Prolonged Grief: A New Mental Disorder?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The issue is not whether certain mental conditions are real—they are. It is how we conceptualize them and what we think treating them requires.
The latest edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) features a new diagnosis: prolonged grief disorder—used for those who, a year after a loss, still remain incapacitated by it. This addition follows more than a decade of debate. Supporters argued that the addition enables clinicians to provide much-needed help to those afflicted by what one might simply consider a too much of grief, whereas opponents insisted that one mustn’t unduly pathologize grief and reject an increasingly medicalized approach to a condition that they considered part of a normal process of dealing with loss—a process which in some simply takes longer than in others.
By including a condition in a professional classification system, we collectively recognize it as real. Recognizing hitherto unnamed conditions can help remove certain kinds of disadvantages. Miranda Fricker emphasizes this in her discussion of what she dubs hermeneutic injustice: a specific sort of epistemic injustice that affects persons in their capacity as knowers1. Creating terms like ‘post-natal depression’ and ‘sexual harassment’, Fricker argues, filled lacunae in the collectively available hermeneutic resources that existed where names for distinctive kinds of social experience should have been. The absence of such resources, Fricker holds, put those who suffered from such experiences at an epistemic disadvantage: they lacked the words to talk about them, understand them, and articulate how they were wronged. Simultaneously, such absences prevented wrong-doers from properly understanding and facing the harm they were inflicting—e.g. those who would ridicule or scold mothers of newborns for not being happier or those who would either actively engage in sexual harassment or (knowingly or not) support the societal structures that helped make it seem as if it was something women just had to put up with.
For Fricker, the hermeneutical disadvantage faced by those who suffer from an as-of-yet ill-understood and largely undiagnosed medical condition is not an epistemic injustice. Those so disadvantaged are not excluded from full participation in hermeneutic practices, or at least not through mechanisms of social coercion that arise due to some structural identity prejudice. They are not, in other words, hermeneutically marginalized, which for Fricker, is an essential characteristic of epistemic injustice. Instead, their situation is simply one of “circumstantial epistemic bad luck”2. Still, Fricker, too, can agree that providing labels for ill-understood conditions is valuable. Naming a condition helps raise awareness of it, makes it discursively available and, thus, a possible object of knowledge and understanding. This, in turn, can enable those afflicted by it to understand their experience and give those who care about them another way of nudging them into seeking help.
Surely, if adding prolonged grief disorder to the DSM-5 were merely a matter of recognizing the condition and of facilitating assistance, nobody should have any qualms with it. However, the addition also turns intense grief into a mental disorder—something for whose treatment insurance companies can be billed. With this, significant forces of interest enter the scene. The DSM-5, recall, is mainly consulted by psychiatrists. In contrast to talk-therapists like psychotherapists or psychoanalysts, psychiatrists constitute a highly medicalized profession, in which symptoms—clustered together as syndromes or disorders—are frequently taken to require drugs to treat them. Adding prolonged grief disorder thus heralds the advent of research into various drug-based grief therapies. Ellen Barry of the New York Times confirms this: “naltrexone, a drug used to help treat addiction,” she reports, “is currently in clinical trials as a form of grief therapy”, and we are likely to see a “competition for approval of medicines by the Food and Drug Administration.”3
Adding diagnoses to the DSM-5 creates financial incentives for players in the pharmaceutical industry to develop drugs advertised as providing relief to those so diagnosed. Surely, for various conditions, providing drug-induced relief from severe symptoms is useful, even necessary to enable patients to return to normal levels of functioning. But while drugs may help suppress feelings associated with intense grief, they cannot remove the grief. If all mental illnesses were brain diseases, they might be removed by adhering to some drug regimen or other. Note, however, that ‘mental illness’ is a metaphor that carries the implicit suggestion that just like physical illnesses, mental afflictions, too, are curable by providing the right kind of physical treatment. Unsurprisingly, this metaphor is embraced by those who stand to massively benefit from what profits they may reap from selling a plethora of drugs to those diagnosed with any of what seems like an ever-increasing number of mental disorders. But metaphors have limits. Lou Marinoff, a proponent of philosophical counselling, puts the point aptly:
Those who are dysfunctional by reason of physical illness entirely beyond their control—such as manic-depressives—are helped by medication. For handling that kind of problem, make your first stop a psychiatrist’s office. But if your problem is about identity or values or ethics, your worst bet is to let someone reify a mental illness and write a prescription. There is no pill that will make you find yourself, achieve your goals, or do the right thing.
Much more could be said about the differences between psychotherapy, psychiatry, and the newcomer in the field: philosophical counselling. Interested readers may benefit from consulting Marinoff’s work. Written in a provocative, sometimes alarmist style, it is both entertaining and—if taken with a substantial grain of salt—frequently insightful. My own view is this: from Fricker’s work, we can extract reasons to side with the proponents of adding prolonged grief disorder to the DSM-5. Creating hermeneutic resources that allow us to help raise awareness, promote understanding, and facilitate assistance is commendable. If the addition achieves that, we should welcome it. And yet, one may indeed worry that practitioners are too eager to move from the recognition of a mental condition to the implementation of therapeutic interventions that are based on the assumption that such afflictions must be understood on the model of physical disease. The issue is not whether certain mental conditions are real—they are. It is how we conceptualize them and what we think treating them requires.
No doubt, grief manifests physically. It is, however, not primarily a physical condition—let alone a brain disease. Grief is a distinctive mental condition. Apart from bouts of sadness, its symptoms typically include the loss of orientation or a sense of meaning. To overcome grief, we must come to terms with who we are or can be without the loved one’s physical presence in our life. We may need to reinvent ourselves, figure out how to be better again and whence to derive a new purpose. What is at stake is our sense of identity, our self-worth, and, ultimately, our happiness. Thinking that such issues are best addressed by popping pills puts us on a dangerous path, leading perhaps towards the kind of dystopian society Aldous Huxley imagined in his 1932 novel Brave New World. It does little to help us understand, let alone address, the moral and broader philosophical issues that trouble the bereaved and that lie at the root not just of prolonged grief but, arguably, of many so-called mental illnesses.
Footnotes:
1 For this and the following, cf. Fricker 2007, chapter 7.
2 Fricker 2007: 152
3 Barry 2022
References:
Barry, E. (2022). “How Long Should It Take to Grieve? Psychiatry Has Come Up With an Answer.” The New York Times, 03/18/2022, URL = https://www.nytimes.com/2022/03/18/health/prolonged-grief-
disorder.html [last access: 04/05/2022])
Fricker, M. (2007). Epistemic Injustice. Power & the Ethics of knowing. Oxford/New York: Oxford University Press.
Huxley, A. (1932). Brave New World. New York: Harper Brothers.
Marinoff, L. (1999). Plato, not Prozac! New York: HarperCollins Publishers.
Professor Raja Rosenhagen is currently serving as Assistant Professor of Philosophy, Head of Department, and Associate Dean of Academic Affairs at Ashoka University. He earned his PhD in Philosophy from the University of Pittsburgh and has a broad range of philosophical interests (see here). He wrote this article a) because he was invited to do so and b) because he is currently nurturing a growing interest in philosophical counselling.
This article is republished from OpenAxis under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Getting antivirals for COVID too often depends on where you live and how wealthy you are
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Medical experts recommend antivirals for people aged 70 and older who get COVID, and for other groups at risk of severe illness and hospitalisation from COVID.
But many older Australians have missed out on antivirals after getting sick with COVID. It is yet another way the health system is failing the most vulnerable.
CGN089/Shutterstock Who missed out?
We analysed COVID antiviral uptake between March 2022 and September 2023. We found some groups were more likely to miss out on antivirals including Indigenous people, people from disadvantaged areas, and people from culturally and linguistically diverse backgrounds.
Some of the differences will be due to different rates of infection. But across this 18-month period, many older Australians were infected at least once, and rates of infection were higher in some disadvantaged communities.
How stark are the differences?
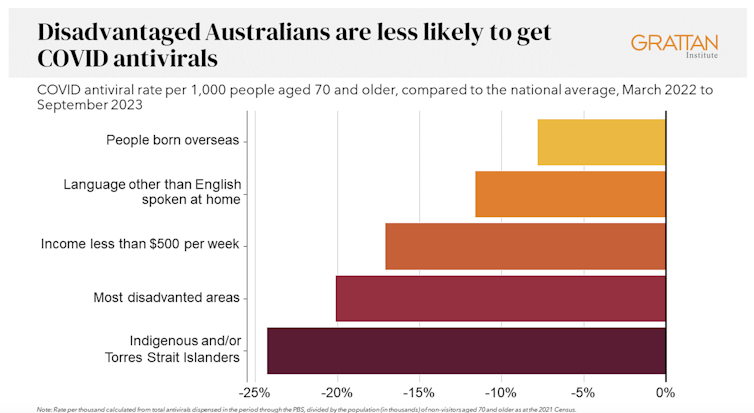
Compared to the national average, Indigenous Australians were nearly 25% less likely to get antivirals, older people living in disadvantaged areas were 20% less likely to get them, and people with a culturally or linguistically diverse background were 13% less likely to get a script.
People in remote areas were 37% less likely to get antivirals than people living in major cities. People in outer regional areas were 25% less likely.
Dispensing rates by group. Grattan Institute Even within the same city, the differences are stark. In Sydney, people older than 70 in the affluent eastern suburbs (including Vaucluse, Point Piper and Bondi) were nearly twice as likely to have had an antiviral as those in Fairfield, in Sydney’s south-west.
Older people in leafy inner-eastern Melbourne (including Canterbury, Hawthorn and Kew) were 1.8 times more likely to have had an antiviral as those in Brimbank (which includes Sunshine) in the city’s west.
Why are people missing out?
COVID antivirals should be taken when symptoms first appear. While awareness of COVID antivirals is generally strong, people often don’t realise they would benefit from the medication. They wait until symptoms get worse and it is too late.
Frequent GP visits make a big difference. Our analysis found people 70 and older who see a GP more frequently were much more likely to be dispensed a COVID antiviral.
Regular visits give an opportunity for preventive care and patient education. For example, GPs can provide high-risk patients with “COVID treatment plans” as a reminder to get tested and seek treatment as soon as they are unwell.
Difficulty seeing a GP could help explain low antiviral use in rural areas. Compared to people in major cities, people in small rural towns have about 35% fewer GPs, see their GP about half as often, and are 30% more likely to report waiting too long for an appointment.
Just like for vaccination, a GP’s focus on antivirals probably matters, as does providing care that is accessible to people from different cultural backgrounds.
Care should go those who need it
Since the period we looked at, evidence has emerged that raises doubts about how effective antivirals are, particularly for people at lower risk of severe illness. That means getting vaccinated is more important than getting antivirals.
But all Australians who are eligible for antivirals should have the same chance of getting them.
These drugs have cost more than A$1.7 billion, with the vast majority of that money coming from the federal government. While dispensing rates have fallen, more than 30,000 packs of COVID antivirals were dispensed in August, costing about $35 million.
Such a huge investment shouldn’t be leaving so many people behind. Getting treatment shouldn’t depend on your income, cultural background or where you live. Instead, care should go to those who need it the most.
Getting antivirals shouldn’t depend on who your GP is. National Cancer Institute/Unsplash People born overseas have been 40% more likely to die from COVID than those born here. Indigenous Australians have been 60% more likely to die from COVID than non-Indigenous people. And the most disadvantaged people have been 2.8 times more likely to die from COVID than those in the wealthiest areas.
All those at-risk groups have been more likely to miss out on antivirals.
It’s not just a problem with antivirals. The same groups are also disproportionately missing out on COVID vaccination, compounding their risk of severe illness. The pattern is repeated for other important preventive health care, such as cancer screening.
A 3-step plan to meet patients’ needs
The federal government should do three things to close these gaps in preventive care.
First, the government should make Primary Health Networks (PHNs) responsible for reducing them. PHNs, the regional bodies responsible for improving primary care, should share data with GPs and step in to boost uptake in communities that are missing out.
Second, the government should extend its MyMedicare reforms. MyMedicare gives general practices flexible funding to care for patients who live in residential aged care or who visit hospital frequently. That approach should be expanded to all patients, with more funding for poorer and sicker patients. That will give GP clinics time to advise patients about preventive health, including COVID vaccines and antivirals, before they get sick.
Third, team-based pharmacist prescribing should be introduced. Then pharmacists could quickly dispense antivirals for patients if they have a prior agreement with the patient’s GP. It’s an approach that would also work for medications for chronic diseases, such as cardiovascular disease.
COVID antivirals, unlike vaccines, have been keeping up with new variants without the need for updates. If a new and more harmful variant emerges, or when a new pandemic hits, governments should have these systems in place to make sure everyone who needs treatment can get it fast.
In the meantime, fairer access to care will help close the big and persistent gaps in health between different groups of Australians.
Peter Breadon, Program Director, Health and Aged Care, Grattan Institute
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
10 Great Exercises to Improve Your Eyesight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If your eyesight has been declining a bit, all is not lost. Just like many other muscles in the body, the muscles of the eye—including those responsible for changing the focal length of your vision—can atrophy without exercise. So, without further ado, here are the exercises recommended:
The eyes (still) have it
- Blink for a minute: blink rapidly for 30–60 seconds to regulate blood circulation, lubricate your eyes, and prevent dryness.
- Rotate your head while staring ahead: turn your head in a circular motion while keeping your gaze straight ahead. This improves blood circulation to your eyes.
- Look to your right and left: slowly move your gaze from right to left while breathing. This one relaxes and stretches the eye muscles.
- Close your eyes and relax: close your eyes for at least 30 seconds to relax and strengthen your photoreceptor cells.
- Move your gaze in different directions: shift your gaze right-left, up-down, in circular motions, and trace a figure 8 with your eyes. This improves visual perception for both near- and far-sightedness.
- Close and open your eyes: tighten your eyes shut for 3–5 seconds, then open them. Repeat seven times to improve blood circulation and relax your eye muscles. ← 10almonds note: the duration makes this different from #4, so do try both!
- Push against your temples with your fingers: gently press your temples with your fingers for two seconds, then release. Repeat 4–5 times to improve fluid circulation in your eyes.
- Draw geometric figures with your gaze: use your eyes to trace shapes such as triangles, squares, and circles to enhance your eye coordination and muscle strength.
- Move your eyeballs up and down: close your eyes and slowly move your eyeballs up and down five times to stretch and relax the muscles ← 10almonds note: this seems to be the same as part of #5 and has a considerable overlap with #8, but we’re listing it anyway, or else everyone will wonder where #9 went!
- Strengthen near and far focusing: focus on your thumb 10 inches away for 10–15 seconds, then switch focus to an object 10–20 feet away. Repeat five times to improve focus adjustment ability.
By practicing these exercises daily, we are told that you can improve eye health and vision within a week.
For more on all these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Vision for Life, Revised Edition – by Dr. Meir Schneider
Take care!
Share This Post
-
Ridged Nails: What Are They Telling You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Yaseen Arsalan, a Doctor of Pharmacy, has advice on the “nutraceutical” side of things:
Onychorrhexis
Sounds like the name of a dinosaur, but it’s actually the condition that creates the vertical ridges that sometimes appear on nails. It’s especially likely in the case of thinner nails, and/or certain nutritional deficiencies. Overuse of certain chemicals (including nail polish remover, hair products that get on your hands a lot, and cleaning fluids) can also cause it. It can also be worsened by various conditions, including eczema, psoriasis, hypothyroidism, anemia, and amyloidosis, but it won’t usually be outright caused by those alone.
There are two main kinds of ridges on nails:
- Vertical ridges: associated with hypothyroidism, anemia, and aging. Often an indicator of low iron.
- Horizontal ridges (Beau’s lines): caused by interrupted nail growth, brute force trauma, chemotherapy, acrylic nails, and gel nail polishes. Can also be an indicator of low zinc.
There are an assortment of medical treatments available, which Dr. Arsalan discusses in the video, but for home remedy treatment, he recommends:
- Nail-strengthening creams (look for coconut oil, shea butter, beeswax, vitamin E)
- Hydration (this is about overall hydration e.g. water intake)
- Careful nail trimming (fingernails with a curved shape and toenails straight across)
- Nail ridge filler (he recommends the brand Barrielle, for not containing formaldehyde or formalin)
- Moisturization (with cuticle oil or hand creams, because that hydration we talked about earlier is important, and we want it to stay inside the nail)
For more on those things, plus the medical treatments plus other “how to avoid this” measures, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Counterintuitive Dos and Don’ts of Nail Health
- Regular Nail Polish vs Gel Nail Polish – Which is Healthier?
Take care!
Share This Post
Related Posts
-
5 Ways To Beat Afternoon Energy Slumps
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Nisha Vora, of Rainbow Plant Life fame. After graduating from Harvard Law School, she realized she hated being a lawyer, and pivoted completely to become what she now is 12 years later, a chef and health coach.
Here are her tips for boosting energy through the day:
Caffeine timing
If you don’t do caffeine at all, no need to change that, but if you do, Vora advises that midday is the best time for it, with a very good rationale:
- of course it should not be too late in the day, because the elimination half-life of caffeine (4–8 hours to eliminate just half of the caffeine, depending on genes, call it 6 hours as an average though honestly for most people it will either be 4 or 8, not 6) is such that it can easily interfere with sleep for most people
- because caffeine is an adenosine blocker, not an adenosine inhibitor, taking caffeine in the morning means either there’s no adenosine to block, or it’ll just “save” that adenosine for later, i.e. when the caffeine is eliminated, then the adenosine will kick in, meaning that your morning sleepiness has now been deferred to the afternoon, rather than eliminated.
Another reminder that caffeine is the “payday loan” of energy. So, midday it is. No morning sleepiness to defer, and yet also not so late as to interfere with sleep.
See also: Calculate (And Enjoy) The Perfect Night’s Sleep
Simplify what can be simplified
This one’s not from a physiological basis, but rather, that a lot of the time most of us have much of our energy being taken by constant task-switching (what gets called multitasking, but as our brain is a single processor, it really means switching rapidly between different kinds of cognition, which is not efficient). In order to avoid that energy drain, try to streamline things and make a particular effort to not only single-task, but to do so without distractions.
Counterpoint: if you have unmedicated ADHD, then chances are you’ll do better with a single small distraction chosen by you, than trying to go without distractions, because your brain will find distractions anyway, so you might as well choose one (for many people it is background music, or a podcast or TV show that one doesn’t may attention to but it’s there) as a matter of harm reduction, and that way you’ll do better at focusing on your primary task than if your brain were reaching out for every and any possible distraction.
Manage your blood sugars
In particular, she advocates for avoiding sugary breakfasts, opting instead for protein, fat, and fiber-rich options. For more in this regard, see:
10 Ways To Balance Your Blood Sugars
Walk after meals
You don’t have to don hiking boots and “I am just going outside and may be some time“; rather, even a 2–5 minute walk after a meal helps regulate digestion and glucose levels, avoiding postprandial energy slumps.
So,
- if you have a treadmill, after eating is a great time to use it for a few minutes
- if you have stairs, now’s a great time to go up and down them a few times
One last technique for when everything else fails
We’ll quote her directly on this one:
❝Despite my best efforts, soemtimes I just have one of those days. Maybe I didn’t sleep well or I’m distracted by my never ending thoughts. If I need to be productive or energized on those days, I will do something that I absolutely hate:
I will take a cold shower.
And I hate it because I’m already always cold all the time, so why would I want to get a cold shower?
Well, it’s because cold water immersion has been shown to dramatically boost your dopamine levels, which gives you more energy and motivation.
In the moment though, it’s mostly painful and I hate everything and everyone around me.
But I know that if I can suffer through two minutes of a cold shower, I will feel so refreshed.❞
There are more benefits than just that, though, see:
A Cold Shower A Day Keeps The Doctor Away?
Want more from Nisha Vora?
We reviewed one of her books a while back:
The Vegan Instant Pot Cookbook – by Nisha Vora
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 5 Love Languages Gone Wrong
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Levelling up the 5 love languages
The saying “happy wife; happy life” certainly goes regardless of gender, and if we’re partnered, it’s difficult to thrive in our individual lives if we’re not thriving as a couple. So, with the usual note that mental health is also just health, let’s take a look at getting beyond the basics of a well-known, often clumsily-applied model:
The 5 love languages
You’re probably familiar with “the 5 love languages”, as developed by Dr. Gary Chapman. If not, they are:
- Acts of Service
- Gift-Giving
- Physical Touch
- Quality Time
- Words of Affirmation
The idea is that we each weight these differently, and problems can arise when a couple are “speaking a different language”.
So, is this a basic compatibility test?
It doesn’t have to be!
We can, if we’re aware of each other’s primary love languages, make an effort to do a thing we wouldn’t necessarily do automatically, to ensure they’re loved the way they need to be.
But…
What a lot of people overlook is that we can also have different primary love languages for giving and for receiving. And, missing that can mean that even taking each other’s primarily love languages into account, efforts to make a partner feel loved, or to feel loved oneself, can miss 50% of the time.
For example, I (your writer here today, hi) could be asked my primary love language and respond without hesitation “Acts of Service!” because that’s my go-to for expressing love.
I’m the person who’ll run around bringing drinks, do all the housework, and without being indelicate, will tend towards giving in the bedroom. But…
A partner trying to act on that information to make me feel loved by giving Acts of Service would be doomed to catastrophic failure, because my knee-jerk reaction would be “No, here, let me do that for you!”
So it’s important for partners to ask each other…
- Not: “what’s your primary love language?” ❌
- But: “what’s your primary way of expressing love?” ✅
- And: “which love language makes you feel most loved?” ✅
For what it’s worth, I thrive on Words of Affirmation, so thanks again to everyone who leaves kind feedback on our articles! It lets me know I provided a good Act of Service
So far, so simple, right? You and your partner (or: other person! Because as we’ve just seen, these go for all kinds of dynamics, not just romantic partnerships) need to be aware of each other’s preferred love languages for giving and receiving.
But…
There’s another pitfall that many fall into, and that’s assuming that the other person has the same idea about what a given love language means, when there’s more to clarify.
For example:
- Acts of Service: is it more important that the service be useful, or that it took effort?
- Gift-Giving: is it better that a gift be more expensive, or more thoughtful and personal?
- Physical Touch: what counts here? If we’re shoulder-to-shoulder on the couch, is that physical touch or is something more active needed?
- Quality Time: does it count if we’re both doing our own thing but together in the same room, comfortable in silence together? Or does it need to be a more active and involved activity together? And is it quality time if we’re at a social event together, or does it need to be just us?
- Words of Affirmation: what, exactly, do we need to hear? For romantic partners, “I love you” can often be important, but is there something else we need to hear? Perhaps a “because…”, or perhaps a “so much that…”, or perhaps something else entirely? Does it no longer count if we have to put the words in our partner’s mouth, or is that just good two-way communication?
Bottom line:
There’s a lot more to this than a “What’s your love language?” click-through quiz, but with a little application and good communication, this model can really resolve a lot of would-be problems that can grow from feeling unappreciated or such. And, the same principles go just the same for friends and others as they do for romantic partners.
In short, it’s one of the keys to good interpersonal relationships in general—something critical for our overall well-being!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s The Deal With MSG?
There are a lot of popular beliefs about MSG. Is there a grain of truth, or should we take them with a grain of salt? We’ll leap straight into myth-busting:
MSG is high in salt
True (technically) False (practically)
- MSG is a salt (a monosodium salt of L-glutamic acid), but to call it “full of salt” in practical terms is like calling coffee “full of fruit”. (Coffee beans are botanically fruit)
- It does contain sodium, though which is what the S stands for!
- We talked previously about how MSG’s sodium content is much lower than that of (table) salt. Specifically, it’s about one third of that of sodium chloride (e.g. table salt).
MSG triggers gluten sensitivity
False!
Or at least, because this kind of absolute negative is hard to prove in science, what we can say categorically is: it does not contain gluten. We understand that the similar name can cause that confusion. However:
- Gluten is a protein, found in wheat (and thus wheat-based foods).
- Glutamate is an amino acid, found in protein-rich foods.
- If you’re thinking “but proteins are made from amino acids”, yes, they are, but the foundational amino acid of gluten is glutamine, not glutamate. Different bricks → different house!
The body can’t process MSG correctly
False!
The body has glutamate receptors throughout the gut and nervous system.
The body metabolizes glutamate from MSG just the same as from any other food that contains it naturally.
Read: Update on food safety of monosodium l-glutamate (MSG) ← evidence-based safety review
MSG causes “Chinese Restaurant Syndrome”
False!
Racism causes that. It finds its origins in what was originally intended as a satirical joke, that the papers picked up and ran with, giving it that name in the 1960s. As to why it grew and persisted, that has more to do with US politics (the US has been often at odds with China for a long time) and xenophobia (people distrust immigrants, such as those who opened restaurants), including nationalistic rhetoric associating immigrants with diseases.
Read: Xenophobia in America in the Age of Coronavirus and Beyond ← academic paper that gives quite a compact yet comprehensive overview
Research science, meanwhile, has not found any such correlation, in more than 40 years of looking.
PS: we realize this item in the list is very US-centric. Apologies to our non-US subscribers. We know that this belief isn’t so much of a thing outside the US—though it certainly can crop up elsewhere sometimes, too.
Are there any health risks associated with MSG, then?
Well, as noted, it does contain sodium, albeit much less than table salt. So… do go easy on it, all the same.
Aside from that, the LD50 (a way of measuring toxicity) of MSG is 15.8g/kg, so if for example you weigh 150lb (68 kg), don’t eat 2.2lb (a kilogram) of MSG.
There have been some studies on rats (or in one case, fruit flies) that found high doses of MSG could cause heart problems and/or promote obesity. However:
- this has not been observed to be the case in humans
- those doses were really high, ranging from 1g/kg to 8g/kg. So that’d be the equivalent of our 150lb person eating it by the cupful
- it was injected (as a solution) into the rats, not ingested by them
- so don’t let someone inject you with a cup of MSG!
Read: A review of the alleged health hazards of monosodium glutamate
Bottom line on MSG and health:
Enjoy in moderation, but enjoy if you wish! MSG is just the salt form of the amino acid glutamate, which is found naturally in many foods, including shrimp, seaweed, and tomatoes.
Scientists have spent more than 40 years trying to find health risks for MSG, and will probably keep trying (which is as science should be), but for now… Everything has either come up negative, or has been the result of injecting laboratory animals with megadoses.
If you’d like to try it in your cooking as a low-sodium way to bring out the flavor of your dishes, you can order it online. Cheapest in bulk, but try it and see if you like it first!
(I’ll be real with you… I have 5 kg in the pantry myself and use about half a teaspoon a day, cooking for two)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: