10,000 Steps, 30 Days, 4 Changes
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ariel wasn’t the most active person, and took on a “30 day challenge” to do the commonly-prescribed 10,000 steps per day—without adjusting her diet or doing any other exercise. How much of a difference does it make, really?
Stepping onwards
The 4 main things that she found changed for her weren’t all what she expected:
- Weight loss yes, but only marginally: she lost 3 lbs in a month, which did nevertheless make a visible difference. We might hypothesize that part of the reason for the small weight loss and yet visible difference is that she gained a little muscle, and the weight loss was specifically shifting away from a cortisol-based fat distribution, to a more healthy fat distribution.
- Different eating habits: she felt less hungry and craved less sugar. This likely has less to do with calorie consumption, and more to do with better insulin signalling.
- Increased energy and improved mood: these are going together in one item, because she said “4 things”, but really they are two related things. So, consider one of them a bonus item! In any case, she felt more energized and productive, and less reliant on caffeine.
- Improved sleep: or rather, at first, disrupted sleep, and then slept better and stayed better. A good reminder that changes for the better don’t always feel better in the first instance!
To hear about it in her own words, and see the before and after pictures, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Rainbow Roasted Potato Salad
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This salad has potatoes in it, but it’s not a potato salad as most people know it. The potatoes are roasted, but in a non-oily-dressing, that nevertheless leaves them with an amazing texture—healthy and delicious; the best of both worlds. And the rest? We’ve got colorful vegetables, we’ve got protein, we’ve got seasonings full of healthy spices, and more.
You will need
- 1½ lbs new potatoes (or any waxy potatoes; sweet potato is also a great option; don’t peel them, whichever you choose) cut into 1″ chunks
- 1 can / 1 cup cooked cannellini beans (or your preferred salad beans)
- 1 carrot, grated
- 2 celery stalks, finely chopped
- 3 spring onions, finely chopped
- ½ small red onion, finely sliced
- 2 tbsp white wine vinegar
- 1 tbsp balsamic vinegar
- 1 tbsp lemon juice
- 1 tbsp nutritional yeast
- 1 tsp garlic powder
- 1 tsp black pepper
- ½ tsp red chili powder
- We didn’t forget salt; it’s just that with the natural sodium content of the potatoes plus the savory flavor-enhancing properties of the nutritional yeast, it’s really not needed here. Add if you feel strongly about it, opting for low-sodium salt, or MSG (which has even less sodium).
- To serve: 1 cup basil pesto (we’ll do a recipe one of these days; meanwhile, store-bought is fine, or you can use the chermoula we made the other day, ignoring the rest of that day’s recipe and just making the chermoula component)
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven as hot as it goes!
2) Combine the potatoes, white wine vinegar, nutritional yeast, garlic powder, black pepper, and red chili powder, mixing thoroughly (but gently!) to coat.
3) Spread the potatoes on a baking tray, and roast in the middle of the oven (for best evenness of cooking); because of the small size of the potato chunks, this should only take about 25 minutes (±5mins depending on your oven); it’s good to turn them halfway through, or at least jiggle them if you don’t want to do all that turning.
4) Allow to cool while still on the baking tray (this allows the steam to escape immediately, rather than the steam steaming the other potatoes, as it would if you put them in a bowl).
5) Now put them in a serving bowl, and mix in the beans, vegetables, balsamic vinegar, and lemon juice, mixing thoroughly but gently
6) Add generous lashings of the pesto to serve; it should be gently mixed a little too, so that it’s not all on top.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- White Potato vs Sweet Potato – Which is Healthier?
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
How To Grow In Comfort
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How To Grow (Without Leaving Your Comfort Zone)
“You have to get out of your comfort zone!” we are told, from cradle to grave.
When we are young, we are advised (or sometimes more forcefully instructed!) that we have to try new things. In our middle age, we are expected to be the world’s greatest go-getters, afraid of nothing and always pushing limits. And when we are old, people bid us “don’t be such a dinosaur”.
It is assumed, unquestioned, that growth can only occur through hardship and discomfort.
But what if that’s a discomforting lie?
Butler (2023) posited an idea: “We never achieve success faster and with less effort than when we are in our comfort zone”
Her words are an obvious callback to the ideas of Csikszentmihalyi (1970) in the sense of “flow”, in the sense in which that word is used in psychology.
Flow is: when a person is in a state of energized focus, full involvement, and enjoyment of an activity.
As a necessary truth (i.e: a function of syllogistic logic), the conditions of “in a state of flow” and “outside of one’s comfort zone” cannot overlap.
From there, we can further deduce (again by simple logic) that if flow can be found, and/but cannot be found outside of the comfort zone, then flow can only be found within the comfort zone.
That is indeed comforting, but what about growth?
Imagine you’ve never gone camping in your life, but you want to get outside of your comfort zone, and now’s the time to do it. So, you check out some maps of the Yukon, purchase some camping gear, and off you go into the wilderness. In the event that you survive to report it, you will indeed be able to say “it was not comfortable”.
But, did growth occur? Maybe, but… it’s a folly to say “what doesn’t kill us makes us stronger” as a reason to pursue such things. Firstly, there’s a high chance it may kill us. Secondly, what doesn’t kill us often leaves us incredibly weakened and vulnerable.
When Hannibal famously took his large army of mostly African mercenaries across the Alps during winter to march on Rome from the other side, he lost most of his men on the way, before proceeding to terrorize Northern Italy convincingly with the small remainder. But! Their hard experience hadn’t made them stronger; it had just removed the weaker soldiers, making the resultant formations harder to break.
All this to say, please do not inflict hardship and discomfort and danger in the hopes it’ll make you stronger; it will probably do the opposite.
But…
If, instead of wilderness trekking in the Yukon…
- You start off with a camper van holiday, then you’ll be taking a fair amount of your comfort with you. In effect, you will be stretching and expanding your comfort zone without leaving it.
- Then maybe another year you might try camping in a tent on a well-catered camping site.
- Later, you might try “roughing it” at a much less well-catered camping site.
- And so on.
Congratulations, you have tried new things and undergone growth, taking your comfort zone with you all the way!
This is more than just “easing yourself into” something
It really is about taking your comfort with you too. If you want to take up running, don’t ask “how can I run just a little bit first” or “how can I make it easier” (well, feel free to ask those things too, but) ask yourself: how can I bring my comfort with me? Comfortable shoes, perhaps, an ergonomic water bottle, shade for your head, maybe.
❝Any fool can rough it, but a good soldier can make himself comfortable in any circumstances❞
~ British Army maxim
This goes for more than just physical stuff, too
If you want to learn a new skill, the initial learning curve can be anxiety-inducing, especially if you are taking a course and worried about keeping up or “not being good enough”.
So, “secretly” study in advance, at your leisure, get yourself a head start. Find a degree of comfort in what you’ve learned so far, and then bring that comfort with you into your entry-level course that is now less intimidating.
Discomfort isn’t a badge of honor (and impedes growth)
Take that extra rest stop on the highway. Bring your favorite coffee with you. Use that walking stick, if it helps.
Whatever it takes to bring your comfort with you, bring it.
Trust us, you’ll get further that way.
Share This Post
-
NADᐩ Against Aging
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Nicotinamide adenine dinucleotide, or “NAD” to its friends, is a coenzyme produced in the human body (amongst other places), and it is critical for cellular energy metabolism, but there’s more to it than that.
Today we’ll be looking mostly at NAD+, of which the + indicates the positive formal charge of one of its nitrogen atoms. We won’t get too much into the chemistry of this, but we will mention that it’s a cofactor with NADH—the former accepting electrons and the latter donating electrons.
Both NAD+ and NADH are critical to good health, but we’re going to focus on NAD+ for the simple reason that it gets depleted with aging.
Note: it gets depleted with aging.
Chronological age is not so important here, but there is a direct relationship between biological aging and NAD+ depletion.
For example, healthy centenarians tend not to have depleted NAD+ levels. Further, its depletion (in those in whom it is depleted) is then a causal factor for many age-related diseases:
❝Remarkably, ageing is accompanied by a gradual decline in tissue and cellular NAD+ levels in multiple model organisms, including rodents and humans.
This decline in NAD+ levels is linked causally to numerous ageing-associated diseases, including cognitive decline, cancer, metabolic disease, sarcopenia and frailty.
Many of these ageing-associated diseases can be slowed down and even reversed by restoring NAD+ levels.❞
~ Dr. Rosalba Perrone et al.
Read in full: NAD+ metabolism and its roles in cellular processes during ageing
As for restoring those NADᐩ levels, that does help in interventional trials, whether by supplementing directly, or with NAD precursors*:
❝NAD+ levels steadily decline with age, resulting in altered metabolism and increased disease susceptibility.
Restoration of NAD+ levels in old or diseased animals can promote health and extend lifespan, prompting a search for safe and efficacious NAD-boosting molecules that hold the promise of increasing the body’s resilience, not just to one disease, but to many, thereby extending healthy human lifespan.❞
~ Dr. David Sinclair et al.
Read more: Therapeutic Potential of NAD-Boosting Molecules: The In Vivo Evidence
*There are actually also other NAD-boosting molecules besides NAD itself and its precursors. For example, the liver will not produce NADᐩ unless it has aminocarboxymuconate-semialdehyde decarboxylase (or “ACMSD”, to its friends), which limits the production of NADᐩ. Why, you ask? The theory is that it is a kind of evolutionary conservativism, much like not lighting a fire without the ability to put it out. In any case, taking ACMSD-blockers will thus result in an increased endogenous production of NADᐩ.
You can read about this here:
De novo NAD+ synthesis enhances mitochondrial function and improves health
Nor is taking supplements or drugs the only way to get more of it; there’s an enzyme nicotinamide phosphoribosyltransferase (“NAMPT”, to its friends) involved in the synthesis of NADᐩ, and exercise boosts levels by 127% (i.e., it more than doubles the levels), based on a modest three-week exercise bike regimen:
Skeletal muscle NAMPT is induced by exercise in humans
And to underline that point, another study found that resistance training (so, a different kind of exercise from that of the previous study) boosts levels of NADᐩ itself by the same 127%:
One way to get more out of NADᐩ
We’ll get straight to the point: it works very well paired with a senolytic agent, i.e. something that kills aging cells so that they get recycled sooner:
NAD+, Senolytics, or Pyruvate for Healthy Aging?
To read more about senolytics, check out:
Fisetin: The Anti-Aging Assassin
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
Is owning a dog good for your health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Australia loves dogs. We have one of the highest rates of pet ownership in the world, and one in two households has at least one dog.
But are they good for our health?
Mental health is the second-most common reason cited for getting a dog, after companionship. And many of us say we “feel healthier” for having a dog – and let them sleep in our bedroom.
Here’s what it means for our physical and mental health to share our homes (and doonas) with our canine companions.
Pogodina Natalia/Shutterstock Are there physical health benefits to having a dog?
Having a dog is linked to lower risk of death over the long term. In 2019, a systematic review gathered evidence published over 70 years, involving nearly four million individual medical cases. It found people who owned a dog had a 24% lower risk of dying from any cause compared to those who did not own a dog.
Having a dog may help lower your blood pressure through more physical activity. Barnabas Davoti/Pexels Dog ownership was linked to increased physical activity. This lowered blood pressure and helped reduce the risk of stroke and heart disease.
The review found for those with previous heart-related medical issues (such as heart attack), living with a dog reduced their subsequent risk of dying by 35%, compared to people with the same history but no dog.
Another recent UK study found adult dog owners were almost four times as likely to meet daily physical activity targets as non-owners. Children in households with a dog were also more active and engaged in more unstructured play, compared to children whose family didn’t have a dog.
Exposure to dirt and microbes carried in from outdoors may also strengthen immune systems and lead to less use of antibiotics in young children who grow up with dogs.
Children in households with a dog were often more active. Maryshot/Shutterstock Health risks
However, dogs can also pose risks to our physical health. One of the most common health issues for pet owners is allergies.
Dogs’ saliva, urine and dander (the skin cells they shed) can trigger allergic reactions resulting in a range of symptoms, from itchy eyes and runny nose to breathing difficulties.
A recent meta-analysis pooled data from nearly two million children. Findings suggested early exposure to dogs may increase the risk of developing asthma (although not quite as much as having a cat does). The child’s age, how much contact they have with the dog and their individual risk all play a part.
Slips, trips and falls are another risk – more people fall over due to dogs than cats.
Having a dog can also expose you to bites and scratches which may become infected and pose a risk for those with compromised immune systems. And they can introduce zoonotic diseases into your home, including ring worm and Campylobacter, a disease that causes diarrhoea.
For those sharing the bed there is an elevated the risk of allergies and picking up ringworm. It may result in lost sleep, as dogs move around at night.
On the other hand some owners report feeling more secure while co-sleeping with their dogs, with the emotional benefit outweighing the possibility of sleep disturbance or waking up with flea bites.
Proper veterinary care and hygiene practices are essential to minimise these risks.
Many of us don’t just share a home with a dog – we let them sleep in our beds. Claudia Mañas/Unsplash What about mental health?
Many people know the benefits of having a dog are not only physical.
As companions, dogs can provide significant emotional support helping to alleviate symptoms of anxiety, depression and post-traumatic stress. Their presence may offer comfort and a sense of purpose to individuals facing mental health challenges.
Loneliness is a significant and growing public health issue in Australia.
In the dog park and your neighbourhood, dogs can make it easier to strike up conversations with strangers and make new friends. These social interactions can help build a sense of community belonging and reduce feelings of social isolation.
For older adults, dog walking can be a valuable loneliness intervention that encourages social interaction with neighbours, while also combating declining physical activity.
However, if you’re experiencing chronic loneliness, it may be hard to engage with other people during walks. An Australian study found simply getting a dog was linked to decreased loneliness. People reported an improved mood – possibly due to the benefits of strengthening bonds with their dog.
Walking a dog can make it easier to talk to people in your neighbourhood. KPegg/Shutterstock What are the drawbacks?
While dogs can bring immense joy and numerous health benefits, there are also downsides and challenges. The responsibility of caring for a dog, especially one with behavioural issues or health problems, can be overwhelming and create financial stress.
Dogs have shorter lifespans than humans, and the loss of a beloved companion can lead to depression or exacerbate existing mental health conditions.
Lifestyle compatibility and housing conditions also play a significant role in whether having a dog is a good fit.
The so-called pet effect suggests that pets, often dogs, improve human physical and mental health in all situations and for all people. The reality is more nuanced. For some, having a pet may be more stressful than beneficial.
Importantly, the animals that share our homes are not just “tools” for human health. Owners and dogs can mutually benefit when the welfare and wellbeing of both are maintained.
Tania Signal, Professor of Psychology, School of Health, Medical and Applied Sciences, CQUniversity Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fitness Freedom for Seniors – by Jackie Jacobs
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Exercise books often assume that either we are training for the Olympics, and most likely also that we are 20 years old. This one doesn’t.
Instead, we see a well-researched, well-organized, clearly-illustrated fitness plan with age in mind. Author Jackie Jacobs offers tips and advice for all levels, and a progressive week-by-week plan of 15-minute sessions. This way, we’re neither overdoing it nor slacking off; it’s a perfect balance.
The exercises are aimed at “all areas”, that is to say, improving cardiovascular fitness, balance, flexibility, and strength. It also gives some supplementary advice with regard to diet and suchlike, but the workouts are the real meat of the book.
Bottom line: if you’d like a robust, science-based exercise regime that’s tailored to seniors, this is the book for you.
Click here to check out Fitness Freedom for Seniors, and get yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Good (Or Bad) Health Starts With Your Blood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Blood Should Be Only Slightly Thicker Than Water
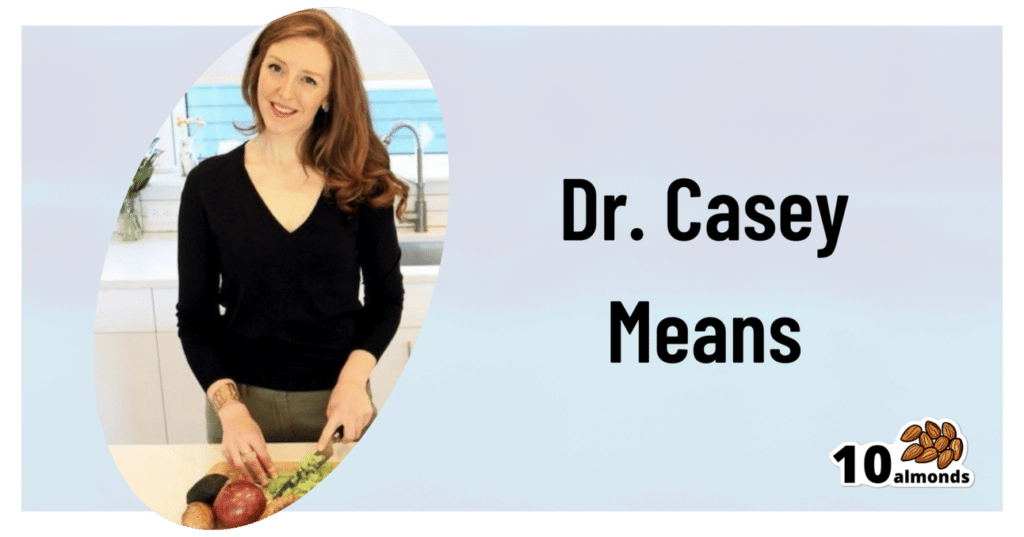
This is Dr. Casey Means, a physician, lecturer (mostly at Stanford), and CMO of a metabolic health company, Levels, as well as being Associate Editor of the International Journal of Diabetes Reversal and Prevention, where she serves alongside such names as Dr. Colin Campbell, Dr. Joel Fuhrman, Dr. Michael Greger, Dr. William Li, Dr. Dean Ornish, and you get the idea: it’s a star-studded cast.
What does she want us to know?
The big blood problem:
❝We’re spending 3.8 trillion dollars a year on healthcare costs in the U.S., and the reality is that people are getting sicker, fatter, and more depressed.
Over 50% of Americans have pre-diabetes or type 2 diabetes; it’s insane, that number should be close to zero.❞
~ Dr. Casey Means
Indeed, pre-diabetes and especially type 2 diabetes should be very avoidable in any wealthy nation.
Unfortunately, the kind of diet that avoids it tends to rely on having at least 2/3 of the following:
- Money
- Time
- Knowledge
For example:
- if you have money and time, you can buy lots of fresh ingredients without undue worry, and take the time to carefully prep and cook them
- if you have money and knowledge you can have someone else shop and cook for you, or at least get meal kits delivered
- if you have time and knowledge, you can actually eat very healthily on a shoestring budget
If you have all three, then the world’s your oyster mushroom steak sautéed in extra virgin olive oil with garlic and cracked black pepper served on a bed of Swiss chard and lashed with Balsamic vinegar.
However, many Americans aren’t in the happy position of having at least 2/3, and a not-insignificant portion of the population don’t even have 1/3.
As an aside: there is a food scientist and chef who’s made it her mission to educate people about food that’s cheap, easy, and healthy:
…but today is about Dr. Means, so, what does she suggest?
Know
thyselfthy blood sugarsDr. Means argues (reasonably; this is well-backed up by general scientific consensus) that much of human disease stems from the diabetes and pre-diabetes that she mentioned above, and so we should focus on that most of all.
Our blood sugar levels being unhealthy will swiftly lead to other metabolic disorders:
Heart disease and non-alcoholic fatty liver disease are perhaps first in line, but waiting in the wings are inflammation-mediated autoimmune disorders, and even dementia, because neuroinflammation is at least as bad as inflammation anywhere else, arguably worse, and our brain can only be as healthy as the blood that feeds it and takes things that shouldn’t be there away.
Indeed,
❝Alzheimer’s dementia is now being called type 3 diabetes because it’s so related to blood sugar❞
~ Dr. Casey Means
…which sounds like a bold claim, but it’s true, even if the name is not “official” yet, it’s well-established in professional circulation:
❝We conclude that the term “type 3 diabetes” accurately reflects the fact that AD represents a form of diabetes that selectively involves the brain and has molecular and biochemical features that overlap with both T1DM and T2DM❞
~ Dr. Suzanne M. de la Monte & Dr. Jack Wands
Read in full: Alzheimer’s Disease Is Type 3 Diabetes–Evidence Reviewed ← this is from the very respectable Journal of Diabetes Science and Technology.
What to do about it
Dr. Means suggests we avoid the “glucose roller-coaster” that most Americans are on, meaning dramatic sugar spikes, or to put it in sciencese: high glycemic variability.
This leads to inflammation, oxidative stress, glycation (where sugar sticks to proteins and DNA), and metabolic dysfunction. Then there’s the flipside: reactive hypoglycemia, a result of a rapid drop in blood sugar after a spike, can cause anxiety, fatigue, weakness/trembling, brain fog, and of course cravings. And so the cycle repeats.
But it doesn’t have to!
By taking it upon ourselves to learn about what causes our blood sugars to rise suddenly or gently, we can manage our diet and other lifestyle factors accordingly.
And yes, it’s not just about diet, Dr. Means tells us. While added sugar and refined carbohydrates or indeed the main drivers of glycemic variability, our sleep, movement, stress management, and even toxin exposure play important parts too.
One way to do this, that Dr. Means recommends, is with a continuous glucose monitor:
Track Your Blood Sugars For Better Personalized Health
Another way is to just apply principles that work for almost everyone:
10 Ways To Balance Blood Sugars
Want to know more from Dr. Means?
You might like her book:
Good Energy – by Dr. Casey Means
…which goes into this in far more detail than we have room to today.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: