyses, the effect of vinegar consumption on postprandial glucose and insulin responses were evaluated through pooled analysis of glucose and insulin AUC in clinical trials. Vinegar consumption was associated with a statistically significant reduction in postprandial glucose and insulin responses in both healthy participants and participants with glucose disorder.❞
~ Sishehbor, Mansoori, & Shirani
Check it out:
Apple cider vinegar for weight loss?
Yep! It appears to be an appetite suppressant, probably moderating ghrelin and leptin levels.
But…
As a bonus, it also lowers triglycerides and total cholesterol, while raising HDL (good cholesterol), and that’s in addition to doubling the weight loss compared to control:
How much to take?
Most of these studies were done with 1–2 tbsp of apple cider vinegar in a glass of water, at mealtime.
Obviously, if you want to enjoy the appetite-suppressant effects, take it before the meal! If you forget and/or choose to take it after though, it’ll still help keep your blood sugars even and still give you the cholesterol-moderating benefits.
Where to get it?
Your local supermarket will surely have it. Or if you buy it online, you can even get it in capsule form!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
General Tso’s Chickpeas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A fiber-rich, heart-healthy take on a classic:
You will need
- 1 can chickpeas, drained
- ¾ cup vegetable stock; ideally you made this yourself from vegetable cuttings that you kept in the freezer for this purpose, but failing that, you should be able to get low-sodium stock cubes at your local supermarket.
- ¼ cup arrowroot starch (cornstarch will do at a pinch, but arrowroot is better and has no flavor of its own)
- 3 tbsp coconut oil
- 2 tbsp grated fresh ginger
- ¼ bulb garlic, minced
- 2 tbsp honey (or maple syrup if you prefer, and if you don’t like sweetness, reduce this to 1 tbsp or even omit entirely, though it won’t be quite so “General Tso” if you do, but it’s your meal!)
- 2 tbsp tomato paste
- 2 tsp hot sauce
- 1 tsp black pepper, coarse ground
- 3 green onions, sliced
Method
(we suggest you read everything at least once before doing anything)
1) Coat the chickpeas in the arrowroot starch by tossing them together in a bowl
2) Heat the coconut oil in a skillet on a medium-high heat, and when hot, add the chickpeas, stirring for 3 minutes
3) Add the remaining ingredients in the order we gave (except the vegetable stock, which goes in last), stirring for 5 more minutes, or until the sauce thickens
4) Serve with the carb of your choice; we recommend our Tasty Versatile Rice Recipe
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Honey vs Maple Syrup – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Build Muscle (Healthily!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do You Have To Gain?
We have previously promised a three-part series about changing one’s weight:
- Losing weight (specifically, losing fat)
- Gaining weight (specifically, gaining muscle)
- Gaining weight (specifically, gaining fat)
And yes, that last one is also something that some people want/need to do (healthily!), and want/need help with that.
There will be, however, no need for a “losing muscle” article, because (even though sometimes a person might have some reason to want to do this), it’s really just a case of “those things we said for gaining muscle? Don’t do those and the muscle will atrophy naturally”.
Here’s the first part: How To Lose Weight (Healthily!)
While some people will want to lose fat, please do be aware that the association between weight loss and good health is not nearly so strong as the weight loss industry would have you believe:
And, while BMI is not a useful measure of health in general, it’s worth noting that over the age of 65, a BMI of 27 (which is in the high end of “overweight”, without being obese) is associated with the lowest all-cause mortality:
BMI and all-cause mortality in older adults: a meta-analysis
Body weight, muscle mass, and protein:
That BMI of 27, or whatever weight you might wish to be, ignores body composition. You’re probably aware that volume-for-volume, muscle weighs more than fat.
You’re also probably aware that if we’re not careful, we tend to lose muscle as we get older. This is known as age-related sarcopenia:
Protein, & Fighting Sarcopenia
Dr. Gabrielle Lyon, our featured expert in the above article, recommends getting at least 1.6g of protein per kg of body weight per day (Americans, divide your weight in pounds by 2.2 to get your weight in kg).
So for example, if you weigh 165lb, that’s 75kg, that’s 1.6×75=120g of protein per day.
There is an upper limit to how much protein per day is healthy, and that limit is probably around 2g of protein per kg of body weight per day:
Protein: How Much Do We Need, Really?
You may be wondering: should we go for animal or plant protein? In which case, the short version is:
- If you only care about muscle growth, any complete sources of protein are fine
- If you care about your general health too, then avoiding red meat is best, but other common protein sources are all fine
- Unprocessed is (unsurprisingly) better than processed in either case
Longer version: Plant vs Animal Protein: Head to Head
What exercises are best for muscle-building?
Of course, different muscles require different exercises, but for all of them, resistance training is what builds muscle the most, and it’s pretty much impossible to build a lot of muscle otherwise.
Check out: Resistance Is Useful! (Especially As We Get Older)
Prepare to fail!
No, really, prepare to fail. Because while resistance training in general is good for maintaining strong muscles and bones, you will only gain muscle if your current muscle is not enough to do the exercise:
- If you do a heavy resistance exercise without undue difficulty, your muscles will say to each other “Good job, team! That was hard, but luckily we were strong enough; no changes necessary”.
- If you do a heavy resistance exercise to the point where you can no longer do it (called: training to failure), then your muscles will say to each other “Oof, what a task! What we’ve got here is clearly not enough, so we’ll have to add more muscle for next time”.
Safety note: training to failure comes with safety risks. If using free weights or weight machines, please do so under well-trained supervision. If doing it with bodyweight (e.g. press-ups until you can press no more) or resistance bands, please check with your doctor first to ensure this is safe for you.
You can also increase the effectiveness of your resistance training by doing it in a way that “confuses” your muscles, making it harder for them to adapt in the moment, and thus forcing them to adapt more in the long term (e.g. get bigger and stronger):
HIIT, But Make It HIRT: High Intensity Resistance Training
Make time for recovery
While many kinds of exercise can be done daily, exercise to build muscle(s) means at the very least resting that muscle (or muscle group) the next day.
For this reason, a lot of bodybuilders have for example a week’s schedule that might look like:
- Monday: Upper body training
- Wednesday: Lower body training
- Friday: Core strength training
…and rest on other days. This gives most muscles a full week of recovery, and every muscle at least 48 hours of recovery.
Note: bodybuilders, like children (who are also doing a lot of body-building, in their own way) need more sleep in order to allow for this recovery and growth to occur. Serious bodybuilders often aim for 12 hours sleep per day. This might be impractical, undesirable, or even impossible for some people, but it’s a factor to be borne in mind and not forgotten.
See also:
Overdone It? How To Speed Up Recovery After Exercise (According To Actual Science)
Anything else that can (safely and healthily) be done to promote muscle growth?
There are a lot of supplements on the market; some are healthy and helpful, other not so much. Here are some we’ve written about:
- What To Eat, Take, And Do Before A Workout
- Creatine: Very Different For Young & Old People
- Ginseng: Exercising With Less Soreness!
- Taurine’s Benefits For Heart Health And More
- Topping Up Testosterone? What To Consider
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: