You’re Not Forgetful: How To Remember Everything
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Elizabeth Filips, medical student busy learning a lot of information, explains how in today’s video:
Active processing
An important thing to keep in mind is that forgetting is an active process, not passive as once believed. It has its own neurotransmitters and pathways, and as such, to improve memory, it’s essential to understand and manage forgetting.
So, how does forgetting occur? Memories are stored with cues or tags, which help retrieve information. However, overloading cues with too much information can cause “transient forgetting”—that is to say, the information is still in there somewhere; you just don’t have the filing system required to retrieve the data. This is the kind of thing that you will try hard to remember at some point in the day when you need it, fail, and then wake up at 3am with an “Aha!” because your brain finally found what you were looking for. So, to avoid that, use unique and strong cues to help improve recall (mnemonics are good for this, as are conceptual anchors).
While memory does not appear to actually be finite, there is some practical truth in the “finite storage” model insofar as learning new information can overwrite previous knowledge, iff your brain mistakes it for an update rather than addition. So for that reason, it’s good to periodically go over old information—in psychology this is called rehearsal, which may conjure theatrical images, but it can be as simple as mentally repeating a phone number, a mnemonic, or visually remembering a route one used to take to go somewhere.
Self-perception affects memory performance. Negative beliefs about one’s memory can worsen performance (so don’t say “I have a bad memory”, even to yourself, and in contrast, find more positive affirmations to make about your memory), and mental health in general plays a significant role in memory. For example, if you have ever had an extended period of depression, then chances are good you have some huge gaps in your memory for that time in your life.
A lot of what we learned in school was wrong—especially what we learned about learning. Traditional (vertical) learning is harder to retain, whereas horizontal learning (connecting topics through shared characteristics) creates stronger, interconnected memories. In short, your memories should tell contextual stories, not be isolated points of data.
Embarking on a new course of study? Yes? (If not, then why not? Pick something!)
It may be difficult at first, but experts memorize things more quickly due to built-up intuition in their field. For example a chess master can glance at a chess board for about 5 seconds and memorize the position—but only if the position is one that could reasonably arise in a game; if the pieces are just placed at random, then their memorization ability plummets to that of the average person, because their expertise has been nullified.
What this means in practical terms: building a “skeleton” framework before learning can enhance memorization through logical connections. For this reason, if embarking on a serious course of study, getting a good initial overview when you start is critical, so that you have a context for the rest of what you learn to go into. For example, let’s say you want to learn a language; if you first quickly do a very basic bare-bones course, such as from Duolingo or similar, then even though you’ll have a very small vocabulary and a modest grasp of grammar and make many mistakes and have a lot of holes in your knowledge, you now have somewhere to “fit” every new word or idea you learn. Same goes for other fields of study; for example, a doctor can be told about a new drug and remember everything about it immediately, because they understand the systems it interacts with, understand how it does what it does, and can compare it mentally to similar drugs, and they thus have a “place” in that overall system for the drug information to reside. But for someone who knows nothing about medicine, it’s just a lot of big words with no meaning. So: framework first, details later.
For more on all this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Boost Your Memory Immediately (Without Supplements)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Undoing The Damage Of Life’s Hard Knocks
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sometimes, What Doesn’t Kill Us Makes Us Insecure
We’ve written before about Complex PTSD, which is much more common than the more popularly understood kind:
Given that C-PTSD affects so many people (around 1 in 5, but really, do read the article above! It explains it better than we have room to repeat today), it seems like a good idea to share tips for managing it.
(Last time, we took all the space for explaining it, so we just linked to some external resources at the end)
What happened to you?
PTSD has (as a necessity, as part of its diagnostic criteria) a clear event that caused it, which makes the above question easy to answer.
C-PTSD often takes more examination to figure out what tapestry of circumstances (and likely but not necessarily: treatment by other people) caused it.
Often it will feel like “but it can’t be that; that’s not that bad”, or “everyone has things like that” (in which case, you’re probably one of the one in five).
The deeper questions
Start by asking yourself: what are you most afraid of, and why? What are you most ashamed of? What do you fear that other people might say about you?
Often there is a core pattern of insecurity that can be summed up in a simple, harmful, I-message, e.g:
- I am a bad person
- I am unloveable
- I am a fake
- I am easy to hurt
- I cannot keep my loved ones safe
…and so forth.
For a bigger list of common insecurities to see what resonates, check out:
Basic Fears/Insecurities, And Their Corresponding Needs/Desires
Find where they came from
You probably learned bad beliefs, and consequently bad coping strategies, because of bad circumstances, and/or bad advice.
- When a parent exclaimed in anger about how stupid you are
- When a partner exclaimed in frustration that always mess everything up
- When an employer told you you weren’t good enough
…or maybe they told you one thing, and showed you the opposite. Or maybe it was entirely non-verbal circumstances:
- When you gambled on a good idea and lost everything
- When you tried so hard at some important endeavour and failed
- When you thought someone could be trusted, and learned the hard way that you were wrong
These are “life’s difficult bits”, but when we’ve lived through a whole stack of them, it’s less like a single shattering hammer-blow of PTSD, and more like the consistent non-stop tap tap tap that ends up doing just as much damage in the long run.
Resolve them
That may sound a bit like a “and quickly create world peace” level of task, but we have tools:
Ask yourself: what if…
…it had been different? Take some time and indulge in a full-blown fantasy of a life that was better. Explore it. How would those different life lessons, different messages, have impacted who you are, your personality, your behaviour?
This is useful, because the brain is famously bad at telling real memories from false ones. Consciously, you’ll know that one was an exploratory fantasy, but to your brain, it’s still doing the appropriate rewiring. So, little by little, neuroplasticity will do its thing.
Tell yourself a better lie
We borrowed this one from the title of a very good book which we’ve reviewed previously.
This idea is not about self-delusion, but rather that we already express our own experiences as a sort of narrative, and that narrative tends to contain value judgements that are often not useful, e.g. “I am stupid”, “I am useless”, and all the other insecurities we mentioned earlier. Some simple examples might be:
- “I had a terrible childhood” → “I have come so far”
- “I should have known better” → “I am wiser now”
- “I have lost so much” → “I have experienced so much”
So, replacing that self-talk can go a long way to re-writing how secure we feel, and therefore how much trauma-response (ideally: none!) we have to stimuli that are not really as threatening as we sometimes feel they are (a hallmark of PTSD in general).
Here’s a guide to more ways:
How To Get Your Brain On A More Positive Track (Without Toxic Positivity)
Take care!
Share This Post
-
What’s the difference between shyness and social anxiety?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s the difference? is a new editorial product that explains the similarities and differences between commonly confused health and medical terms, and why they matter.
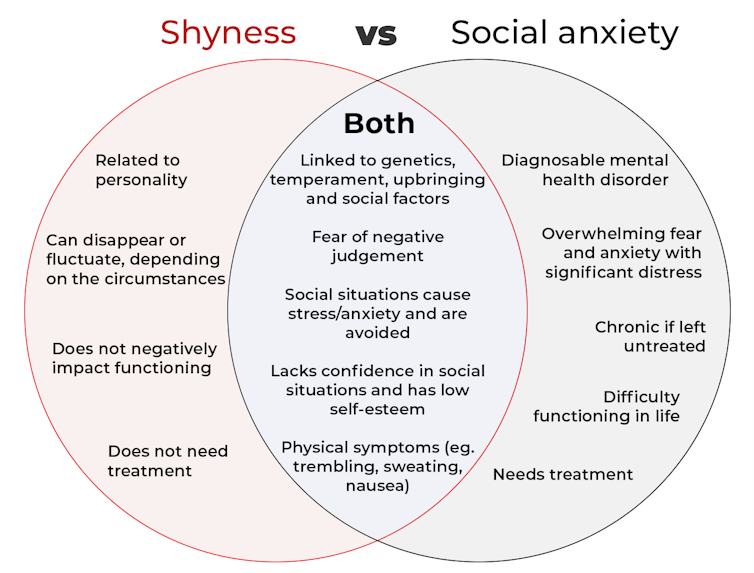
The terms “shyness” and “social anxiety” are often used interchangeably because they both involve feeling uncomfortable in social situations.
However, feeling shy, or having a shy personality, is not the same as experiencing social anxiety (short for “social anxiety disorder”).
Here are some of the similarities and differences, and what the distinction means.
pathdoc/Shutterstock How are they similar?
It can be normal to feel nervous or even stressed in new social situations or when interacting with new people. And everyone differs in how comfortable they feel when interacting with others.
For people who are shy or socially anxious, social situations can be very uncomfortable, stressful or even threatening. There can be a strong desire to avoid these situations.
People who are shy or socially anxious may respond with “flight” (by withdrawing from the situation or avoiding it entirely), “freeze” (by detaching themselves or feeling disconnected from their body), or “fawn” (by trying to appease or placate others).
A complex interaction of biological and environmental factors is also thought to influence the development of shyness and social anxiety.
For example, both shy children and adults with social anxiety have neural circuits that respond strongly to stressful social situations, such as being excluded or left out.
People who are shy or socially anxious commonly report physical symptoms of stress in certain situations, or even when anticipating them. These include sweating, blushing, trembling, an increased heart rate or hyperventilation.
How are they different?
Social anxiety is a diagnosable mental health condition and is an example of an anxiety disorder.
For people who struggle with social anxiety, social situations – including social interactions, being observed and performing in front of others – trigger intense fear or anxiety about being judged, criticised or rejected.
To be diagnosed with social anxiety disorder, social anxiety needs to be persistent (lasting more than six months) and have a significant negative impact on important areas of life such as work, school, relationships, and identity or sense of self.
Many adults with social anxiety report feeling shy, timid and lacking in confidence when they were a child. However, not all shy children go on to develop social anxiety. Also, feeling shy does not necessarily mean a person meets the criteria for social anxiety disorder.
People vary in how shy or outgoing they are, depending on where they are, who they are with and how comfortable they feel in the situation. This is particularly true for children, who sometimes appear reserved and shy with strangers and peers, and outgoing with known and trusted adults.
Individual differences in temperament, personality traits, early childhood experiences, family upbringing and environment, and parenting style, can also influence the extent to which people feel shy across social situations.
Not all shy children go on to develop social anxiety. 249 Anurak/Shutterstock However, people with social anxiety have overwhelming fears about embarrassing themselves or being negatively judged by others; they experience these fears consistently and across multiple social situations.
The intensity of this fear or anxiety often leads people to avoid situations. If avoiding a situation is not possible, they may engage in safety behaviours, such as looking at their phone, wearing sunglasses or rehearsing conversation topics.
The effect social anxiety can have on a person’s life can be far-reaching. It may include low self-esteem, breakdown of friendships or romantic relationships, difficulties pursuing and progressing in a career, and dropping out of study.
The impact this has on a person’s ability to lead a meaningful and fulfilling life, and the distress this causes, differentiates social anxiety from shyness.
Children can show similar signs or symptoms of social anxiety to adults. But they may also feel upset and teary, irritable, have temper tantrums, cling to their parents, or refuse to speak in certain situations.
If left untreated, social anxiety can set children and young people up for a future of missed opportunities, so early intervention is key. With professional and parental support, patience and guidance, children can be taught strategies to overcome social anxiety.
Why does the distinction matter?
Social anxiety disorder is a mental health condition that persists for people who do not receive adequate support or treatment.
Without treatment, it can lead to difficulties in education and at work, and in developing meaningful relationships.
Receiving a diagnosis of social anxiety disorder can be validating for some people as it recognises the level of distress and that its impact is more intense than shyness.
A diagnosis can also be an important first step in accessing appropriate, evidence-based treatment.
Different people have different support needs. However, clinical practice guidelines recommend cognitive-behavioural therapy (a kind of psychological therapy that teaches people practical coping skills). This is often used with exposure therapy (a kind of psychological therapy that helps people face their fears by breaking them down into a series of step-by-step activities). This combination is effective in-person, online and in brief treatments.
Treatment is available online as well as in-person. ImYanis/Shutterstock For more support or further reading
Online resources about social anxiety include:
- This Way Up’s online program for managing excessive shyness and fear of social situations
- Beyond Blue’s resources on social anxiety
- a guide to looking after yourself if you have social anxiety, from the Western Australian health department
- social anxiety online program for children and teens from the University of Queensland
- inroads, a self-guided online program for young adults who drink alcohol to manage their anxiety.
We thank the Black Dog Institute Lived Experience Advisory Network members for providing feedback and input for this article and our research.
Kayla Steele, Postdoctoral research fellow and clinical psychologist, UNSW Sydney and Jill Newby, Professor, NHMRC Emerging Leader & Clinical Psychologist, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Leverage Placebo Effect For Yourself
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago
The placebo effect is a well-known, well-evidenced factor that is very relevant when it comes to the testing and implementation of medical treatments:
NIH | National Center for Biotechnology Information | Placebo Effect
Some things that make placebo effect stronger include:
- Larger pills instead of small ones: because there’s got to be more going on in there, right?
- Thematically-colored pills: e.g. red for stimulant effects, blue for relaxing effects
- Things that seem expensive: e.g. a well-made large heavy machine, over a cheap-looking flimsy plastic device. Similarly, medication from a small glass jar with a childproof lock, rather than popped out from a cheap blister-pack.
- Things that seem rational: if there’s an explanation for how it works that you understand and find rational, or at least you believe you understand and find rational ← this works in advertising, too; if there’s a “because”, it lands better almost regardless of what follows the word “because”
- Things delivered confidently by a professional: this is similar to the “argument from authority” fallacy (whereby a proposed authority will be more likely trusted, even if this is not their area of expertise at all, e.g. celebrity endorsements), but in the case of placebo trials, this often looks like a well-dressed middle-aged or older man with an expensive haircut calling for a young confident-looking aide in a lab coat to administer the medicine, and is received better than a slightly frazzled academic saying “and, uh, this one’s yours” while handing you a pill.
- Things with ritual attached: this can be related to the above (the more pomp and circumstance is given to the administration of the treatment, the better), but it can also be as simple as an instruction on an at-home-trial medication saying “take 20 minutes before bed”. Because, if it weren’t important, they wouldn’t bother to specify that, right? So it must be important!
And now for a quick personality test
Did you see the above as a list of dastardly tricks to watch out for, or did you see the above as a list of things that can make your actual medication more effective?
It’s arguably both, of course, but the latter more optimistic view is a lot more useful than the former more pessimistic one.
Since placebo effect works at least somewhat even when you know about it, there is nothing to stop you from leveraging it for your own benefit when taking medication or doing health-related things.
Next time you take your meds or supplements or similar, pause for a moment for each one to remember what it is and what it will be doing for you. This is a lot like the principles (which are physiological as well as psychological) of mindful eating, by the way:
How To Get More Nutrition From The Same Food
Placebo makes some surprising things evidence-based
We’ve addressed placebo effect sometimes as part of an assessment of a given alternative therapy, often in our “Mythbusting Friday” edition of 10almonds.
- In some cases, placebo is adjuvant to the therapy, i.e. it is one of multiple mechanisms of action (example: chiropractic or acupuncture)
- In some cases, placebo is the only known mechanism of action (example: homeopathy)
- In some cases, even placebo can’t help (example: ear candling)
One other fascinating and far-reaching (in a potentially good way) thing that placebo makes evidence-based is: prayer
…which is particularly interesting for something that is fundamentally faith-based, i.e. the opposite of evidence-based.
Now, we’re a health science publication, not a theological publication, so we’ll consider actual divine intervention to be beyond the scope of mechanisms of action we can examine, but there’s been a lot of research done into the extent to which prayer is beneficial as a therapy, what things it may be beneficial for, and what factors affect whether it helps:
Prayer and healing: A medical and scientific perspective on randomized controlled trials
👆 full paper here, and it is very worthwhile reading if you have time, whether or not you are religious personally
Placebo works best when there’s a clear possibility for psychosomatic effect
We’ve mentioned before, and we’ll mention again:
- psychosomatic effect does not mean: “imagining it”
- psychosomatic effect means: “your brain regulates almost everything else in your body, directly or indirectly, including your autonomic functions, and especially notably when it comes to illness, your immune responses”
So, a placebo might well heal your rash or even shrink a tumor, but it probably won’t regrow a missing limb, for instance.
And, this is important: it’s not about how credible/miraculous the outcome will be!
Rather, it is because we have existing pre-programmed internal bodily processes for healing rashes and shrinking tumors, that just need to be activated—whereas we don’t have existing pre-programmed internal bodily processes for regrowing a missing limb, so that’s not something our brain can just tell our body to do.
So for this reason, in terms of what placebo can and can’t do:
- Get rid of cancer? Yes, sometimes—because the body has a process for doing that; enjoy your remission
- Fix a broken nail? No—because the body has no process for doing that; you’ll just have to cut it and wait for it to grow again
With that in mind, what will you use the not-so-mystical powers of placebo for? What ever you go for… Enjoy, and take care!
Share This Post
Related Posts
-
Exercise and Fat Loss (5 Things You Need To Know)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to think “I’ll eat whatever; I can always burn it off later”, and if it’s an odd occasion, then that’s fine; indeed, a fit and healthy body can usually weather small infrequent dietary indiscretions easily. But…
You can’t outrun a bad diet
Exercise can create a calorie deficit, but over time, the body balances this out by adjusting one’s metabolism, leading to a plateau in fat loss—and as you might know, you can’t out-exercise a bad diet. On the contrary, dietary adjustments are crucial for fat loss and body recomposition.
About that calorie deficit in the first place, by the way: extreme calorie deficits through exercise alone can lead to muscle loss, reduced energy, and thus sabotage long-term fat loss because having muscle mass increases one’s base metabolic rate (while having fat does not).
Another thing to bear in mind about exercise is that longer workouts without adequate rests in between can cause burnout, injury, or weight gain due to the body doing its best to conserve energy.
So, a good diet is a necessary condition for both muscle maintenance and fat loss.
Five Key Diet Tips:
- Include foods you love: don’t feel obliged cut out favorite foods that are a little unhealthy; incorporate them in moderation for sustainability.
- Keep adjustments small: avoid making drastic dietary changes all at once; make gradual tweaks to prevent feeling deprived.
- Prioritize protein: focus on including a protein source in every meal to increase satiety and aid in muscle building.
- Avoid low-calorie diets: drastically cutting calories can lead to muscle loss, metabolic adaptation, and overeating.
- Embrace diet evolution: changes may not feel sustainable at first, but adjustments over time help achieve long-term balance. You can always “adjust course” as you go.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Are You A Calorie-Burning Machine?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Edamame vs Soybeans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing edamame to soybeans, we picked the soybeans.
Why?
You may be thinking: aren’t edamame soybeans? And yes, yes they are. But just like our many instances of pitting Brassica oleracea vs Brassica oleracea (one species, many cultivars e.g. broccoli, cauliflower, kale, cabbage, Brussels sprouts, etc), there are still differences. In this case, edamame and soybeans aren’t even different cultivars, what are conventionally called edamame are just the young beans of the plant, while what are conventionally called soybeans are the mature beans of the plant.
The main nutritional difference is: as they get older, they lose vitamins and gain minerals. More on that later. But first, “main difference” isn’t “only difference”, so…
In terms of macros, edamame have more carbs, while soybeans have a little more fiber and a lot more protein. An easy win for the mature soybeans.
In the category of vitamins, edamame have more of vitamins A, B1, B3, B5, B9, C, E, K, and choline, while soybeans have more of vitamins B2 and B6. A clear win for edamame, this time.
When it comes to minerals, the nutritional tables are turned, and edamame have more manganese and zinc, while soybeans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium. An easy win for soybeans.
Adding up the sections makes for a two-to-one victory for soybeans, but by all means enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
White Bread vs White Pasta – Which Is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing a white bread to a white pasta, we picked the pasta.
Why?
Neither are great for the health! But like for like, the glycemic index of the bread is usually around 150% of the glycemic index for pasta.
All that said, we heartily recommend going for wholegrain in either case!
Bonus tip: cooking pasta “al dente”, so it is still at least a little firm to the bite, results in a lower GI compared to being boiled to death.
Bonus bonus tip: letting pasta cool increases resistant starches. You can then reheat the pasta without losing this benefit.
Please don’t put it in the microwave though; you will make an Italian cry. Instead, simply put it in a colander and pour boiling water over it, and then serve in your usual manner (a good approach if serving it separately is: put it in the serving bowl/dish/pan, drizzle a little extra virgin olive oil and a little cracked black pepper, stir to mix those in, and serve)
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: