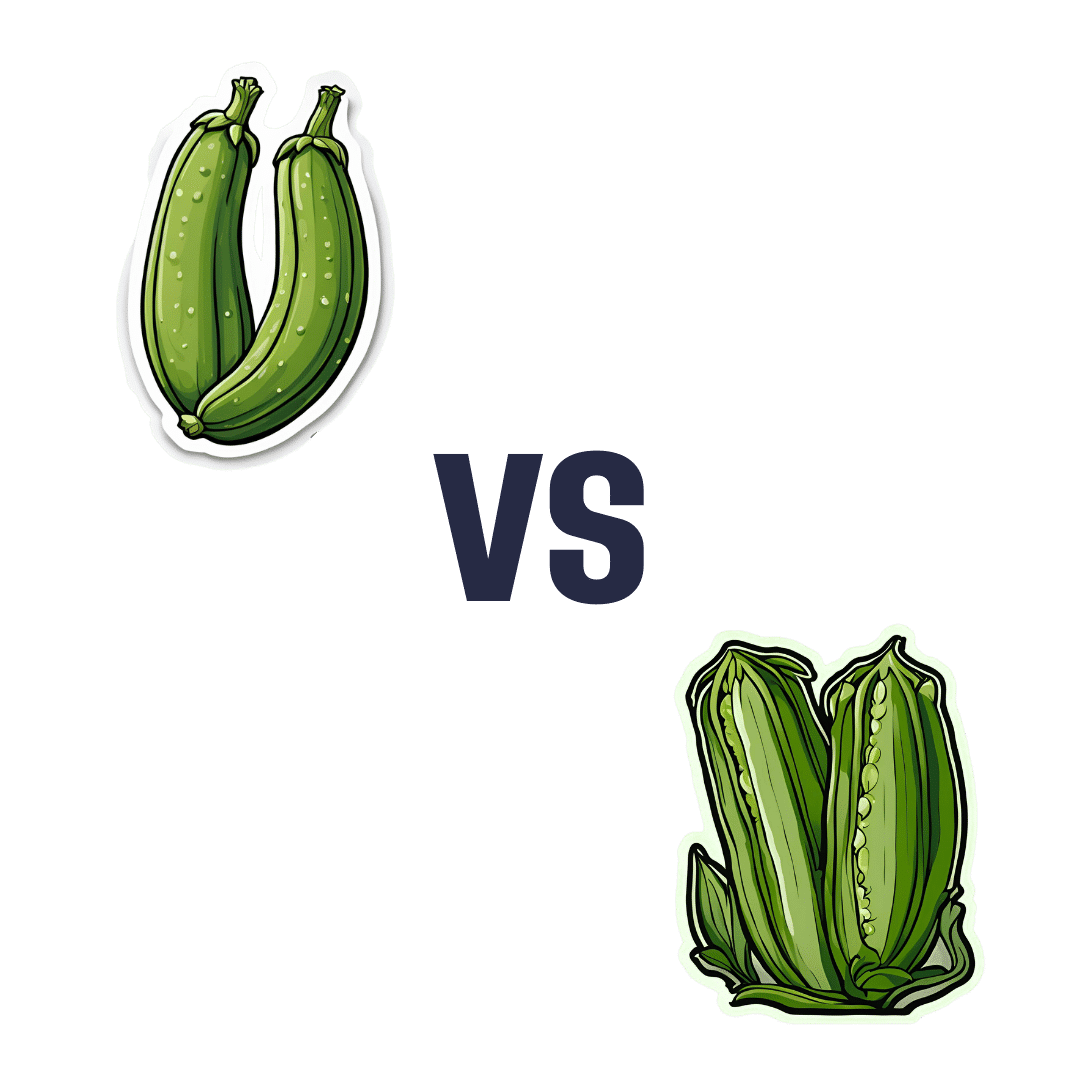
Zucchini vs Okra – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing zucchini to okra, we picked the okra.
Why?
Looking at the macros first, okra has nearly 2x the protein and more than 3x the fiber (for about 2x the carbs).
In terms of vitamins, things are also quite one-sided; zucchini has a little more vitamin B2, while okra has a lot more of vitamins A, B1, B3, B5, B6, B9, C, E, K, and choline.
Nor does the mineral situation make any compelling counterargument; zucchini is higher only in sodium, while okra has a lot more calcium, copper, iron, magnesium, manganese, phosphorus, potassium*, selenium, and zinc.
*Actually it’s only a little more potassium. But the rest are with big margins of difference.
Both of these on-the-cusp-of-being-pungent vegetables have beneficial antioxidant polyphenols (especially various forms of quercetin), but okra has more.
In short: enjoy both, of course, but there’s a clear winner here and it’s okra.
Want to learn more?
You might like to read:
Enjoy Bitter/Astringent/Pungent Foods For Your Heart & Brain
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
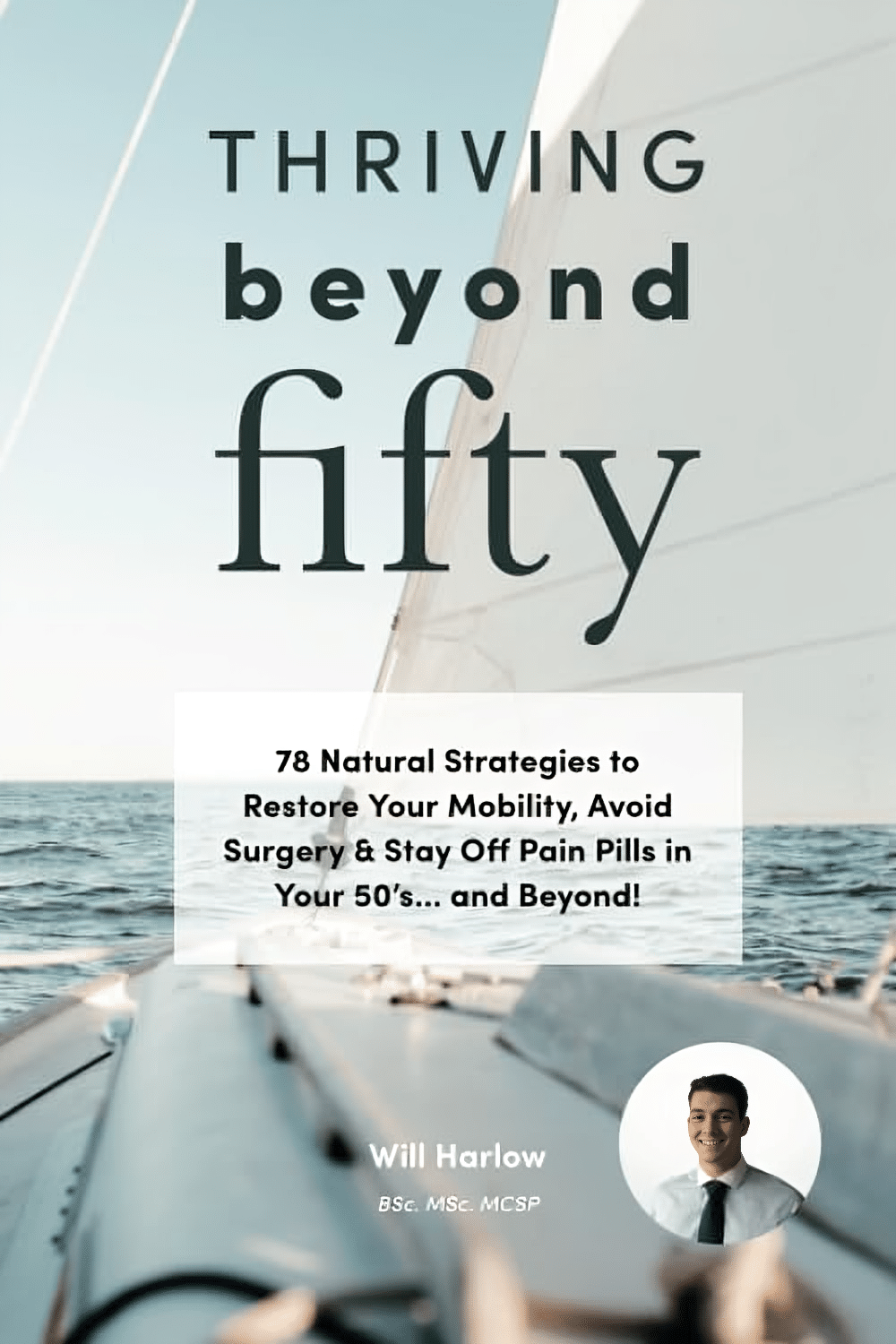
Thriving Beyond Fifty – by Will Harlow
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve featured this author sometimes in our video section; he’s an over-50s specialist physiotherapist with a lot of very functional advice to offer.
In this book, Harlow focusses heavily on three things: mobility, strength, endurance.
You may not want to be a gymnast, powerlifter, or marathon-runner, but these things are important for us all to maintain to at least a fair degree:
- Mobility can be the difference between tweaking one’s shoulder getting something from a high shelf, or not
- Strength can be the difference between being able to get back up, or not
- Endurance can be the difference between coming back from a long day on your feet and thinking “that was a good day; I’m looking forward to tomorrow now”, or not
One of the greatest strengths of this book is its comprehensive troubleshooting aspect; if you have a weak spot, chances are this book has the remedy.
As for the style, it’s quite casual/conversational in tone, but without skimping on science and detail. It’s clear, explanatory, and helpful throughout.
Bottom line: if you’d like to maintain/improve mobility, strength, and endurance, then this book is a very recommendable resource.
Click here to check out Thriving Beyond Fifty, and keep thriving at every age!
Share This Post
-
Health Benefits Of Cranberries (But: You’d Better Watch Out)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Health Benefits Of Cranberries (But: You’d Better Watch Out)
Quick clarification first: today we’re going to be talking about cranberries. Not “cranberry juice drink” that is loaded with sugar, nor “cranberry jelly” or similar that is more added sugar than it is cranberry.
We’re going to keep this short today, because “eat berries” is probably something you know already, but there are some things you should be aware of!
The benefits
Cranberries, even more than most berries, are full of polyphenols and flavonoids that do “those three things that usually come together”: antioxidant properties, anti-inflammatory properties, and anti-cancer properties
Unsurprisingly, this also means they’re good for the immune system and thus quite a boon in flu season:
They’re also good for heart health:
Quick Tip: we’re giving you one study for each of these things for brevity, but if you click through on any of our PubMed study links, you’ll (almost) always see a heading “Similar articles” heading beneath it, which will (almost) always show you plenty more.
Perhaps the most popular reason people take cranberry supplements, though, is their effectiveness at prevention of urinary tract infections:
Indeed, their effectiveness is such that researchers have considered them a putative alternative to antibiotics, particularly in individuals with recurrent UTIs:
Is it safe?
Cranberries are generally considered a very healthful food. However, there are two known possible exceptions:
If you are taking warfarin, it is possible that cranberry consumption may cause additional anti-clotting effects that you don’t want.
If you are at increased risk of kidney stones, the science is currently unclear as to whether this will help or hinder:
- Influence of cranberry juice on the urinary risk factors for calcium oxalate kidney stone formation ← this one concluded “Cranberry juice has antilithogenic properties and, as such, deserves consideration as a conservative therapeutic protocol in managing calcium oxalate urolithiasis”
- Dietary supplementation with cranberry concentrate tablets may increase the risk of nephrolithiasis ← this one, as you can see, concluded the opposite
- Safety of Cranberry: Evaluation of Evidence of Kidney Stone Formation and Botanical Drug-Interactions ← this one acknowledges “contradictory data regarding the role of cranberry in kidney stone formation”
Where can I get some?
You can probably buy fresh, frozen, or dried cranberries from wherever you normally do your grocery shopping.
However, if you prefer to take it in supplement form, then here’s an example product on Amazon
Enjoy!
Share This Post
-
Proteins Of The Week
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week’s news round-up is, entirely by chance, somewhat protein-centric in one form or another. So, check out the bad, the very bad, the mostly good, the inconvenient, and the worst:
Mediterranean diet vs the menopause
Researchers looked at hundreds of women with an average age of 51, and took note of their dietary habits vs their menopause symptoms. Most of them were consuming soft drinks and red meat, and not good in terms of meeting the recommendations for key food groups including vegetables, legumes, fruit, fish and nuts, and there was an association between greater adherence to Mediterranean diet principles, and better health.
Read in full: Fewer soft drinks and less red meat may ease menopause symptoms: Study
Related: Four Ways To Upgrade The Mediterranean Diet
Listeria in meat
This one’s not a study, but it is relevant important news. The headline pretty much says it all, so if you don’t eat meat, this isn’t one you need to worry about any further than that. If you do eat meat, though, you might want to check out the below article to find out whether the meat you eat might be carrying listeria:
Read in full: Almost 10 million pounds of meat recalled due to Listeria danger
Related: Frozen/Thawed/Refrozen Meat: How Much Is Safety, And How Much Is Taste?
Brawn and brain?
A study looked at cognitively healthy older adults (of whom, 57% women), and found an association between their muscle strength and their psychological wellbeing. Note that when we said “cognitively healthy”, this means being free from dementia etc—not necessarily psychologically health in all respects, such as also being free from depression and enjoying good self-esteem.
Read in full: Study links muscle strength and mental health in older adults
Related: Staying Strong: Tips To Prevent Muscle Loss With Age
The protein that blocks bone formation
This one’s more clinical but definitely of interest to any with osteoporosis or at high risk of osteoporosis. Researchers identified a specific protein that blocks osteoblast function, thus more of this protein means less bone production. Currently, this is not something that we as individuals can do anything about at home, but it is promising for future osteoporosis meds development.
Read in full: Protein blocking bone development could hold clues for future osteoporosis treatment
Related: Which Osteoporosis Medication, If Any, Is Right For You?
Rabies risk
People associate rabies with “rabid dogs”, but the biggest rabies threat is actually bats, and they don’t even need to necessarily bite you to confer the disease (it suffices to have licked the skin, for instance—and bats are basically sky-puppies who will lick anything). Because rabies has a 100% fatality rate in unvaccinated humans, this is very serious. This means that if you wake up and there’s a bat in the house, it doesn’t matter if it hasn’t bitten anyone; get thee to a hospital (where you can get the vaccine before the disease takes hold; this will still be very unpleasant but you’ll probably survive so long as you get the vaccine in time).
Read in full: What to know about bats and rabies
Related: Dodging Dengue In The US ← much less serious than rabies, but still not to be trifled with—particularly noteworthy if you’re in an area currently affected by floodwaters or even just unusually heavy rain, by the way, as this will leave standing water in which mosquitos breed.
Take care!
Share This Post
Related Posts
-
Valentine’s Day & Your Heart
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re not talking metaphorically; this is about your “beating wet pumpy thing” as a friend of this writer once put it!
Heart to heart
A dietician calls for us to take care of our hearts this Valentine’s Day, with ideas such as:
- Teamwork makes the dream work: support your partner’s health objectives by choosing gifts or activities that align with their goals, such as opting for new running shoes instead of candy if they aim to exercise more.
- Split up… Dinner: instead of consuming large portions individually, consider sharing a decadent meal to reduce metabolic load while still enjoying the experience together.
- A moving experience: plan active dates like hiking, dancing, or taking a walk, which promote both bonding and cardiovascular health. And if you can think of other perhaps “vigorous activities” you might enjoy doing together on Valentine’s Day, then that’s great for your heart too!
- Be aware of mutual health influences: recognize that partners can impact each other’s health behaviors and risks; making healthy choices together can strengthen both the relationship and individual well-being.
- No date, no problem: if you’re single this Valentine’s Day, consider connecting with friends, of if that’s not for you, perhaps treating yourself to a “self-care day” at home.
Read in full: Celebrate Valentine’s Day with actual hearts in mind, says dietitian
Related: Only One Kind Of Relationship Promotes Longevity This Much!
Playing the hand you’re dealt
We can make many choices in life that affect our health one way or the other, but there are some things we can’t control, and that includes a family history of some disease or other. In the case of a family history of heart conditions, all is not lost, and you can still play the odds:
- Diet: rich in fiber, especially fresh fruits and vegetables, legumes, and whole grains. Go easy on sugary, salty, and/or processed foods. Yes, sugary too! Sugary foods can increase blood pressure in the same way that salt does, by forcing the same homeostatic response.
- Exercise: prioritize movement, as in those “active minutes” that your smartwatch tracks. That famous “150 minutes per week” is great; more is better.
- Sleep: get up regularly around the same time each morning, preferably early. You should get to the point whereby you wake up shortly before the time your alarm would go off, each morning.
- Avoid: smoking and alcohol. They are both terrible for heart health.
- Teamwork: work with healthcare professionals to manage your heart health; a personalized plan is best, and they are there to help.
Remember, genes predispose; they don’t predetermine:
Read in full: Expert explains how to improve heart health, even if your family has history of heart conditions
Related: The Whole Heart Solution: Halt Heart Disease Now With the Best Alternatives and Traditional Medicine
Not so sweet?
Chocolate is famously high in antioxidants, but that must be weighed against other factors, if for example you’re eating a product that, when all’s said and done and the ingredients list is read, is mostly sugar.
That can be avoided, though! If you do like chocolate, we recommend getting dark chocolate with a high percentage of cocoa; 90% is great if you can find it!
Even so, the saturated fat content means you still might want to make it a moment for intentional “mindful eating” of a square or two, before setting it aside for another day:
Read in full: Valentine’s Day and chocolate are a perfect match, but is it a healthy relationship?
Related: 10 “Healthy” Foods That Are Often Worse Than You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Buffed-Up Buffalo Cauliflower
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is a tasty snack that also more protein than you’d think, because of the garbanzo bean flour. It also has plenty of health-giving spices, as well as blood-sugar-balancing vinegar, no added sugar, and very little salt.
You will need
- 1 medium head of cauliflower, cut into florets
- ½ cup garbanzo bean flour
- ½ cup water
- ⅓ cup hot sauce (we recommend a low-sugar kind; Nando’s hot sauce is good for this if available where you are, as it has no added sugar and its main ingredient by volume is vinegar, which is good for balancing blood sugars)
- 2 tbsp extra virgin olive oil, plus more for the pan
- 2 tsp garlic powder
- 2 tsp nutritional yeast
- 2 tsp black pepper, freshly ground
- 1 tsp smoked paprika
- ½ tsp MSG, or 1 tsp low sodium salt
For the ranch sauce:
- ½ cup raw sunflower seeds
- ⅓ cup water
- ⅓ cup milk (plant milk being healthiest if you choose one that’s unsweetened)
- 2 tbsp apple cider vinegar
- 2 tbsp extra virgin olive oil
- 1 tsp onion powder
- 1 tsp dried thyme
- 1 tsp dried oregano
- 1 tsp dried dill
- ½ tsp MSG, or 1 tsp low sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 400℉/200℃.
2) Blend the ranch sauce ingredients until smooth, and set aside.
3) Mix the buffalo cauliflower ingredients except for the cauliflower, in a big bowl.
4) Add the cauliflower to the big bowl, mixing well to coat evenly.
5) Bake the buffalo cauliflower florets on a baking tray lined with baking paper, for about 25 minutes, turning gently if it seems they are at risk of cooking unevenly.
6) Serve hot, with the sunflower ranch on the side!
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- An Apple (Cider Vinegar) A Day…
- 10 Ways To Balance Blood Sugars
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Pulse – by Jenny Chandler
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beans, chickpeas, and lentils are well-established super-healthy foods, but they’re often not a lot of people’s favorite. And why? Usually because of unhappy associations with boring dishes that can barely be called dishes.
This book raises the bar for pulses of various kinds, and not only provides recipes (180 of them) but also guidelines on principles, tips and tricks, what works and what doesn’t, what makes things better or worse, perfect partners, sprouting, and more.
The recipes themselves are not all vegan, nor even all vegetarian, but the beans are the star throughout. For those who are vegan or vegetarian, it’s easy to make substitutions, not least of all because the author is generous with “try this instead of that” and “consider also” suggestions, to help us tailor each dish to our personal preferences, and even the desired vibe of a given meal.
The dishes are neither overly simplistic (it’s not a student survival cookbook, by any means) nor overly complicated; rather, enough is done to make each dish invitingly tasty, and nothing extraneous or pretentious is added for the sake of being fancy. This is about delicious home cooking, nothing more nor less.
If the book has a weakness, it’s that visual learners will feel the absence of pictures for many recipes. But, the text is clear, the instructions are easy to follow, and a photo for each dish would probably have doubled the cost of the book, at least, while halving the number of recipes.
Bottom line: if you’d like to get more beans and other pulses in your diet, but are unsure how to make it exciting, this is an excellent option.
Click here to check out Pulse, and expand your kitchen repertoire!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: