‘I can’t quite shut it off’: Prevalence of insomnia a growing concern for women
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Tasha Werner, 43, gets up at 3:30 a.m. twice a week for her part-time job at a fitness centre in Calgary. After a five-hour shift, she is back home by 9 a.m. to homeschool her two children, aged 9 and 12. The hardest part of her position – stay-at-home mom, homeschool teacher and part-time worker – is the downtime “lost from my life,” says Werner.
A study by Howard M. Kravitz, a psychiatrist in Chicago, showed that up to 60 per cent of women experience sleep disorders due to hormonal changes linked to menopause. But there is an increasing prevalence of insomnia symptoms in women that may be attributed, in part, to societal changes.
“We live in a world that didn’t exist a generation ago. Now everyone is trying to figure it out,” says Michael Grandner, director of the Sleep and Health Research Program at the University of Arizona.
While women are no longer expected to stay at home, many who are employed outside the home also have the primary responsibility for family matters. And women aged 40 to 60 commonly fall within the “sandwich generation,” caring for both children and parents.
As women juggle their responsibilities, these duties can take a toll, both emotionally and practically.
Both Werner and her husband were raised in traditional homes; their mothers stayed at home to oversee childcare, cooking, grocery shopping and household duties. Initially, Werner and her husband followed a similar path, mirroring their parents’ lives as homemakers. “I think we just fell into what we were used to,” says Werner.
However, a notable shift in their family dynamics occurred once she started working outside the home.
Her children’s physical needs and illnesses have had major consequences on her sleep. If one of the children is sick with the flu, that’s “a week of not a lot of sleep during the night,” she says, “because that’s my job.” Many nights, she finds herself waking up between 1 a.m. and 3 a.m., worrying about how the kids are doing academically or behaviourally.
“We face a specific set of anxieties and a different set of pressures than men,” says Emma Kobil, who has been a therapist in Denver, Colo., for 15 years and is now an insomnia coach. There is so much pressure to be everything as a woman – to be an amazing homemaker and worker while maintaining a hot-rocking body and having a cool personality, to “be the cool mom but also the CEO, to follow your dreams and be the boss b****,” says Kobil.
And there’s an appeal to that concept. Daughters grow up viewing their moms as superwomen juggling responsibilities. But what isn’t always obvious are the challenges women face while managing their lives and the health issues they may encounter.
A study revealed that women are 41 per cent more at risk of insomnia than men.
A thorough study revealed that women are 41 per cent more at risk of insomnia than men. Beyond menopausal hormonal shifts, societal pressures, maternal concerns and the challenge of balancing multiple roles contribute to women’s increased susceptibility to insomnia.
Cyndi Aarrestad, 57, lives on a farm in Saskatchewan with her husband, Denis. Now an empty nester, Aarrestad fills her time working on the farm, keeping house, volunteering at her church and managing her small woodworking business. And she struggles with sleep.
Despite implementing some remedies, including stretching, drinking calming teas and rubbing her feet before bed, Aarrestad says achieving restful sleep has remained elusive for the past decade.
Two primary factors contribute to her sleep challenges — her inability to quiet her mind and hormonal hot flashes due to menopause. Faced with family and outside commitments, Aarrestad finds it challenging to escape night time’s mental chatter. “It’s a mom thing for me … I can’t quite shut it off.” Even as her children transitioned to young adulthood and moved out, the worries persisted, highlighting the lasting concerns moms have about their kids’ jobs, relationships and overall well-being.
Therapist Kobil says that every woman she’s ever worked with experiences this pressure to do everything, to be perfect. These women feel like they’re not measuring up. They’re encouraged to take on other people’s burdens; to be the confidante and the saviour in many ways; to sacrifice themselves. Sleep disruptions simply reflect the consequences of this pressure.
“They’re trying to fit 20 hours in a 24-hour day, and it doesn’t work,” says Grandner, the sleep specialist.
Grandner says that consistently sleeping six hours or less as an adult makes one 55 per cent more likely to become obese, 20 per cent more likely to develop high blood pressure, and 30 per cent more likely to develop Type 2 diabetes if you didn’t have it already. This lack of sleep makes you more likely to catch the flu. It makes vaccines less effective, and it increases your likelihood of developing depression and anxiety.
When is the time to change? Yesterday. Grandner warns that the sleep sacrifices made at a young age impact health later. But it’s never too late to make changes, he says, and “you do the best with what you’ve got.”
Kobil suggests a practical approach for women struggling with sleep. She emphasizes understanding that sleeplessness isn’t a threat and encourages a shift in mindset about being awake. Instead of fighting sleeplessness, she advises treating oneself kindly, recognizing the difficulty.
Kobil recommends creating a simple playbook with comforting activities for awake moments during the night. Just as you would comfort a child who’s afraid, she suggests being gentle with yourself, gradually changing the perception of wakefulness into a positive experience.
This article is republished from HealthyDebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Teas To Drink Before Bed (By Science!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Which Sleepy Tea?
Herbal “tea” preparations (henceforth we will write it without the quotation marks, although these are not true teas) are popular for winding down at the end of a long day ready for a relaxing sleep.
Today we’ll look at the science for them! We’ll be brief for each, because we’ve selected five and have only so much room, but here goes:
Camomile
Simply put, it works and has plenty of good science for it. Here’s just one example:
❝Noteworthy, our meta-analysis showed a significant improvement in sleep quality after chamomile administration❞
Also this writer’s favourite relaxation drink!
(example on Amazon if you want some)
Lavender
We didn’t find robust science for its popularly-claimed sedative properties, but it does appear to be anxiolytic, and anxiety gets in the way of sleep, so while lavender may not be a sedative, it may calm a racing mind all the same, thus facilitating better sleep:
(example on Amazon if you want some)
Magnolia
Animal study for the mechanism:
Human study for “it is observed to help humans sleep better”:
As you can see from the title, its sedative properties weren’t the point of the study, but if you click through to read it, you can see that they found (and recorded) this benefit anyway
(example on Amazon if you want some)
Passionflower
There’s not a lot of evidence for this one, but there is some. Here’s a small study (n=41) that found:
❝Of six sleep-diary measures analysed, sleep quality showed a significantly better rating for passionflower compared with placebo (t(40) = 2.70, p < 0.01). These initial findings suggest that the consumption of a low dose of Passiflora incarnata, in the form of tea, yields short-term subjective sleep benefits for healthy adults with mild fluctuations in sleep quality.❞
So, that’s not exactly a huge body of evidence, but it is promising.
(example on Amazon if you want some)
Valerian
We’ll be honest, the science for this one is sloppy. It’s very rare to find Valerian tested by itself (or sold by itself; we had to dig a bit to find one for the Amazon link below), and that skews the results of science and renders any conclusions questionable.
And the studies that were done? Dubious methods, and inconclusive results:
Nevertheless, if you want to try it for yourself, you can do a case study (i.e., n=1 sample) if not a randomized controlled trial, and let us know how it goes 🙂
(example on Amazon if you want some)
Summary
- Valerian we really don’t have the science to say anything about it
- Passionflower has some nascent science for it, but not much
- Lavender is probably not soporific, but it is anxiolytic
- Magnolia almost certainly helps, but isn’t nearly so well-backed as…
- Camomile comes out on top, easily—by both sheer weight of evidence, and by clear conclusive uncontroversial results.
Enjoy!
Share This Post
-
What’s the difference between miscarriage and stillbirth?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
Former US First Lady Michelle Obama revealed in her memoir she had a miscarriage. UK singer-songwriter and actor Lily Allen has gone on the record about her stillbirth.
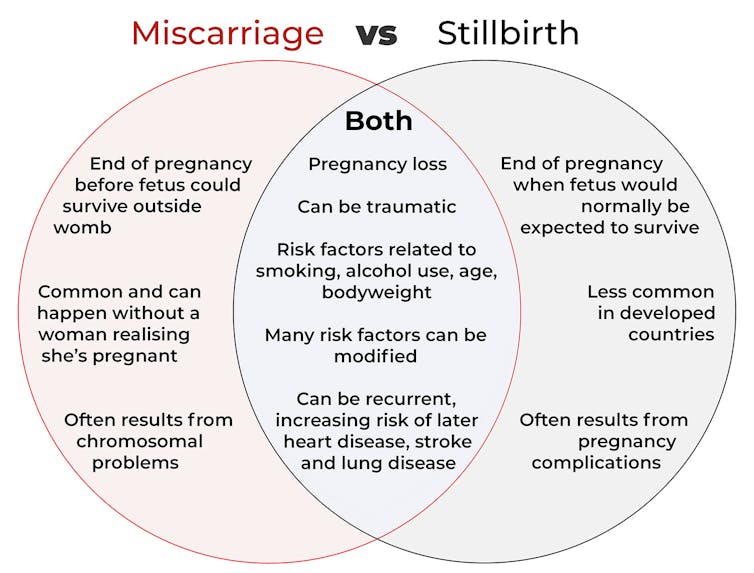
Both miscarriage and stillbirth are sadly familiar terms for pregnancy loss. They can be traumatic life events for the prospective parents and family, and their impacts can be long-lasting. But the terms can be confused.
Here are some similarities and differences between miscarriage and stillbirth, and why they matter.
christinarosepix/Shutterstock Let’s start with some definitions
In broad terms, a miscarriage is when a pregnancy ends while the fetus is not yet viable (before it could survive outside the womb).
This is the loss of an “intra-uterine” pregnancy, when an embryo is implanted in the womb to then develop into a fetus. The term miscarriage excludes ectopic pregnancies, where the embryo is implanted outside the womb.
However, stillbirth refers to the end of a pregnancy when the fetus is normally viable. There may have been sufficient time into the pregnancy. Alternatively, the fetus may have grown large enough to be normally expected to survive, but it dies in the womb or during delivery.
The Australian Institute of Health and Welfare defines stillbirth as a fetal death of at least 20 completed weeks of gestation or with a birthweight of at least 400 grams.
Internationally, definitions of stillbirth vary depending on the jurisdiction.
How common are they?
It is difficult to know how common miscarriages are as they can happen when a woman doesn’t know she is pregnant. There may be no obvious symptoms or something that looks like a heavier-than-normal period. So miscarriages are likely to be more common than reported.
Studies from Europe and North America suggest a miscarriage occurs in about one in seven pregnancies (15%). More than one in eight women (13%) will have a miscarriage at some time in her life.
Around 1–2% of women have recurrent miscarriages. In Australia this is when someone has three or more miscarriages with no pregnancy in between.
Australia has one of the lowest rates of stillbirth in the world. The rate has been relatively steady over the past 20 years at 0.7% or around seven per 1,000 pregnancies.
Who’s at risk?
Someone who has already had a miscarriage or stillbirth has an increased risk of that outcome again in a subsequent pregnancy.
Compared with women who have had a live birth, those who have had a stillbirth have double the risk of another. For those who have had recurrent miscarriages, the risk of another miscarriage is four-fold higher.
Some factors have a u-shaped relationship, with the risk of miscarriage and stillbirth lowest in the middle.
For instance, maternal age is a risk factor for both miscarriage and stillbirth, especially if under 20 years old or older than 35. Increasing age of the male is only a risk factor for stillbirth, especially for fathers over 40.
An older dad can be a risk factor for stillbirth, but not miscarriage. Elizaveta Galitckaia/Shutterstock Similarly for maternal bodyweight, women with a body mass index or BMI in the normal range have the lowest risk of miscarriage and stillbirth compared with those in the obese or underweight categories.
Lifestyle factors such as smoking and heavy alcohol drinking while pregnant are also risk factors for both miscarriage and stillbirth.
So it’s important to not only avoid smoking and alcohol while pregnant, but before getting pregnant. This is because early in the pregnancy, women may not know they have conceived and could unwittingly expose the developing fetus.
Why do they happen?
Miscarriage often results from chromosomal problems in the developing fetus. However, genetic conditions or birth defects account for only 7-14% of stillbirths.
Instead, stillbirths often relate directly to pregnancy complications, such as a prolonged pregnancy or problems with the umbilical cord.
Maternal health at the time of pregnancy is another contributing factor in the risk of both miscarriage and stillbirths.
Chronic diseases, such as high blood pressure, diabetes, hypothyroidism (underactive thyroid), polycystic ovary syndrome, problems with the immune system (such as an autoimmune disorder), and some bacterial and viral infections are among factors that can increase the risk of miscarriage.
Similarly mothers with diabetes, high blood pressure, and untreated infections, such as malaria or syphilis, face an increased risk of stillbirth.
In many cases, however, the specific cause of pregnancy loss is not known.
How about the long-term health risks?
Miscarriage and stillbirth can be early indicators of health issues later in life.
For instance, women who have had recurrent miscarriages or recurrent stillbirths are at higher risk of cardiovascular disease (such as heart disease or stroke).
Our research has also looked at the increased risk of stroke. Compared with women who had never miscarried, we found women with a history of three or more miscarriages had a 35% higher risk of non-fatal stroke and 82% higher risk of fatal stroke.
Women who had a stillbirth had a 31% higher risk of a non-fatal stroke, and those who had had two or more stillbirths were at a 26% higher risk of a fatal stroke.
We saw similar patterns in chronic obstructive pulmonary disease or COPD, a progressive lung disease with respiratory symptoms such as breathlessness and coughing.
Our data showed women with a history of recurrent miscarriages or stillbirths were at a 36% or 67% higher risk of COPD, respectively, even after accounting for a history of asthma.
Long-term health risks of recurrent miscarriages or stillbirths include developing lung disease later in life. PRPicturesProduction/Shutterstock Why is all this important?
Being well-informed about the similarities and differences between these two traumatic life events may help explain what has happened to you or a loved one.
Where risk factors can be modified, such as smoking and obesity, this information can be empowering for individuals who wish to reduce their risk of miscarriage and stillbirth and make lifestyle changes before they become pregnant.
More information and support about miscarriage and stillbirth is available from SANDS and Pink Elephants.
Gita Mishra, Professor of Life Course Epidemiology, Faculty of Medicine, The University of Queensland; Chen Liang, PhD student, reproductive history and non-communicable diseases in women, The University of Queensland, and Jenny Doust, Clinical Professorial Research Fellow, School of Public Health, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Reduce Your Skin Tag Risk
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝As I get older, I seem to be increasingly prone to skin tags, which appear, seemingly out of nowhere, on my face, chest and back. My dermatologist happily burns them off – but is there anything I can do to prevent them?!❞
Not a lot! But, potentially something.
The main risk factor for skin tags is genetic, and you can’t change that in any easy way.
The other main risk factors are connected to each other:
Skin folds, and chafing
Skin tags mostly appear where chafing happens. This can be, for example:
- Inside joint articulations (especially groin and armpits)
- Between fat rolls (if you have them)
So, if you have fat rolls, then losing weight will also reduce the risk of skin tags.
Additionally, obesity and some often-related problems such as diabetes, hypertension, and an atherogenic lipid profile also increase the risk of skin tags (amongst other more serious things):
See: Association of Skin Tag with Metabolic Syndrome and its Components
As for the chafing, this can be reduced in various ways, including:
- losing weight if (and only if) you are carrying excess weight
- dressing against chafing (consider your underwear choices, for example)
- keeping hair in the armpits and groin (it’s part of what it’s there for)
See also: Simply The Pits: These Underarm Myths!
Take care!
Share This Post
Related Posts
-
Superfood Baked Apples
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superfoods, and super-tasty. This is a healthy twist on a classic; your blood sugars will thank you for choosing this tasty sweet delight. It’s also packed with nutrients!
You will need
- 2 large firm baking apples, cored but not peeled
- 1/2 cup chopped walnuts
- 3 tbsp goji berries, rehydrated (soak them in warm water for 10–15minutes and drain)
- 1 tbsp honey, or maple syrup, per your preference (this writer is also a fan of aged balsamic vinegar for its strong flavor and much milder sweetness. If you don’t like things to be too sweet, this is the option for you)
- 2 tsp ground sweet cinnamon
- 1 tsp ground ginger
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 180℃ / 350℉ / gas mark 4
2) Mix the chopped walnuts with the goji berries and the honey (or whatever you used instead of the honey) as well as the sweet cinnamon and the ginger.
3) Place the apples in shallow baking dish, and use the mixture you just made to stuff their holes.
4) Add 1/2 cup water to the dish, around the apples. Cover gently with foil, and bake until soft.
Tip: check them every 20 minutes; they may be done in 40 or it may take 60; in honesty it depends on your oven. If unsure, cook them for longer at a lower temperature.
5) Serve warm.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- From Apples to Bees, and High-Fructose C’s
- Why You Should Diversify Your Nuts!
- Goji Berries: Which Benefits Do They Really Have?
- The Sugary Food That Lowers Blood Sugars
- Honey vs Maple Syrup – Which is Healthier?
- A Tale Of Two Cinnamons ← this is important, about why we chose the sweet cinnamon
- Ginger Does A Lot More Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kiwi Fruit vs Pineapple – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi fruit to pineapple, we picked the kiwi.
Why?
In terms of macros, they’re mostly quite comparable, being fruits made of mostly water, and a similar carb count (slightly different proportions of sugar types, but nothing that throws out the end result, and the GI is low for both). Technically kiwi has twice the protein, but they are fruits and “twice the protein” means “0.5g difference per 100g”. Aside from that, and more meaningfully, kiwi also has twice the fiber.
When it comes to vitamins, kiwi has more of vitamins A, B9, C, E, K, and choline, while pineapple has more of vitamins B1, B2, B3, B5, and B6. This would be a marginal (6:5) win for kiwi, but kiwi’s margins of difference are greater per vitamin, including 72x more vitamin E (with a cupful giving 29% of the RDA, vs a cupful of pineapple giving 0.4% of the RDA) and 57x more vitamin K (with a cupful giving a day’s RDA, vs a cupful of pineapple giving a little under 2% of the RDA). So, this is a fair win for kiwi.
In the category of minerals, things are clear: kiwi has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc, while pineapple has more manganese. An overwhelming win for kiwi.
Looking at their respective anti-inflammatory powers, pineapple has its special bromelain enzymes, which is a point in its favour, but when it comes to actual polyphenols, the two fruits are quite balanced, with kiwi’s flavonoids vs pineapple’s lignans.
Adding up the sections, it’s a clear win for kiwi—but pineapple is a very respectable fruit too (especially because of its bromelain content), so do enjoy both!
Want to learn more?
You might like to read:
Bromelain vs Inflammation & Much More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Twice-Baked Stuffed Potatoes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Packed with protein and fiber and dosed with healthy spices, these tasty treats can be enjoyed hot as they are, or cold as part of a salad dinner.
You will need
- 4 large baking potatoes
- 2 cans chickpeas, drained
- 1 can coconut milk
- ½ cup shredded mozzarella cheese, or plant-based alternative
- 1 bulb garlic (sounds like a lot, but this is about three cloves per potato; adjust if you want, though)
- 3 tbsp chopped pickled jalapeños
- 1 tbsp black pepper
- 2 tsp ground cumin
- 2 tsp dried thyme
- 1 tsp onion powder
- Toppings: smoked paprika, finely chopped parsley
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉ / 200℃.
2) Wash, prick, and bake the potatoes—the latter being for an hour, or until tender.
3) Remove them from the oven and lower the temperature to 350℉ / 175℃.
4) Cut the potatoes lengthways and scoop out the insides into a food processor, leaving enough in the potato that it can hold its shape.
5) Add the remaining ingredients (except the toppings, and half the chickpeas) to the food processor, and blend until smooth.
6) Stuff the filling back into the potato shells (by simple physics of volume, you’ll have a little more than you need, but make it heaped mounds rather than a flat fill-in, and you can probably use most of it, if not all), add the other half of the chickpeas on top and then finally the paprika dusting, and bake for a further 20 minutes.
7) Serve, adding the chopped parsley garnish.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Should You Go Light Or Heavy On Carbs?
- Eat More (Of This) For Lower Blood Pressure
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: