Yoga that Helps You on the Loo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How This Video Helps You Poo
When you’re feeling a bit bloated, Yoga With Bird’s 10-minute yoga routine promises to help you release…your gas. And, perhaps, more.
From a tabletop flow to soothing twists, each pose allows you to sync your breath with movement, helping to promote organic relief.
With options to modify with pillows for extra support, this video (below) caters to everyone needing a digestive reset.
Other Toilet Tricks
If yoga isn’t your thing, or you’re interested in trying to use different methods to make your visits to the bathroom a bit easier, we’ve spoken about the ways to manage gut health, and use of probiotics or fiber, and even the prevention of hemorrhoids.
Namaste and goodbye to bloat!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Beat Loneliness & Isolation
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Overcoming Loneliness & Isolation
One of the biggest mental health threats that faces many of us as we get older is growing isolation, and the loneliness that can come with it. Family and friends thin out over the years, and getting out and about isn’t always as easy as it used to be for everyone.
Nor is youth a guaranteed protection against this—in today’s world of urban sprawl and nothing-is-walkable cities, in which access to social spaces such as cafés and the like means paying the rising costs with money that young people often don’t have… And that’s without getting started on how much the pandemic impacted an entire generation’s social environments (or lack thereof).
Why is this a problem?
Humans are, by evolution, social creatures. As individuals we may have something of a spectrum from introvert to extrovert, but as a species, we thrive in community. And we suffer, when we don’t have that.
What can we do about it?
We can start by recognizing our needs, such as they are, and identifying to what extent they are being met (or not).
- Some of us may be very comfortable with a lot of alone time—but need someone to talk to sometimes.
- Some of us may need near-constant company to feel at our best—and that’s fine too! We just need to plan accordingly.
In the former case, it’s important to remember that needing someone to talk to is not being a burden to them. Not only will our company probably enrich them too, but also, we are evolved to care for one another, and that itself can bring fulfilment to them as much as to you. But what if you don’t a friend to talk to?
- You might be surprised at who would be glad of you reaching out. Have a think through whom you know, and give it a go. This can be scary, because what if they reject us, or worse, they don’t reject us but silently resent us instead? Again, they probably won’t. Human connection requires taking risks and being vulnerable sometimes.
- If that’s not an option, there are services that can fill your need. For some, therapy might serve a dual purpose in this regard. For others, you might want to check out the list of (mostly free) resources at the bottom of this article
In the second case (that we need near-constant company to feel at our best) we probably need to look more at our overall lifestyle, and find ways to be part of a community. That can include:
- Living in a close-knit community (places with a lot of retirees in one place often have this; or younger folk might look at communal living/working spaces, for example)
- Getting involved in local groups (you can check out NextDoor.com or MeetUp.com for this)
- Volunteering for a charity (not only are acts of service generally fulfilling in and of themselves, but also, you will probably be working with other people of a charitable nature, and such people tend to make for good company!)
Need a little help?
There are many, many organizations that will love to help you (or anyone else) overcome loneliness and isolation.
Rather than list them all here and make this email very long by describing how each of them works, here’s a great compilation of resources:
Share This Post
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Ease Neck Pain At Home
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Bang is offering exercises to alleviate neck pain, which pain can be a real… Well, if only there were a good phrase for expressing how troublesome pain in that part of the body can be.
To be clear, he’s a doctor of chiropractic, not a medical doctor, but his advice has clearly been helping people alleviate pain, so without further ado, he advises the following things:
- Taking the head and neck slowly and carefully through the full range of motion available
- Contracting the neck muscles while repeating the above exercise, three times each way
- Backing off a little if it hurts at any point, but noting where the limits lie
- Repeating again the range of motion exercise, this time adding gentle resistance
- Holding each end of this for twenty seconds before releasing and doing the other side, three times each way
- Finally, stabilizing the head centrally and pushing into one’s hands, as an isometric strengthening exercise
He demonstrates each part clearly in this short (5:58) video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more about chiropractic?
You might like our previous main feature:
Is Chiropractic All It’s Cracked Up To Be?
Take care!
Share This Post
Related Posts
-
Take These To Lower Cholesterol! (Statin Alternatives)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Ada Ozoh, a diabetes specialist, took an interest in this upon noting the many-headed beast that is metabolic syndrome means that neither diabetes nor cardiovascular disease exist in a vacuum, and there are some things that can help a lot against both. Here she shares some of her top recommendations:
Statin-free options
Dr. Ozoh recommends:
- Bergamot: lowers LDL (“bad” cholesterol) by about 30% and slightly increases HDL (“good” cholesterol), at 500–1000mg/day, seeing results in 1–6 months
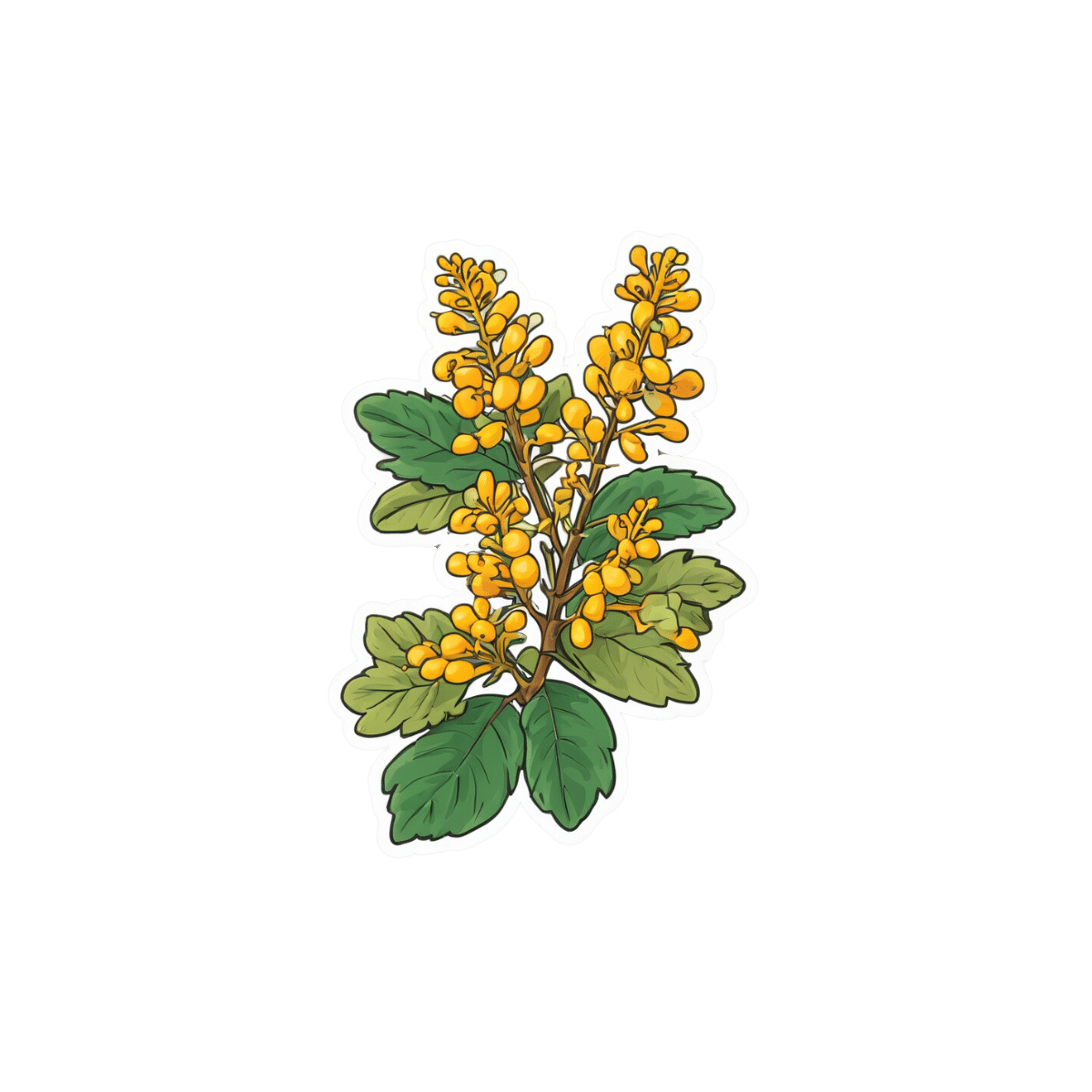
- Berberine: prevents fat absorption and helps burn stored fat, as well as reducing blood sugar levels and blood pressure, at 1,500mg/day
- Silymarin: protects the liver, and lowers cholesterol in type 2 diabetes, at 280–420mg/day
- Phytosterols: lower cholesterol by about 10%; found naturally in many plants, but it takes supplementation to read the needed (for this purpose) dosage of 2g/day
- Red yeast rice: this is white rice fermented with yeast, and it lowers LDL cholesterol by about 25%, seeing results in around 3 months
For more information on all of the above (including more details on the biochemistry, as well as potential issues to be aware of), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- Statins: His & Hers? Very Different For Men & Women
- Berberine For Metabolic Health
- Milk Thistle For The Brain, Bones, & More ← this is about silymarin, which is extracted from Silybum marianum, the milk thistle plant
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Increase in online ADHD diagnoses for kids poses ethical questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In 2020, in the midst of a pandemic, clinical protocols were altered for Ontario health clinics, allowing them to perform more types of care virtually. This included ADHD assessments and ADHD prescriptions for children – services that previously had been restricted to in-person appointments. But while other restrictions on virtual care are back, clinics are still allowed to virtually assess children for ADHD.
This shift has allowed for more and quicker diagnoses – though not covered by provincial insurance (OHIP) – via a host of newly emerging private, for-profit clinics. However, it also has raised significant ethical questions.
It solves an equity issue in terms of rural access to timely assessments, but does it also create new equity issues as a privatized service?
Is it even feasible to diagnose a child for a condition like ADHD without meeting that child in person?
And as rates of ADHD diagnosis continue to rise, should health regulators re-examine the virtual care approach?
Ontario: More prescriptions, less regulation
There are numerous for-profit clinics offering virtual diagnoses and prescriptions for childhood ADHD in Ontario. These include KixCare, which does not offer the option of an in-person assessment. Another clinic, Springboard, makes virtual appointments available within days, charging around $2,600 for assessments, which take three to four hours. The clinic offers coaching and therapy at an additional cost, also not covered by OHIP. Families can choose to continue to visit the clinic virtually during a trial stage with medications, prescribed by a doctor in the clinic who then sends prescribing information back to the child’s primary care provider.
For-profit clinics like these are departing from Canada’s traditional single-payer health care model. By charging patients out-of-pocket fees for services, the clinics are able to generate more revenue because they are working outside of the billing standards for OHIP, standards that set limits on the maximum amount doctors can earn for providing specific services. Instead many services are provided by non-physician providers, who are not limited by OHIP in the same way.
Need for safeguards
ADHD prescriptions rose during the pandemic in Ontario, with women, people of higher income and those aged 20 to 24 receiving the most new diagnoses, according to research published in January 2024 by a team including researchers from the Centre for Addictions and Mental Health and Holland Bloorview Children’s Hospital. There may be numerous reasons for this increase but could the move to virtual care have been a factor?
Ontario psychiatrist Javeed Sukhera, who treats both children and adults in Canada and the U.S., says virtual assessments can work for youth with ADHD, who may receive treatment quicker if they live in remote areas. However, he is concerned that as health care becomes more privatized, it will lead to exploitation and over-diagnosis of certain conditions.
“There have been a lot of profiteers who have tried to capitalize on people’s needs and I think this is very dangerous,” he said. “In some settings, profiteering companies have set up systems to offer ADHD assessments that are almost always substandard. This is different from not-for-profit setups that adhere to quality standards and regulatory mechanisms.”
Sukhera’s concerns recall the case of Cerebral Inc., a New York state-based virtual care company founded in 2020 that marketed on social media platforms including Instagram and TikTok. Cerebral offered online prescriptions for ADHD drugs among other services and boasted more than 200,000 patients. But as Dani Blum reported in the New York Times, Cerebral was accused in 2023 of pressuring doctors on staff to prescribe stimulants and faced an investigation by state prosecutors into whether it violated the U.S. Controlled Substances Act.
“At the start of the pandemic, regulators relaxed rules around medical prescription of controlled substances,” wrote Blum. “Those changes opened the door for companies to prescribe and market drugs without the protocols that can accompany an in-person visit.”
Access increased – but is it equitable?
Virtual care has been a necessity in rural areas in Ontario since well before the pandemic, although ADHD assessments for children were restricted to in-person appointments prior to 2020.
But ADHD assessment clinics that charge families out-of-pocket for services are only accessible to people with higher incomes. Rural families, many of whom are low income, are unable to afford thousands for private assessments, let alone the other services upsold by providers. If the private clinic/virtual care trend continues to grow unchecked, it may also attract doctors away from the public model of care since they can bill more for services. This could further aggravate the gap in care that lower income people already experience.
This could further aggravate the gap in care that lower income people already experience.
Sukhera says some risks could be addressed by instituting OHIP coverage for services at private clinics (similar to private surgical facilities that offer mixed private/public coverage), but also with safeguards to ensure that profits are reinvested back into the health-care system.
“This would be especially useful for folks who do not have the income, the means to pay out of pocket,” he said.
Concerns of misdiagnosis and over-prescription
Some for-profit companies also benefit financially from diagnosing and issuing prescriptions, as has been suggested in the Cerebral case. If it is cheaper for a clinic to do shorter, virtual appointments and they are also motivated to diagnose and prescribe more, then controls need to be put in place to prevent misdiagnosis.
The problem of misdiagnosis may also be related to the nature of ADHD assessments themselves. University of Strathclyde professor Matthew Smith, author of Hyperactive: The Controversial History of ADHD, notes that since the publication of Diagnostic and Statistical Manual of Mental Disorders in 1980, assessment has typically involved a few hours of parents and patients providing their subjective perspectives on how they experience time, tasks and the world around them.
“It’s often a box-ticking exercise, rather than really learning about the context in which these behaviours exist,” Smith said. “The tendency has been to use a list of yes/no questions which – if enough are answered in the affirmative – lead to a diagnosis. When this is done online or via Zoom, there is even less opportunity to understand the context surrounding behaviour.”
Smith cited a 2023 BBC investigation in which reporter Rory Carson booked an in-person ADHD assessment at a clinic and was found not to have the condition, then had a private online assessment – from a provider on her couch in a tracksuit – and was diagnosed with ADHD after just 45 minutes, for a fee of £685.
What do patients want?
If Canadian regulators can effectively tackle the issue of privatization and the risk of misdiagnosis, there is still another hurdle: not every youth is willing to take part in virtual care.
Jennifer Reesman, a therapist and Training Director for Neuropsychology at the Chesapeake Center for ADHD, Learning & Behavioural Health in Maryland, echoed Sukhera’s concerns about substandard care, cautioning that virtual care is not suitable for some of her young clients who had poor experiences with online education and resist online health care. It can be an emotional issue for pediatric patients who are managing their feelings about the pandemic experience.
“We need to respect what their needs are, not just the needs of the provider,” says Reesman.
In 2020, Ontario opted for virtual care based on the capacity of our health system in a pandemic. Today, with a shortage of doctors, we are still in a crisis of capacity. The success of virtual care may rest on how engaged regulators are with equity issues, such as waitlists and access to care for rural dwellers, and how they resolve ethical problems around standards of care.
Children and youth are a distinct category, which is why we had restrictions on virtual ADHD diagnosis prior to the pandemic. A question remains, then: If we could snap our fingers and have the capacity to provide in-person ADHD care for all children, would we? If the answer to that question is yes, then how can we begin to build our capacity?
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sleep Tracking, For Five Million Nights
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
5 Sleep Phenotypes, By Actual Science
You probably know people can be broadly divided into “early birds” and “night owls”:
Early Bird Or Night Owl? Genes vs Environment
…and then the term “hummingbird” gets used for a person who flits between the two.
That’s three animals so far. If you read a book we reviewed recently, specifically this one:
The Power of When – by Dr. Michael Breus
…then you may have used the guide within to self-diagnose your circadian rhythm type (chronotype) according to Dr. Breus’s system, which divides people into bears, lions, wolves, and dolphins.
That’s another four animals. If you have a FitBit, it can “diagnose” you with being those and/or a menagerie of others, such as giraffe, hedgehog, parrot, and tortoise:
How Fitbit Developed the Sleep Profile Experience (Part 2 – Sleep Animals)
Five million nights
A team of researchers recently took a step away from this veritable zoo of 11 different animals and counting, and used a sophisticated modelling system to create a spatial-temporal map of people’s sleep habits, and this map created five main “islands” that people’s sleep habits could settle on, or sometimes move from island to island.
Those “five million nights” by the way? It was actually 5,095,798 nights! You might notice that would take from the 2020s to the 15970s to complete, so this was rather a matter of monitoring 33,152 individuals between January and October of the same year. Between them, they got those 5,095,798 nights of sleep (or in some cases, nights of little or no sleep, but still, they were there for the nights).
The five main phenotypes that the researchers found were:
- What we think of as “normal” sleep. In this phenotype, people get about eight hours of uninterrupted sleep for at least six days in a row.
- As above for half the nights, but they only sleep for short periods of time in bouts of less than three hours the other half.
- As per normal sleep, but with one interrupted night per week, consisting of a 5 hour sleep period and then broken sleep for a few more hours.
- As per normal sleep generally, but with occasional nights in which long bouts of sleep are separated by a mid-sleep waking.
- Sleeping for very short periods of time every night. This phenotype was the rarest the researchers found, and represents extremely disrupted sleep.
As you might suspect, phenotype 1 is healthier than phenotype 5. But that’s not hugely informational, as the correlation between getting good sleep and having good health is well-established. So, what did the study teach us?
❝We found that little changes in sleep quality helped us identify health risks. Those little changes wouldn’t show up on an average night, or on a questionnaire, so it really shows how wearables help us detect risks that would otherwise be missed.❞
More specifically,
❝We found that the little differences in how sleep disruptions occur can tell us a lot. Even if these instances are rare, their frequency is also telling. So it’s not just whether you sleep well or not – it’s the patterns of sleep over time where the key info hides❞
…and, which gets to the absolute point,
❝If you imagine there’s a landscape of sleep types, then it’s less about where you tend to live on that landscape, and more about how often you leave that area❞
In other words: if your sleep pattern is not ideal, that’s one thing and it’d probably be good to address it, by improving your sleep. However, if your sleep pattern changes phenotype without an obvious known reason why, this may be considered an alarm bell warning of something else that needs addressing, which may be an underlying illness or condition—meaning it can be worthwhile being a little extra vigilant when it comes to regular health screenings, in case something new has appeared.
Want to read more?
You can read the paper in full here:
Five million nights: temporal dynamics in human sleep phenotypes
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: