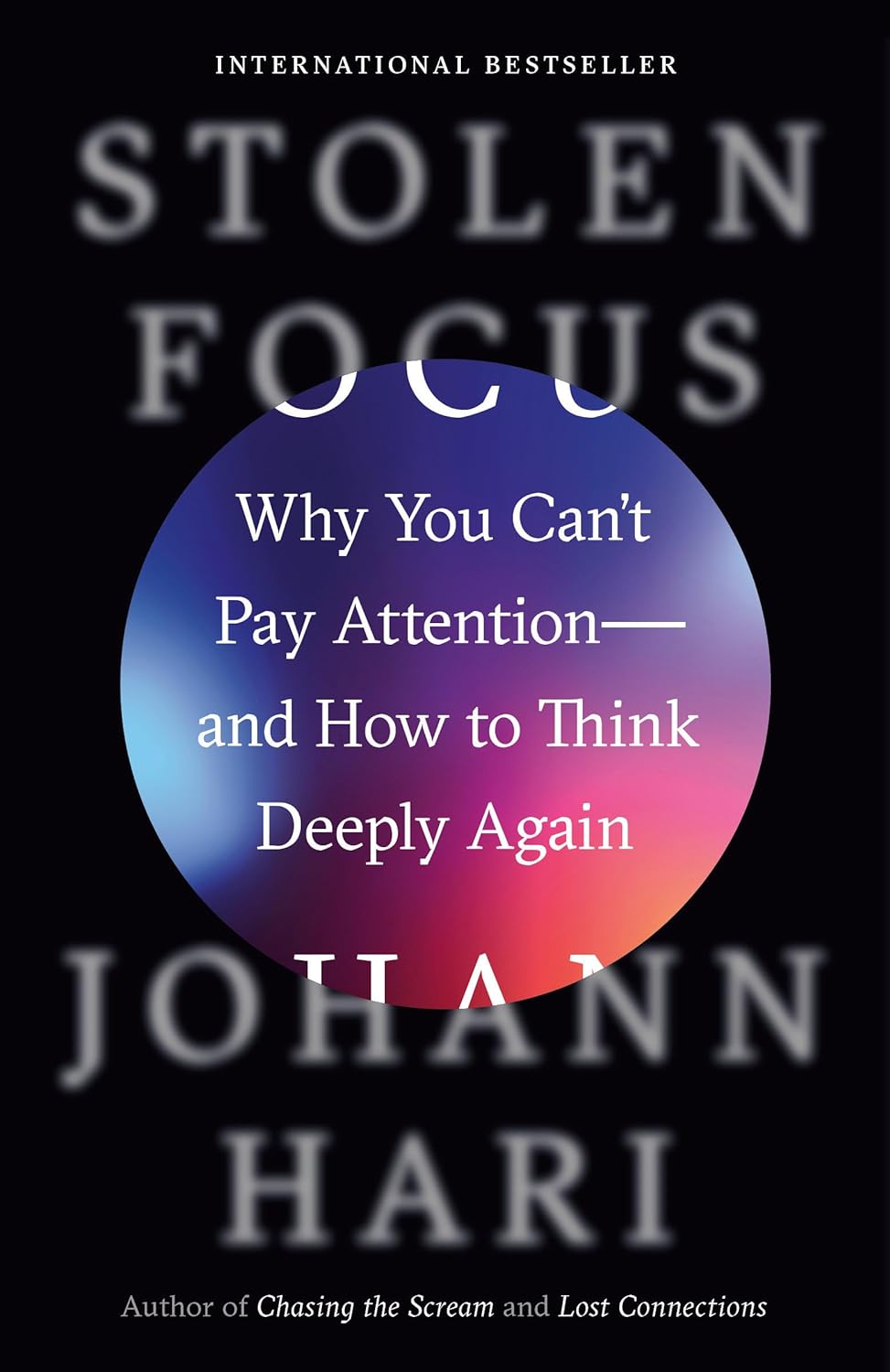
Stolen Focus – by Johann Hari
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Having trouble concentrating for long periods? It’s not just a matter of getting older…
Johann Hari outlines twelve key ways in which our attention has not merely “wandered”, so much as it has been outright stolen.
By whom? For what purpose? Obvious culprits include social media and outrage-stoking news outlets, but the problem, as Hari illustrates, goes much deeper than that.
He talks about how we cannot truly multi-task, and can only switch beween tasks, at a cost. And yet, the modern world is not at all friendly to single-tasking!
Writer’s note: as I write this, I have active two screens, containing four windows, one of which has three tabs open. I am not multitasking; all those things pertain to the work I am doing right now. If I closed them between use, it’d only cost me more time and attention opening and closing them all the time. And yet, my working conditions are considered practically “hyperfocused” in this century!
- We learn about how the working world has changed, and the rise of physical and mental exhaustion that has come with it.
- We learn about the collapse of sustained reading, that started well before the modern Internet.
- We learn about factors such as dietary shifts that sap our energy too.
…and more. Twelve key things, remember.
But, it’s not all doom and gloom. There are things we can do to fight back. Some are personal changes; others are societal changes to push for.
The last part of the book is given over to, essentially, a manifesto (and how-to guide) for reclaiming our attention and thinking deeply again.
Bottom line: if you struggle with maintaining attention; this is a book for you. You might want to put your phone in a drawer while you read it, though
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Nicotine Benefits (That We Don’t Recommend)!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Does nicotine have any benefits at all? I know it’s incredibly addictive but if you exclude the addiction, does it do anything?❞
Good news: yes, nicotine is a stimulant and can be considered a performance enhancer, for example:
❝Compared with the placebo group, the nicotine group exhibited enhanced motor reaction times, grooved pegboard test (GPT) results on cognitive function, and baseball-hitting performance, and small effect sizes were noted (d = 0.47, 0.46 and 0.41, respectively).❞
Read in full: Acute Effects of Nicotine on Physiological Responses and Sport Performance in Healthy Baseball Players
However, another study found that its use as a cognitive enhancer was only of benefit when there was already a cognitive impairment:
❝Studies of the effects of nicotinic systems and/or nicotinic receptor stimulation in pathological disease states such as Alzheimer’s disease, Parkinson’s disease, attention deficit/hyperactivity disorder and schizophrenia show the potential for therapeutic utility of nicotinic drugs.
In contrast to studies in pathological states, studies of nicotine in normal-non-smokers tend to show deleterious effects.
This contradiction can be resolved by consideration of cognitive and biological baseline dependency differences between study populations in terms of the relationship of optimal cognitive performance to nicotinic receptor activity.
Although normal individuals are unlikely to show cognitive benefits after nicotinic stimulation except under extreme task conditions, individuals with a variety of disease states can benefit from nicotinic drugs❞
Read in full: Effects of nicotinic stimulation on cognitive performance
Bad news: its addictive qualities wipe out those benefits due to tolerance and thus normalization in short order. So you may get those benefits briefly, but then you’re addicted and also lose the benefits, as well as also ruining your health—making it a lose/lose/lose situation quite quickly.
As an aside, while nicotine is poisonous per se, in the quantities taken by most users, the nicotine itself is not usually what kills. It’s mostly the other stuff that comes with it (smoking is by far and away the worst of all; vaping is relatively less bad, but that’s not a strong statement in this case) that causes problems.
See also: Vaping: A Lot Of Hot Air?
However, this is still not an argument for, say, getting nicotine gum and thinking “no harmful effects” because then you’ll be get a brief performance boost yes before it runs out and being addicted to it and now being in a position whereby if you stop, your performance will be lower than before you started (since you now got used to it, and it became your new normal), before eventually recovering:
In summary
We recommend against using nicotine in the first place, and for those who are addicted, we recommend quitting immediately if not contraindicated (check with your doctor if unsure; there are some situations where it is inadvisable to take away something your body is dependent on, until you correct some other thing first).
For more on quitting in general, see:
Addiction Myths That Are Hard To Quit
Take care!
Share This Post

This Is Your Brain on Music – by Dr. Daniel Levitin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Music has sometimes been touted as having cognitive benefits, by its practice and even by the passive experience of it. But what’s the actual science of it?
Dr. Levitin, an accomplished musician and neuroscientist, explores and explains.
We learn about how music in all likelihood allowed our ancestors to develop speech, something that set us apart (and ahead!) as a species. How music was naturally-selected-for in accordance with its relationship with health. How processing music involves almost every part of the brain. How music pertains specifically to memory. And more.
As a bonus, as well as explaining a lot about our brain, this book offers those of us with limited knowledge of music theory a valuable overview of the seven main dimensions of music, too.
Bottom line: if you’d like to know more about the many-faceted relationship between music and cognitive function, this is a top-tier book about such.
Click here to check out “This Is Your Brain On Music”, and learn more about yours!
Share This Post

Dry Needling for Meralgia Paresthetica?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Could you address dry needling, who should administer it, and could it be a remedy for meralgia paresthetica? If not, could you speak to home-based remedies for meralgia paresthetica? Thank you?❞
We’ll need to take a main feature some time to answer this one fully, but we will say some quick things here:
- Dry needling, much like acupuncture, has been found to help with pain relief.
- Meralgia paresthetica, being a neuropathy, may benefit from some things that benefit people with peripheral neuropathy, such as lion’s mane mushroom. There is definitely not research to support this hypothesis yet though (so far as we could find anyway; there is plenty to support lion’s mane helping with nerve regeneration in general, but nothing specific for meralgia paresthetica).
Some previous articles you might enjoy meanwhile:
- Pinpointing The Usefulness Of Acupuncture
- Science-Based Alternative Pain Relief
- Peripheral Neuropathy: How To Avoid It, Manage It, Treat It
- What Does Lion’s Mane Actually Do, Anyway?
Take care!
Share This Post
Related Posts

Healthy Habits for Managing & Reversing Prediabetes – by Dr. Marie Feldman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The book doesn’t assume prior knowledge, and does explain the science of diabetes, prediabetes, the terms and the symptoms, what’s going on inside, etc—before getting onto the main meat of the book, the tips.
The promised 100 tips are varied in their application; they range from diet and exercise, to matters of sleep, stress, and even love.
There are bonus tips too! For example, an appendix covers “tips for healthier eating out” (i.e. in restaurants etc) and a grocery list to ensure your pantry is good for defending you against prediabetes.
The writing style is very accessible pop-science; this isn’t like reading some dry academic paper—though it does cite its sources for claims, which we always love to see.
Bottom line: if you’d like to proof yourself against prediabetes, and are looking for “small things that add up” habits to get into to achieve that, this book is an excellent first choice.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Doctors Are as Vulnerable to Addiction as Anyone. California Grapples With a Response
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
BEVERLY HILLS, Calif. — Ariella Morrow, an internal medicine doctor, gradually slid from healthy self-esteem and professional success into the depths of depression.
Beginning in 2015, she suffered a string of personal troubles, including a shattering family trauma, marital strife, and a major professional setback. At first, sheer grit and determination kept her going, but eventually she was unable to keep her troubles at bay and took refuge in heavy drinking. By late 2020, Morrow could barely get out of bed and didn’t shower or brush her teeth for weeks on end. She was up to two bottles of wine a day, alternating it with Scotch whisky.
Sitting in her well-appointed home on a recent autumn afternoon, adorned in a bright lavender dress, matching lipstick, and a large pearl necklace, Morrow traced the arc of her surrender to alcohol: “I’m not going to drink before 5 p.m. I’m not going to drink before 2. I’m not going to drink while the kids are home. And then, it was 10 o’clock, 9 o’clock, wake up and drink.”
As addiction and overdose deaths command headlines across the nation, the Medical Board of California, which licenses MDs, is developing a new program to treat and monitor doctors with alcohol and drug problems. But a fault line has appeared over whether those who join the new program without being ordered to by the board should be subject to public disclosure.
Patient advocates note that the medical board’s primary mission is “to protect healthcare consumers and prevent harm,” which they say trumps physician privacy.
The names of those required by the board to undergo treatment and monitoring under a disciplinary order are already made public. But addiction medicine professionals say that if the state wants troubled doctors to come forward without a board order, confidentiality is crucial.
Public disclosure would be “a powerful disincentive for anybody to get help” and would impede early intervention, which is key to avoiding impairment on the job that could harm patients, said Scott Hambleton, president of the Federation of State Physician Health Programs, whose core members help arrange care and monitoring of doctors for substance use disorders and mental health conditions as an alternative to discipline.
But consumer advocates argue that patients have a right to know if their doctor has an addiction. “Doctors are supposed to talk to their patients about all the risks and benefits of any treatment or procedure, yet the risk of an addicted doctor is expected to remain a secret?” Marian Hollingsworth, a volunteer advocate with the Patient Safety Action Network, told the medical board at a Nov. 14 hearing on the new program.
Doctors are as vulnerable to addiction as anyone else. People who work to help rehabilitate physicians say the rate of substance use disorders among them is at least as high as the rate for the general public, which the federal Substance Abuse and Mental Health Services Administration put at 17.3% in a Nov. 13 report.
Alcohol is a very common drug of choice among doctors, but their ready access to pain meds is also a particular risk.
“If you have an opioid use disorder and are working in an operating room with medications like fentanyl staring you down, it’s a challenge and can be a trigger,” said Chwen-Yuen Angie Chen, an addiction medicine doctor who chairs the Well-Being of Physicians and Physicians-in-Training Committee at Stanford Health Care. “It’s like someone with an alcohol use disorder working at a bar.”
From Pioneer to Lagger
California was once at the forefront of physician treatment and monitoring. In 1981, the medical board launched a program for the evaluation, treatment, and monitoring of physicians with mental illness or substance use problems. Participants were often required to take random drug tests, attend multiple group meetings a week, submit to work-site surveillance by colleagues, and stay in the program for at least five years. Doctors who voluntarily entered the program generally enjoyed confidentiality, but those ordered into it by the board as part of a disciplinary action were on the public record.
The program was terminated in 2008 after several audits found serious flaws. One such audit, conducted by Julianne D’Angelo Fellmeth, a consumer interest lawyer who was chosen as an outside monitor for the board, found that doctors in the program were often able to evade the random drug tests, attendance at mandatory group therapy sessions was not accurately tracked, and participants were not properly monitored at work sites.
Today, MDs who want help with addiction can seek private treatment on their own or in many cases are referred by hospitals and other health care employers to third parties that organize treatment and surveillance. The medical board can order a doctor on probation to get treatment.
In contrast, the California licensing boards of eight other health-related professions, including osteopathic physicians, registered nurses, dentists, and pharmacists, have treatment and monitoring programs administered under one master contract by a publicly traded company called Maximus Inc. California paid Maximus about $1.6 million last fiscal year to administer those programs.
When and if the final medical board regulations are adopted, the next step would be for the board to open bidding to find a program administrator.
Fall From Grace
Morrow’s troubles started long after the original California program had been shut down.
The daughter of a prominent cosmetic surgeon, Morrow grew up in Palm Springs in circumstances she describes as “beyond privileged.” Her father, David Morrow, later became her most trusted mentor.
But her charmed life began to fall apart in 2015, when her father and mother, Linda Morrow, were indicted on federal insurance fraud charges in a well-publicized case. In 2017, the couple fled to Israel in an attempt to escape criminal prosecution, but later they were both arrested and returned to the United States to face prison sentences.
The legal woes of Morrow’s parents, later compounded by marital problems related to the failure of her husband’s business, took a heavy toll on Morrow. She was in her early 30s when the trouble with her parents started, and she was working 16-hour days to build a private medical practice, with two small children at home. By the end of 2019, she was severely depressed and turning increasingly to alcohol. Then, the loss of her admitting privileges at a large Los Angeles hospital due to inadequate medical record-keeping shattered what remained of her self-confidence.
Morrow, reflecting on her experience, said the very strengths that propel doctors through medical school and keep them going in their careers can foster a sense of denial. “We are so strong that our strength is our greatest threat. Our power is our powerlessness,” she said. Morrow ignored all the flashing yellow lights and even the red light beyond which serious trouble lay: “I blew through all of it, and I fell off the cliff.”
By late 2020, no longer working, bedridden by depression, and drinking to excess, she realized she could no longer will her way through: “I finally said to my husband, ‘I need help.’ He said, ‘I know you do.’”
Ultimately, she packed herself off to a private residential treatment center in Texas. Now sober for 21 months, Morrow said the privacy of the addiction treatment she chose was invaluable because it shielded her from professional scrutiny.
“I didn’t have to feel naked and judged,” she said.
Morrow said her privacy concerns would make her reluctant to join a state program like the one being considered by the medical board.
Physician Privacy vs. Patient Protection
The proposed regulations would spare doctors in the program who were not under board discipline from public disclosure as long as they stayed sober and complied with all the requirements, generally including random drug tests, attendance at group sessions, and work-site monitoring. If the program put a restriction on a doctor’s medical license, it would be posted on the medical board’s website, but without mentioning the doctor’s participation in the program.
Yet even that might compromise a doctor’s career since “having a restricted license for unspecified reasons could have many enduring personal and professional implications, none positive,” said Tracy Zemansky, a clinical psychologist and president of the Southern California division of Pacific Assistance Group, which provides support and monitoring for physicians.
Zemansky and others say doctors, just like anyone else, are entitled to medical privacy under federal law, as long as they haven’t caused harm.
Many who work in addiction medicine also criticized the proposed new program for not including mental health problems, which often go hand in hand with addiction and are covered by physician health programs in other states.
“To forgo mental health treatment, I think, is a grave mistake,” Morrow said. For her, depression and alcoholism were inseparable, and the residential program she attended treated her for both.
Another point of contention is money. Under the current proposal, doctors would bear all the costs of the program.
The initial clinical evaluation, plus the regular random drug tests, group sessions, and monitoring at their work sites could cost participants over $27,000 a year on average, according to estimates posted by the medical board. And if they were required to go for 30-day inpatient treatment, that would add an additional $40,000 — plus nearly $36,000 in lost wages.
People who work in the field of addiction medicine believe that is an unfair burden. They note that most programs for physicians in other states have outside funding to reduce the cost to participants.
“The cost should not be fully borne by the doctors, because there are many other people that are benefiting from this, including the board, malpractice insurers, hospitals, the medical association,” said Greg Skipper, a semi-retired addiction medicine doctor who ran Alabama’s state physician health program for 12 years. In Alabama, he said, those institutions contribute to the program, significantly cutting the amount doctors have to pay.
The treatment program that Morrow attended in spring of 2021, at The Menninger Clinic in Houston, cost $80,000 for a six-week stay, which was covered by a concerned family member. “It saved my life,” she said.
Though Morrow had difficulty maintaining her sobriety in the first year after treatment, she has now been sober since April 2, 2022. These days, Morrow regularly attends therapy and Alcoholics Anonymous and has pivoted to become an addiction medicine doctor.
“I am a better doctor today because of my experience — no question,” Morrow said. “I am proud to be a doctor who’s an alcoholic in recovery.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Dr. Greger’s Anti-Aging Eight
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Greger’s Anti-Aging Eight

This is Dr. Michael Greger. We’ve featured him before: Brain Food? The Eyes Have It!
This time, we’re working from his latest book, the excellent “How Not To Age”, which we reviewed all so recently. It is very information-dense, but we’re going to be focussing on one part, his “anti-aging eight”, that is to say, eight interventions he rates the most highly to slow aging in general (other parts of the book pertained to slowing eleven specific pathways of aging, or preserving specific bodily functions against aging, for example).
Without further ado, his “anti-aging eight” are…
- Nuts
- Greens
- Berries
- Xenohormesis & microRNA manipulation
- Prebiotics & postbiotics
- Caloric restriction / IF
- Protein restriction
- NAD+
As you may have noticed, some of these are things might appear already on your grocery shopping list; others don’t seem so “household”. Let’s break them down:
Nuts, greens, berries
These are amongst the most nutrient-dense and phytochemical-useful parts of the diet that Dr. Greger advocates for in his already-famous “Dr. Greger’s Daily Dozen”.
For brevity, we’ll not go into the science of these here, but will advise you: eat a daily portion of nuts, a daily portion of berries, and a couple of daily portions of greens.
Xenohormesis & microRNA manipulation
You might, actually, have these on your grocery shopping list too!
Hormesis, you may recall from previous editions of 10almonds, is about engaging in a small amount of eustress to trigger the body’s self-strengthening response, for example:
Xenohormesis is about getting similar benefits, second-hand.
For example, plants that have been grown to “organic” standards (i.e. without artificial pesticides, herbicides, fertilizers) have had to adapt to their relatively harsher environment by upping their levels of protective polyphenols and other phytochemicals that, as it turns out, are as beneficial to us as they are to the plants:
Hormetic Effects of Phytochemicals on Health and Longevity
Additionally, the flip side of xenohormesis is that some plant compounds can themselves act as a source of hormetic stress that end up bolstering us. For example:
In essence, it’s not just that it has anti-oxidant effect; it also provides a tiny oxidative-stress immunization against serious sources of oxidative stress—and thus, aging.
MicroRNA manipulation is, alas, too complex to truly summarize an entire chapter in a line or two, but it has to do with genetic information from the food that we eat having a beneficial or deleterious effect to our own health:
Diet-derived microRNAs: unicorn or silver bullet?
A couple of quick takeaways (out of very many) from Dr. Greger’s chapter on this is to spring for the better quality olive oil, and skip the cow’s milk:
- Impact of Phenol-Enriched Virgin Olive Oils on the Postprandial Levels of Circulating microRNAs Related to Cardiovascular Disease
- MicroRNA exosomes of pasteurized milk: potential pathogens of Western diseases
Prebiotics & Postbiotics
We’re short on space, so we’ll link you to a previous article, and tell you that it’s important against aging too:
Making Friends With Your Gut (You Can Thank Us Later)
An example of how one of Dr. Greger’s most-recommended postbiotics helps against aging, by the way:
- The mitophagy activator urolithin A is safe and induces a molecular signature of improved mitochondrial and cellular health in humans
- Urolithin A improves muscle strength, exercise performance, and biomarkers of mitochondrial health in a randomized trial in middle-aged adults
(Urolithin can be found in many plants, and especially those containing tannins)
See also: How to Make Urolithin Postbiotics from Tannins
Caloric restriction / Intermittent fasting
This is about lowering metabolic load and promoting cellular apoptosis (programmed cell death; sounds bad; is good) and autophagy (self-consumption; again, sounds bad; is good).
For example, he cites the intermittent fasters’ 46% lower risk of dying in the subsequent years of follow-up in this longitudinal study:
For brevity we’ll link to our previous IF article, but we’ll revisit caloric restriction in a main feature on of these days:
Fasting Without Crashing? We sort the science from the hype!
Dr. Greger favours caloric restriction over intermittent fasting, arguing that it is easier to adhere to and harder to get wrong if one has some confounding factor (e.g. diabetes, or a medication that requires food at certain times, etc). If adhered to healthily, the benefits appear to be comparable for each, though.
Protein restriction
In contrast to our recent main feature Protein vs Sarcopenia, in which that week’s featured expert argued for high protein consumption levels, protein restriction can, on the other hand, have anti-aging effects. A reminder that our body is a complex organism, and sometimes what’s good for one thing is bad for another!
Dr. Greger offers protein restriction as a way to get many of the benefits of caloric restriction, without caloric restriction. He further notes that caloric restriction without protein restriction doesn’t decrease IGF-1 levels (a marker of aging).
However, for FGF21 levels (these are good and we want them higher to stay younger), what matters more than lowering proteins in general is lowering levels of the amino acid methionine—found mostly in animal products, not plants—so the source of the protein matters:
For example, legumes deliver only 5–10% of the methionine that meat does, for the same amount of protein, so that’s a factor to bear in mind.
NAD+
This is about nicotinamide adenine dinucleotide, or NAD+ to its friends.
NAD+ levels decline with age, and that decline is a causal factor in aging, and boosting the levels can slow aging:
Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
Can we get NAD+ from food? We can, but not in useful quantities or with sufficient bioavailability.
Supplements, then? Dr. Greger finds the evidence for their usefulness lacking, in interventional trials.
How to boost NAD+, then? Dr. Greger prescribes…
Exercise! It boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
Another study on resistance training found the same 127% boost:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: