In the Realm of Hungry Ghosts – by Dr. Gabor Maté
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books by Dr. Maté before, and this one’s about addiction. We’ve reviewed books about addiction before too, so what makes this one different?
Wow, is this one so different. Most books about addiction are about “beating” it. Stop drinking, quit sugar, etc. And, that’s all well and good. It is definitely good to do those things. But this one’s about understanding it, deeply. Because, as Dr. Maté makes very clear, “there, but for the grace of epigenetics and environmental factors, go we”.
Indeed, most of us will have addictions; they’re (happily) just not too problematic for most of us, being either substances that are not too harmful (e.g. coffee), or behavioral addictions that aren’t terribly impacting our lives (e.g. Dr. Maté’s compulsion to keep buying more classical music, which he then tries to hide from his wife).
The book does also cover a lot of much more serious addictions, the kind that have ruined lives, and the kind that definitely didn’t need to, if people had been given the right kind of help—instead of, all too often, they got the opposite.
Perhaps the greatest value of this book is that; understanding what creates addiction in the first place, what maintains it, and what help people actually need.
Bottom line: if you’d like more insight into the human aspect of addiction without getting remotely wishy-washy, this book is probably the best one out there.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Menopause Does To The Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
World Menopause Day: Menopause & Cardiovascular Disease Risk
Today, the 18th of October, is World Menopause Day.
The theme for this year is cardiovascular disease (CVD), and if your first reaction is to wonder what that has to do with the menopause, then this is the reason why it’s being featured. Much of the menopause and its effects are shrouded in mystery; not because of a lack of science (though sometimes a bit of that too), but rather, because it is popularly considered an unimportant, semi-taboo topic.
So, let’s be the change we want to see, and try to fix that!
What does CVD have to do with the menopause?
To quote Dr. Anjana Nair:
❝The metabolic and clinical factors secondary to menopause, such as dyslipidemia, insulin resistance, fat redistribution and systemic hypertension, contribute to the accelerated risk for cardiovascular aging and disease.
Atherosclerosis appears to be the end result of the interaction between cardiovascular risk factors and their accentuation during the perimenopausal period.
The increased cardiovascular risk in menopause stems from the exaggerated effects of changing physiology on the cardiovascular system.❞
Source: Cardiovascular Changes in Menopause
See also: Menopause-associated risk of cardiovascular disease
Can we do anything about it?
Yes, we can! Here be science:
- Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association
- Cardiovascular risk in menopausal women and our evolving understanding of menopausal hormone therapy: risks, benefits, and current guidelines for use
This (in few words: get your hormone levels checked, and consider HRT if appropriate) is consistent with the advice from gynecologist Dr. Jen Gunter, whom we featured back in August:
What You Should Have Been Told About The Menopause Beforehand
What about lifestyle changes?
We definitely can do some good things; here’s what the science has to say:
- Mediterranean diet: yes, evidence-based
- High soy consumption: mixed evidence, unclear. So, eat it if you want, don’t if you don’t.
- Supplements e.g. vitamins and minerals: yes, evidence-based.
- Supplements e.g. herbal preparations: many may help, but watch out for adverse interactions with meds. Check with your pharmacist or doctor.
- Supplements; specifically CBD: not enough evidence yet
- Exercise: yes, evidence-based—especially low-impact high-resistance training, for bone strength, as well as regular moderate-intensity exercise and/or High-Intensity Interval Training, to guard against CVD.
For a full low-down on all of these:
Revealing the evidence-based lifestyle solutions to managing your menopause symptoms
Want to know more?
You can get the International Menopause Society’s free downloadable booklet here:
Menopause & Cardiovascular Disease: What Women Need To Know
You may also like our previous main feature:
What Does “Balance Your Hormones” Even Mean?
Take care!
Share This Post
-
How Much Difference Do Probiotic Supplements Make, Really?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How Much Difference Do Probiotic Supplements Make?
There are three main things that get talked about with regard to gut health:
- Prebiotics (fibrous foods)
- Probiotics (things containing live “good” bacteria)
- Postbiotics (things to help them thrive)
Today we’ll be talking about probiotics, but if you’d like a refresher on general gut health, here’s our previous main feature:
Making Friends With Your Gut (You Can Thank Us Later)
What bacteria are in probiotics?
There are many kinds, but the most common by far are Lactobacillus sp. and Bifidobacteria sp.
Taxonomical note: “sp.” just stands for “species”. The first name is the genus, which contains a plurality of (sometimes, many) species.
Lactobacillus acidophilus, also written L. acidophilus, is a common species of Lactobacillus sp. in probiotics.
Bifidobacterium bifidum, also written B. bifidum, is a common species of Bifidobacterium sp. in probiotics.
What difference do they make?
First, and perhaps counterintuitively, putting more bacteria into your gut has a settling effect on the digestion. In particular, probiotics have been found effective against symptoms of IBS and ulcerative colitis, (but not Crohn’s):
- Probiotics in Irritable Bowel Syndrome: An Up-to-Date Systematic Review
- The role of probiotics in the prevention and treatment of IBS and other related diseases: a systematic review of randomized human clinical trials
- Safety and Potential Role of Lactobacillus rhamnosus GG Administration as Monotherapy in Ulcerative Colitis Patients
- Probiotics for induction of remission in Crohn’s disease
Probiotics are also helpful against diarrhea, including that caused by infections and/or antibiotics, as well as to reduce antibiotic resistance:
- Probiotics for the prevention of Clostridium difficile-associated diarrhea in adults and children
- Probiotic approach to prevent antibiotic resistance
Probiotics also boost the immune system outside of the gut, too, for example reducing the duration of respiratory infections:
You may recallthe link between gut health and brain health, thanks in large part to the vagus nerve connecting the two:
The Brain-Gut Highway: A Two-Way Street
No surprises, then, that probiotics benefit mental health. See:
- The effects of probiotics on mental health and hypothalamic-pituitary-adrenal axis: A randomized, double-blind, placebo-controlled trial
- A randomized controlled trial to test the effect of multispecies probiotics on cognitive reactivity to sad mood
- Clinical and metabolic response to probiotic administration in patients with major depressive disorder: A randomized, double-blind, placebo-controlled trial
There are so many kinds; which should I get?
Diversity is good, so more kinds is better. However, if you have specific benefits you’d like to enjoy, you may want to go stronger on particular strains:
Choosing an appropriate probiotic product for your patient: An evidence-based practical guide
Where can I get them?
We don’t sell them, but here’s an example product on Amazon, for your convenience.
Alternatively, you can check out today’s sponsor, who also sell such; we recommend comparing products and deciding which will be best for you
Enjoy!
Share This Post
-
How To En-Joy Life (With Long-Term Benefits)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
New Year’s Dissolutions?
We have talked previously about:
The Science Of New Year’s Pre-Resolutions
…and here we are now at the end of the first week of January; how’s it going?
Hopefully, based on that article, it’s been going just great since December! For most people, statistically speaking, it hasn’t.
Around now is typically when many people enter the “bargaining” stage of New Year’s Resolutions, which at this point are often in serious danger of becoming New Year’s Dissolutions.
What’s important, really?
When trying to juggle potentially too many new items, it’s important to be able to decide where to focus one’s efforts in the case of needing to drop a ball or two.
First, the laziest way…
The path of least resistance
This is perhaps most people’s go-to. It, without too much thought, drops whatever feels most onerous, and continues with what seems easiest.
This is not a terrible approach, because what we enjoy, we will be more likely to continue. But it can be improved upon, while still getting that benefit.
Marie Kondo your
resolutionsvaluesInstead of throwing out the new habits that “don’t spark joy”, ask yourself:
“What brings me joy?”
…because often, the answer is something that’s a result of a thing that didn’t “spark joy” directly. Many things in life involve delayed gratification.
Let’s separate the [unwanted action] from the [wanted result] for a moment.
Rather than struggling on with something unpleasant for the hope of joy at the end of the rainbow, though, give yourself permission to improve the middle bit.
For example, if the idea of having lots of energy and good cardiovascular fitness is what prompted you to commit to those 6am runs each morning (but they’re not actually joyous in your experience), what would be more fun and still give you the same benefit?
Now that you know “having lots of energy and good CV fitness” is what sparks joy, not “getting up to run at 6am”, you can change lanes without pulling off the highway entirely.
Maybe a dance class will be more your speed, for example.
The key here is: you’ll have changed your resolution, without breaking it in any way that mattered
Want more ways to keep on track without burning out?
Who doesn’t? So, check out:
How To Keep On Keeping On… Long Term!
Enjoy!
Share This Post
Related Posts
-
Women are less likely to receive CPR than men. Training on manikins with breasts could help
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
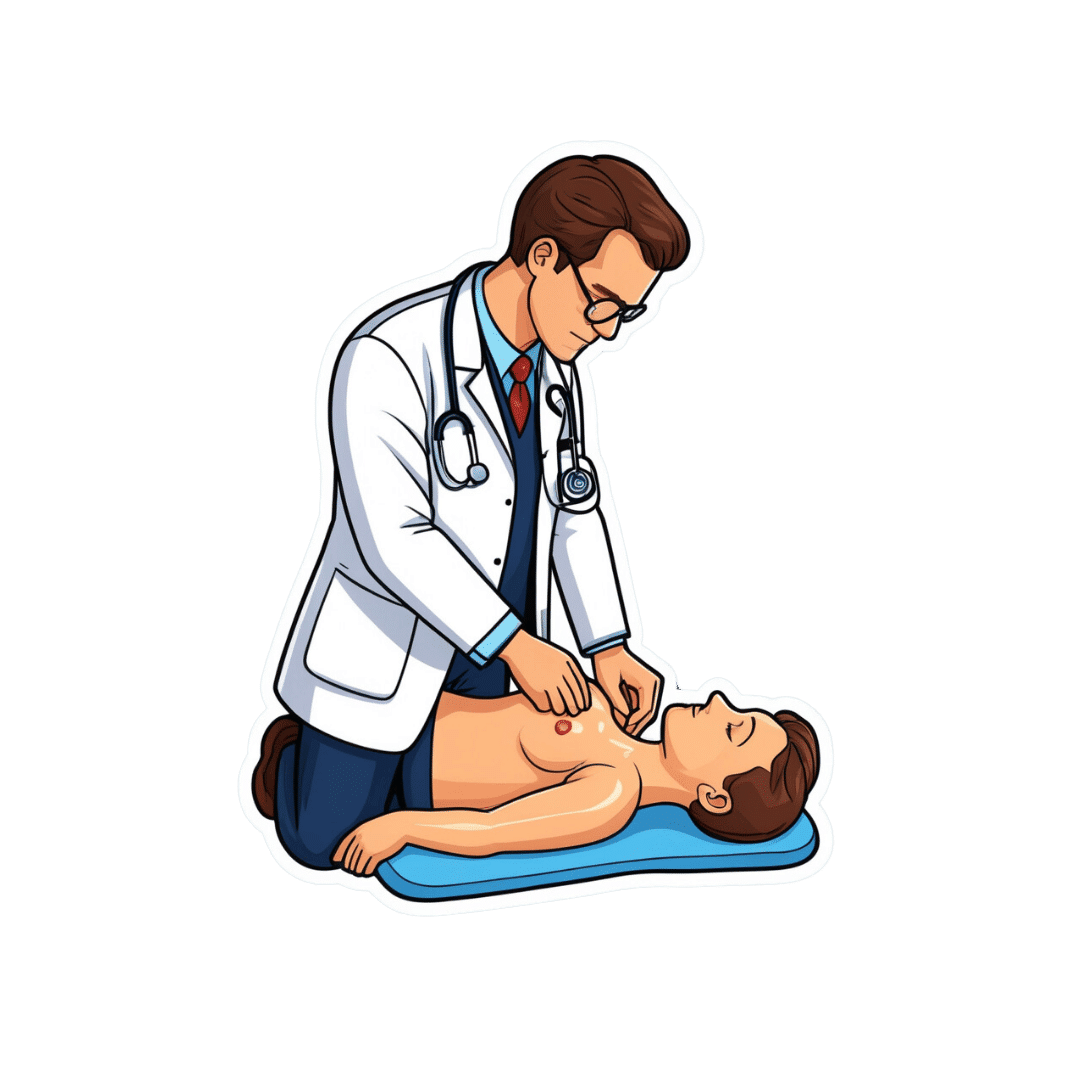
If someone’s heart suddenly stops beating, they may only have minutes to live. Doing CPR (cardiopulmonary resusciation) can increase their chances of survival. CPR makes sure blood keeps pumping, providing oxygen to the brain and vital organs until specialist treatment arrives.
But research shows bystanders are less likely to intervene to perform CPR when that person is a woman. A recent Australian study analysed 4,491 cardiac arrests between 2017–19 and found bystanders were more likely to give CPR to men (74%) than women (65%).
Could this partly be because CPR training dummies (known as manikins) don’t have breasts? Our new research looked at manikins available worldwide to train people in performing CPR and found 95% are flat-chested.
Anatomically, breasts don’t change CPR technique. But they may influence whether people attempt it – and hesitation in these crucial moments could mean the difference between life and death.
Pixel-Shot/Shutterstock Heart health disparities
Cardiovascular diseases – including heart disease, stroke and cardiac arrest – are the leading cause of death for women across the world.
But if a woman has a cardiac arrest outside hospital (meaning her heart stops pumping properly), she is 10% less likely to receive CPR than a man. Women are also less likely to survive CPR and more likely to have brain damage following cardiac arrests.
Bystanders are less likely to intervene if a woman needs CPR, compared to a man. doublelee/Shutterstock These are just some of many unequal health outcomes women experience, along with transgender and non-binary people. Compared to men, their symptoms are more likely to be dismissed or misdiagnosed, or it may take longer for them to receive a diagnosis.
Bystander reluctance
There is also increasing evidence women are less likely to receive CPR compared to men.
This may be partly due to bystander concerns they’ll be accused of sexual harassment, worry they might cause damage (in some cases based on a perception women are more “frail”) and discomfort about touching a woman’s breast.
Bystanders may also have trouble recognising a woman is experiencing a cardiac arrest.
Even in simulations of scenarios, researchers have found those who intervened were less likely to remove a woman’s clothing to prepare for resuscitation, compared to men. And women were less likely to receive CPR or defibrillation (an electric charge to restart the heart) – even when the training was an online game that didn’t involve touching anyone.
There is evidence that how people act in resuscitation training scenarios mirrors what they do in real emergencies. This means it’s vital to train people to recognise a cardiac arrest and be prepared to intervene, across genders and body types.
Skewed to male bodies
Most CPR training resources feature male bodies, or don’t specify a sex. If the bodies don’t have breasts, it implies a male default.
For example, a 2022 study looking at CPR training across North, Central and South America, found most manikins available were white (88%), male (94%) and lean (99%).
It’s extremely rare for a manikin to have breasts or a larger body. M Isolation photo/Shutterstock These studies reflect what we see in our own work, training other health practitioners to do CPR. We have noticed all the manikins available to for training are flat-chested. One of us (Rebecca) found it difficult to find any training manikins with breasts.
A single manikin with breasts
Our new research investigated what CPR manikins are available and how diverse they are. We identified 20 CPR manikins on the global market in 2023. Manikins are usually a torso with a head and no arms.
Of the 20 available, five (25%) were sold as “female” – but only one of these had breasts. That means 95% of available CPR training manikins were flat-chested.
We also looked at other features of diversity, including skin tone and larger bodies. We found 65% had more than one skin tone available, but just one was a larger size body. More research is needed on how these aspects affect bystanders in giving CPR.
Breasts don’t change CPR technique
CPR technique doesn’t change when someone has breasts. The barriers are cultural. And while you might feel uncomfortable, starting CPR as soon as possible could save a life.
Signs someone might need CPR include not breathing properly or at all, or not responding to you.
To perform effective CPR, you should:
- put the heel of your hand on the middle of their chest
- put your other hand on the top of the first hand, and interlock fingers (keep your arms straight)
- press down hard, to a depth of about 5cm before releasing
- push the chest at a rate of 100-120 beats per minute (you can sing a song) in your head to help keep time!)
https://www.youtube.com/embed/Plse2FOkV4Q?wmode=transparent&start=94 An example of how to do CPR – with a flat-chested manikin.
What about a defibrillator?
You don’t need to remove someone’s bra to perform CPR. But you may need to if a defibrillator is required.
A defibrillator is a device that applies an electric charge to restore the heartbeat. A bra with an underwire could cause a slight burn to the skin when the debrillator’s pads apply the electric charge. But if you can’t remove the bra, don’t let it delay care.
What should change?
Our research highlights the need for a range of CPR training manikins with breasts, as well as different body sizes.
Training resources need to better prepare people to intervene and perform CPR on people with breasts. We also need greater education about women’s risk of getting and dying from heart-related diseases.
Jessica Stokes-Parish, Assistant Professor in Medicine, Bond University and Rebecca A. Szabo, Honorary Senior Lecturer in Critical Care and Obstetrics, Gynaecology and Newborn Health, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Artichoke vs Asparagus – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing artichoke to asparagus, we picked the artichoke.
Why?
Both are great and it was close!
In terms of macros, artichoke has a little more protein and around 3x the carbs and fiber: the ratio there means that both vegetables have an identical glycemic index, so we’ll go with the “most food per food” reckoning of nutritional density, and call it for the artichoke.
When it comes to vitamins, artichoke has more of vitamins B3, B5, B6, B7, B9, C, and choline, while asparagus has more of vitamins A, B1, B2, E, and K. Both very respectable nutritional sets, but artichoke gets a marginal 6:5 win on strength of numbers.
In the category of minerals, artichoke has more calcium, copper, magnesium, manganese, phosphorus, and potassium, while asparagus has more iron, selenium, and zinc. A clearer 6:3 win for artichoke this time.
Once again, both of these are great foods, so by all means enjoy either or both. But if you’re looking for the nutritionally densest option, it’s the artichoke!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Menopause Does To The Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
World Menopause Day: Menopause & Cardiovascular Disease Risk
Today, the 18th of October, is World Menopause Day.
The theme for this year is cardiovascular disease (CVD), and if your first reaction is to wonder what that has to do with the menopause, then this is the reason why it’s being featured. Much of the menopause and its effects are shrouded in mystery; not because of a lack of science (though sometimes a bit of that too), but rather, because it is popularly considered an unimportant, semi-taboo topic.
So, let’s be the change we want to see, and try to fix that!
What does CVD have to do with the menopause?
To quote Dr. Anjana Nair:
❝The metabolic and clinical factors secondary to menopause, such as dyslipidemia, insulin resistance, fat redistribution and systemic hypertension, contribute to the accelerated risk for cardiovascular aging and disease.
Atherosclerosis appears to be the end result of the interaction between cardiovascular risk factors and their accentuation during the perimenopausal period.
The increased cardiovascular risk in menopause stems from the exaggerated effects of changing physiology on the cardiovascular system.❞
Source: Cardiovascular Changes in Menopause
See also: Menopause-associated risk of cardiovascular disease
Can we do anything about it?
Yes, we can! Here be science:
- Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association
- Cardiovascular risk in menopausal women and our evolving understanding of menopausal hormone therapy: risks, benefits, and current guidelines for use
This (in few words: get your hormone levels checked, and consider HRT if appropriate) is consistent with the advice from gynecologist Dr. Jen Gunter, whom we featured back in August:
What You Should Have Been Told About The Menopause Beforehand
What about lifestyle changes?
We definitely can do some good things; here’s what the science has to say:
- Mediterranean diet: yes, evidence-based
- High soy consumption: mixed evidence, unclear. So, eat it if you want, don’t if you don’t.
- Supplements e.g. vitamins and minerals: yes, evidence-based.
- Supplements e.g. herbal preparations: many may help, but watch out for adverse interactions with meds. Check with your pharmacist or doctor.
- Supplements; specifically CBD: not enough evidence yet
- Exercise: yes, evidence-based—especially low-impact high-resistance training, for bone strength, as well as regular moderate-intensity exercise and/or High-Intensity Interval Training, to guard against CVD.
For a full low-down on all of these:
Revealing the evidence-based lifestyle solutions to managing your menopause symptoms
Want to know more?
You can get the International Menopause Society’s free downloadable booklet here:
Menopause & Cardiovascular Disease: What Women Need To Know
You may also like our previous main feature:
What Does “Balance Your Hormones” Even Mean?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: