What’s the difference between ADD and ADHD?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Around one in 20 people has attention-deficit hyperactivity disorder (ADHD). It’s one of the most common neurodevelopmental disorders in childhood and often continues into adulthood.
ADHD is diagnosed when people experience problems with inattention and/or hyperactivity and impulsivity that negatively impacts them at school or work, in social settings and at home.
Some people call the condition attention-deficit disorder, or ADD. So what’s the difference?
In short, what was previously called ADD is now known as ADHD. So how did we get here?
Let’s start with some history
The first clinical description of children with inattention, hyperactivity and impulsivity was in 1902. British paediatrician Professor George Still presented a series of lectures about his observations of 43 children who were defiant, aggressive, undisciplined and extremely emotional or passionate.
Since then, our understanding of the condition evolved and made its way into the Diagnostic and Statistical Manual of Mental Disorders, known as the DSM. Clinicians use the DSM to diagnose mental health and neurodevelopmental conditions.
The first DSM, published in 1952, did not include a specific related child or adolescent category. But the second edition, published in 1968, included a section on behaviour disorders in young people. It referred to ADHD-type characteristics as “hyperkinetic reaction of childhood or adolescence”. This described the excessive, involuntary movement of children with the disorder.

In the early 1980s, the third DSM added a condition it called “attention deficit disorder”, listing two types: attention deficit disorder with hyperactivity (ADDH) and attention deficit disorder as the subtype without the hyperactivity.
However, seven years later, a revised DSM (DSM-III-R) replaced ADD (and its two sub-types) with ADHD and three sub-types we have today:
- predominantly inattentive
- predominantly hyperactive-impulsive
- combined.
Why change ADD to ADHD?
ADHD replaced ADD in the DSM-III-R in 1987 for a number of reasons.
First was the controversy and debate over the presence or absence of hyperactivity: the “H” in ADHD. When ADD was initially named, little research had been done to determine the similarities and differences between the two sub-types.
The next issue was around the term “attention-deficit” and whether these deficits were similar or different across both sub-types. Questions also arose about the extent of these differences: if these sub-types were so different, were they actually different conditions?
Meanwhile, a new focus on inattention (an “attention deficit”) recognised that children with inattentive behaviours may not necessarily be disruptive and challenging but are more likely to be forgetful and daydreamers.

Why do some people use the term ADD?
There was a surge of diagnoses in the 1980s. So it’s understandable that some people still hold onto the term ADD.
Some may identify as having ADD because out of habit, because this is what they were originally diagnosed with or because they don’t have hyperactivity/impulsivity traits.
Others who don’t have ADHD may use the term they came across in the 80s or 90s, not knowing the terminology has changed.
How is ADHD currently diagnosed?
The three sub-types of ADHD, outlined in the DSM-5 are:
- predominantly inattentive. People with the inattentive sub-type have difficulty sustaining concentration, are easily distracted and forgetful, lose things frequently, and are unable to follow detailed instructions
- predominantly hyperactive-impulsive. Those with this sub-type find it hard to be still, need to move constantly in structured situations, frequently interrupt others, talk non-stop and struggle with self control
- combined. Those with the combined sub-type experience the characteristics of those who are inattentive and hyperactive-impulsive.
ADHD diagnoses continue to rise among children and adults. And while ADHD was commonly diagnosed in boys, more recently we have seen growing numbers of girls and women seeking diagnoses.
However, some international experts contest the expanded definition of ADHD, driven by clinical practice in the United States. They argue the challenges of unwanted behaviours and educational outcomes for young people with the condition are uniquely shaped by each country’s cultural, political and local factors.
Regardless of the name change to reflect what we know about the condition, ADHD continues to impact educational, social and life situations of many children, adolescents and adults.
Kathy Gibbs, Program Director for the Bachelor of Education, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Triple Your Breast Cancer Survival Chances
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Keeping Abreast Of Your Cancer Risk
It’s the kind of thing that most people think won’t happen to them. And hopefully, it won’t!
But…
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
- *and even this depends on the type of double mastectomy and other circumstances, and technically there will always be a non-zero risk, because of complicating factors.
- Breast cancer, if diagnosed early (before it spreads), has a 98% survival rate.
- That survival rate drops to 31% if diagnosed after it has spread through the body.
(The US CDC’s breast cancer “stat bite” page has more stats and interactive graphs, so click here to see those charts and get the more detailed low-down on mortality/survival rates with various different situations)
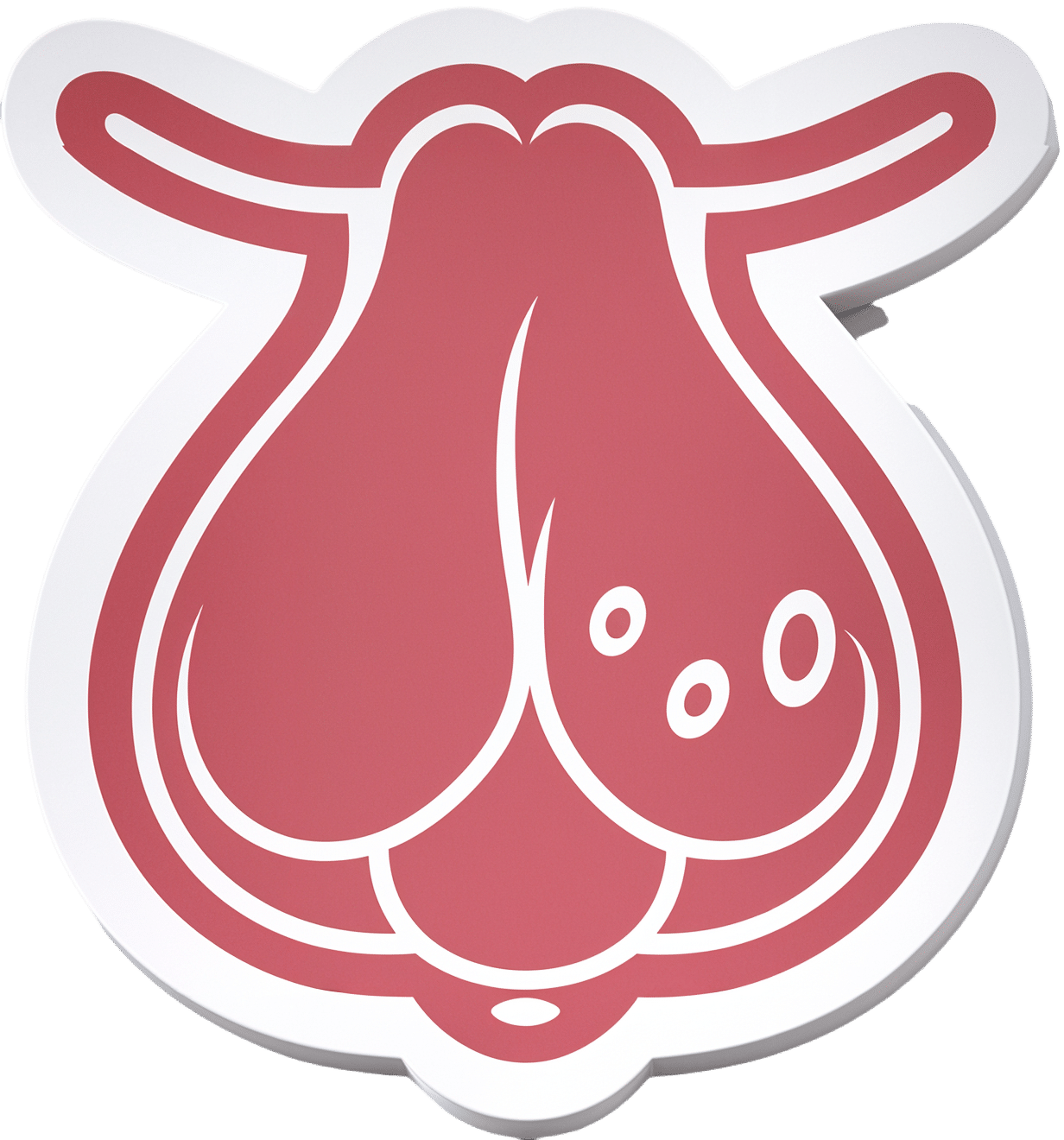
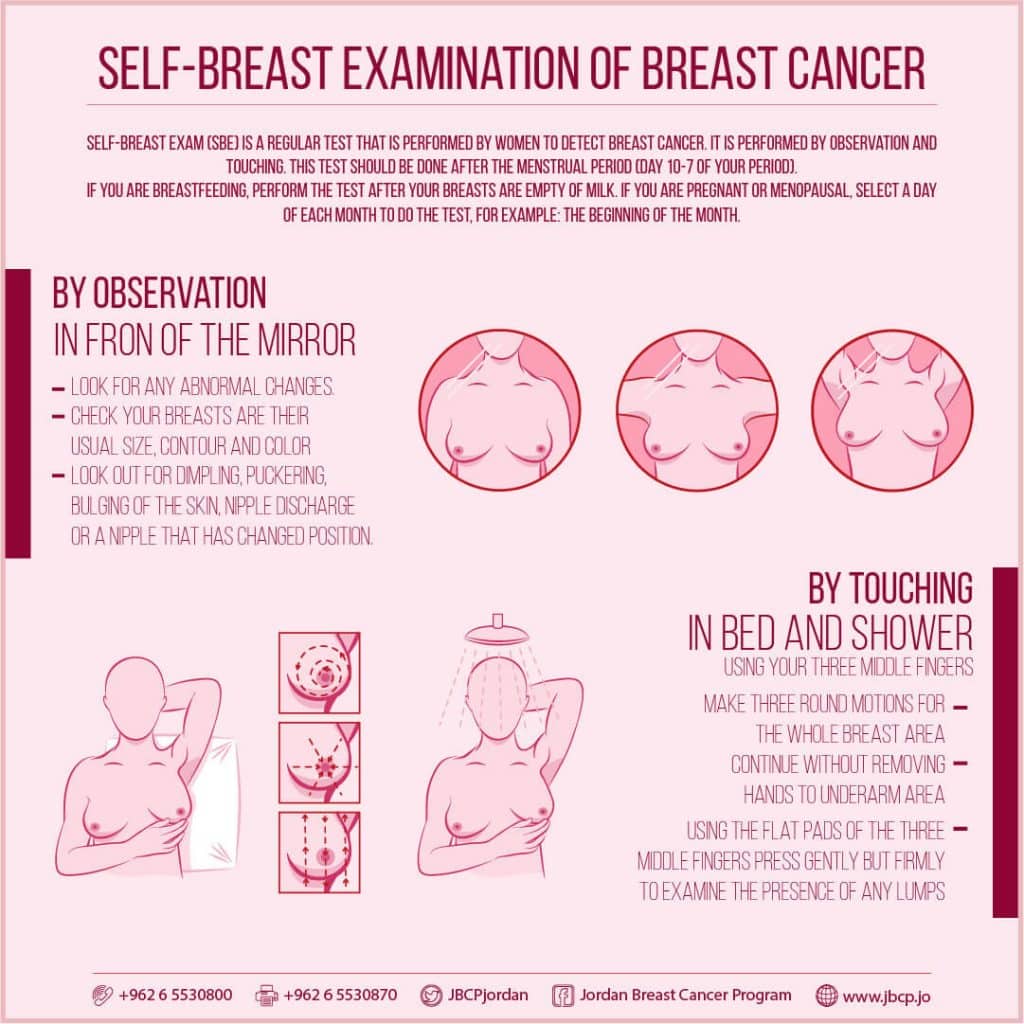
We think that the difference between 98% and 31% survival rates is more than enough reason to give ourselves a monthly self-check at the very least! You’ve probably seen how-to diagrams before, but here are instructions for your convenience:
(This graphic was created by the Jordan Breast Cancer Program—check them out, as they have lots of resources)
If you don’t have the opportunity to take matters into your own hands right now, rather than just promise yourself “I’ll do that later”, take this free 4-minute Breast Health Assessment from Aurora Healthcare. Again, we think the difference early diagnosis can make to your survival chances make these tests well worth it:
Click Here To Take The Free 4-Minute Breast Health Assessment!
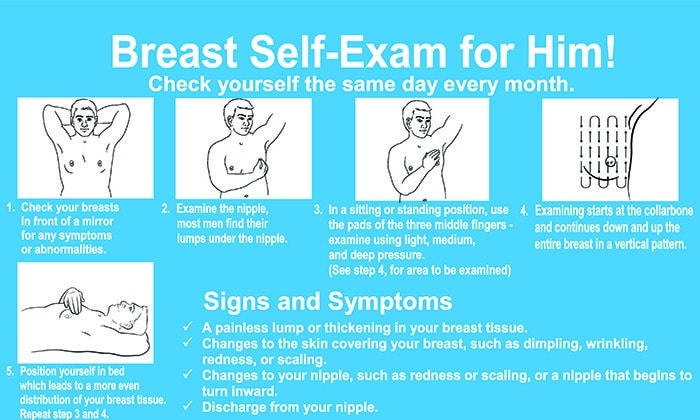
Lest we forget, men can also get breast cancer (the CDC has a page for men too), especially if over 50. But how do you check for breast cancer, when you don’t have breasts in the commonly-understood sense of the word?
So take a moment to do this (yes, really actually do it!), and set a reminder in your calendar to repeat it monthly—there really is no reason not to!
Take care of yourself; you’re important.
Share This Post
- Anyone (who has not had a double mastectomy*, anyway) can get breast cancer.
-
Happy Mind, Happy Life – by Dr. Rangan Chatterjee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Let’s start with a “why”. If happiness doesn’t strike you as a worthwhile goal in and of itself, Dr. Chatterjee discusses the health implications of happiness/unhappiness.
And, yes, including in studies where other factors were controlled for, so he shows how happiness/unhappiness does really have a causal role in health—it’s not just a matter of “breaking news: sick people are less happy”.
The author, a British GP (General Practitioner, the equivalent of what the US calls a “family doctor”) with decades of experience, has found a lot of value in the practice of holistic medicine. For this reason, it’s what he recommends to his patients at work, in his books, his blog, and his regular spot on a popular BBC breakfast show.
The writing style is relaxed and personable, without skimping on information density. Indeed, Dr. Chatterjee offers many pieces of holistic health advice, and dozens of practical exercises to boost your happiness and proof you against adversity.
Because, whatever motivational speakers may say, we can’t purely “think ourselves happy”; sometimes we have real external threats and bad things in life. But, we can still improve our experience of even these things, not to mention suffer less, and get through it in better shape with a smile at the end of it.
Bottom line: if you’d like to be happier and healthier (who wouldn’t?), then this book is a sure-fire way to set you on that path.
Click here to check out Happy Mind, Happy Life and upgrade yours!
Share This Post
-
Foods For Managing Hypothyroidism (incl. Hashimoto’s)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Foods for Managing Hypothyroidism
For any unfamiliar, hypothyroidism is the condition of having an underactive thyroid gland. The thyroid gland lives at the base of the front of your neck, and, as the name suggests, it makes and stores thyroid hormones. Those are important for many systems in the body, and a shortage typically causes fatigue, weight gain, and other symptoms.
What causes it?
This makes a difference in some cases to how it can be treated/managed. Causes include:
- Hashimoto’s thyroiditis, an autoimmune condition
- Severe inflammation (end result is similar to the above, but more treatable)
- Dietary deficiencies, especially iodine deficiency
- Secondary endocrine issues, e.g. pituitary gland didn’t make enough TSH for the thyroid gland to do its thing
- Some medications (ask your pharmacist)
We can’t do a lot about those last two by leveraging diet alone, but we can make a big difference to the others.
What to eat (and what to avoid)
There is nuance here, which we’ll go into a bit, but let’s start by giving the
one-linetwo-line summary that tends to be the dietary advice for most things:- Eat a nutrient-dense whole-foods diet (shocking, we know)
- Avoid sugar, alcohol, flour, processed foods (ditto)
What’s the deal with meat and dairy?
- Meat: avoid red and processed meats; poultry and fish are fine or even good (unless fried; don’t do that)
- Dairy: limit/avoid milk; but unsweetened yogurt and cheese are fine or even good
What’s the deal with plants?
First, get plenty of fiber, because that’s important to ease almost any inflammation-related condition, and for general good health for most people (an exception is if you have Crohn’s Disease, for example).
If you have Hashimoto’s, then gluten (as found in wheat, barley, and rye) may be an issue, but the jury is still out, science-wise. Here’s an example study for “avoid gluten” and “don’t worry about gluten”, respectively:
- The Effect of Gluten-Free Diet on Thyroid Autoimmunity in Women with Hashimoto’s Thyroiditis
- Doubtful Justification of the Gluten-Free Diet in the Course of Hashimoto’s Disease
So, you might want to skip it, to be on the safe side, but that’s up to you (and the advice of your nutritionist/doctor, as applicable).
A word on goitrogens…
Goitrogens are found in cruciferous vegetables and soy, both of which are very healthy foods for most people, but need some extra awareness in the case of hypothyroidism. This means there’s no need to abstain completely, but:
- Keep serving sizes small, for example a 100g serving only
- Cook goitrogenic foods before eating them, to greatly reduce goitrogenic activity
For more details, reading even just the abstract (intro summary) of this paper will help you get healthy cruciferous veg content without having a goitrogenic effect.
(as for soy, consider just skipping that if you suffer from hypothyroidism)
What nutrients to focus on getting?
- Top tier nutrients: iodine, selenium, zinc
- Also important: vitamin B12, vitamin D, magnesium, iron
Enjoy!
Share This Post
Related Posts
-
Coenzyme Q10 From Foods & Supplements
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Coenzyme Q10 and the difference it makes
Coenzyme Q10, often abbreviated to CoQ10, is a popular supplement, and is often one of the more expensive supplements that’s commonly found on supermarket shelves as opposed to having to go to more specialist stores or looking online.
What is it?
It’s a compound naturally made in the human body and stored in mitochondria. Now, everyone remembers the main job of mitochondria (producing energy), but they also protect cells from oxidative stress, among other things. In other words, aging.
Like many things, CoQ10 production slows as we age. So after a certain age, often around 45 but lifestyle factors can push it either way, it can start to make sense to supplement.
Does it work?
The short answer is “yes”, though we’ll do a quick breakdown of some main benefits, and studies for such, before moving on.
First, do bear in mind that CoQ10 comes in two main forms, ubiquinol and ubiquinone.
Ubiquinol is much more easily-used by the body, so that’s the one you want. Here be science:
What is it good for?
Benefits include:
- Against aging
- Against skin cancer
- Against breast cancer
- Against prostate cancer
- Against heart failure
- Against obesity
- Against diabetes
- Against Alzheimer’s
- Against Parkinson’s
Can we get it from foods?
Yes, and it’s equally well-absorbed through foods or supplementation, so feel free to go with whichever is more convenient for you.
Read: Intestinal absorption of coenzyme Q10 administered in a meal or as capsules to healthy subjects
If you do want to get it from food, you can get it from many places:
- Organ meats: the top source, though many don’t want to eat them, either because they don’t like them or some of us just don’t eat meat. If you do, though, top choices include the heart, liver, and kidneys.
- Fatty fish: sardines are up top, along with mackerel, herring, and trout
- Vegetables: leafy greens, and cruciferous vegetables e.g. cauliflower, broccoli, sprouts
- Legumes: for example soy, lentils, peanuts
- Nuts and seeds: pistachios come up top; sesame seeds are great too
- Fruit: strawberries come up top; oranges are great too
If supplementing, how much is good?
Most studies have used doses in the 100mg–200mg (per day) range.
However, it’s also been found to be safe at 1200mg (per day), for example in this high-quality study that found that higher doses resulted in greater benefit, in patients with early Parkinson’s Disease:
Effects of coenzyme Q10 in early Parkinson disease: evidence of slowing of the functional decline
Wondering where you can get it?
We don’t sell it (or anything else for that matter), and you can probably find it in your local supermarket or health food store. However, if you’d like to buy it online, here’s an example product on Amazon
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Future-Proof Your Brain
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This is Kimberly Wilson. She’s a psychologist, not a doctor, and/but her speciality is neurophysiology and brain health.
Here’s what she wants us to know…
Avoid this very common killer
As you’re probably aware, the #1 killer in the US is heart disease, followed by COVID, which effectively pushed everything down a place. Thereafter, we see cancer, followed by accidental injuries, stroke, and dementia (including Alzheimer’s).
Over in the UK, where Wilson is from, dementia (including Alzheimer’s disease) is the #1 killer, followed by heart disease and then respiratory diseases (including COVID), and then stroke, then cancer.
As ever, what’s good for the heart is good for the brain, so many of the same interventions will help avoid both. With regard to some of the other differences in order, the reasons are mostly due to differences in the two countries’ healthcare systems and firearms laws.
It’s worth noting, though, that the leading cause of death in young people (aged 15–19) is suicide in the UK; in the US it’s nominally accidental injuries first (e.g. accidental shootings) with intentional suicide in the second spot.
In other words… Young or old, mental health is a serious health category that kills literally the most people in the UK, and also makes the top spots in the US.
Avoid the early killer
Given the demographics of most of our readership, chances are you’ve already lived past your teens and twenties. That’s not to say that suicide is no longer a risk, though, and it’s also worth noting that while mental health issues are invisible, they’re still physical illnesses (the brain is also an organ, after all!), so this isn’t something where you can simply “decide not to” and that’s you set, safe for life. So, please do continue to take good care in that regard.
We wrote about this previously, here:
How To Stay Alive (When You Really Don’t Want To)
Avoid the later killer
Wilson talks about how a recent survey found that…
- while nearly half of adults say dementia is the disease they fear most,
- only a third of those thought you could do anything to avoid it, and
- just 1% could name the 7 known risk factors.
Quick test: can you name the 7 known risk factors?
Please take a moment to actually try (this kind of mental stimulation is good in any case), and count them out on your fingers (or write them down), and then…
When you’re ready: click here to see the answer!
How many did you get? If you got them all, well done. If not, then well, now you know, so that’s good.
So, with those 7 things in mind, the first obvious advice is to take care of those things.
Taking an evidence-based medicine approach, Wilson recommends some specific interventions that will each improve one or more of those things, directly or indirectly:
Eating right
Wilson is a big fan of “nutritional psychiatry” and feeding one’s brain properly. We wrote about this, here:
The 6 Pillars Of Nutritional Psychiatry
As well as agreeing with the obvious “eat plenty of fiber, different-colored plants, and plenty of greens and beans”, Wilson specifically also champions getting enough of vitamins B9, B12, and D, as well as getting a healthy dose of omega-3 fatty acids.
She also recommends intermittent fasting, if that’s a reasonable option for you—but advocates for not worrying about it, if it’s not easy for you. For example, if you are diabetic, or have (or have a history with) some kind of eating disorder(s), then it’s probably not usefully practicable. But for most people, it can reduce systemic inflammation, which means also reducing neuroinflammation.
Managing stress right
Here she advocates for three main things:
- Mindful meditation (see: Evidence-Based, No-Frills Mindfulness)
- Psychological resilience (see: Building Psychological Resilience)
- Mindful social media use (see: Making Social Media Work For Your Mental Health)
Managing money right
Not often we talk about this in a health science publication as opposed to a financial planning publication, but the fact is that a lot of mental distress, which goes on to have a huge impact on the brain, is rooted in financial stresses.
And, of course, it’s good to be able to draw on financial resources to directly fund one’s good health, but that is the secondary consideration here—the financial stress is the biggest issue, and you can’t CBT your way out of debt, for example.
Therapists often face this, and what has been referred to informally by professionals in the field as “Shit Life Syndrome”—and there’s only so much that therapy can do about that.
We’re not a financial publication, but one recommendation we’ll drop is that if you don’t currently have budgeting software that you use, this writer personally uses and swears by YNAB (You Need A Budget), so maybe check that out if you don’t already have everything covered in that regard. It’s not free, but there is a 34-day free trial.
Therapy can be very worthwhile nonetheless
Wilson notes that therapy is like non-invasive brain surgery (because of neuroplasticity, it’s literally changing physical things in your brain).
It’s not a magic bullet and it’s not the right choice for everyone, but it’s worth considering, and even self-therapy can yield benefits for many:
The Gym For Your Mental Health: Getting The Most Out Of Therapy
Sleeping right
Sleep is not only critical for health in general and brain health in particular, it’s also most of when our glymphatic system does clean-up in the brain (essential for avoiding Alzheimer’s & Parkinson’s, amongst other diseases):
How To Clean Your Brain (Glymphatic Health Primer)
Want to know more from Kimberley Wilson?
We reviewed a book of hers recently, here:
Unprocessed: What your Diet Is Doing To Your Brain – by Kimberley Wilson
However, much of what we shared today was sourced from another book of hers that we haven’t reviewed yet but probably will do one of these days:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is ‘doll therapy’ for people with dementia? And is it backed by science?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The way people living with dementia experience the world can change as the disease progresses. Their sense of reality or place in time can become distorted, which can cause agitation and distress.
One of the best ways to support people experiencing changes in perception and behaviour is to manage their environment. This can have profound benefits including reducing the need for sedatives.
One such strategy is the use of dolls as comfort aids.
Jack Cronkhite/Shutterstock What is ‘doll therapy’?
More appropriately referred to as “child representation”, lifelike dolls (also known as empathy dolls) can provide comfort for some people with dementia.
Memories from the distant past are often more salient than more recent events in dementia. This means that past experiences of parenthood and caring for young children may feel more “real” to a person with dementia than where they are now.
Hallucinations or delusions may also occur, where a person hears a baby crying or fears they have lost their baby.
Providing a doll can be a tangible way of reducing distress without invalidating the experience of the person with dementia.
Some people believe the doll is real
A recent case involving an aged care nurse mistreating a dementia patient’s therapy doll highlights the importance of appropriate training and support for care workers in this area.
For those who do become attached to a therapeutic doll, they will treat the doll as a real baby needing care and may therefore have a profound emotional response if the doll is mishandled.
It’s important to be guided by the person with dementia and only act as if it’s a real baby if the person themselves believes that is the case.
What does the evidence say about their use?
Evidence shows the use of empathy dolls may help reduce agitation and anxiety and improve overall quality of life in people living with dementia.
Child representation therapy falls under the banner of non-pharmacological approaches to dementia care. More specifically, the attachment to the doll may act as a form of reminiscence therapy, which involves using prompts to reconnect with past experiences.
Interacting with the dolls may also act as a form of sensory stimulation, where the person with dementia may gain comfort from touching and holding the doll. Sensory stimulation may support emotional well-being and aid commnication.
However, not all people living with dementia will respond to an empathy doll.
It depends on a person’s background. Shutterstock The introduction of a therapeutic doll needs to be done in conjunction with careful observation and consideration of the person’s background.
Empathy dolls may be inappropriate or less effective for those who have not previously cared for children or who may have experienced past birth trauma or the loss of a child.
Be guided by the person with dementia and how they respond to the doll.
Are there downsides?
The approach has attracted some controversy. It has been suggested that child representation therapy “infantilises” people living with dementia and may increase negative stigma.
Further, the attachment may become so strong that the person with dementia will become upset if someone else picks the doll up. This may create some difficulties in the presence of grandchildren or when cleaning the doll.
The introduction of child representation therapy may also require additional staff training and time. Non-pharmacological interventions such as child representation, however, have been shown to be cost-effective.
Could robots be the future?
The use of more interactive empathy dolls and pet-like robots is also gaining popularity.
While robots have been shown to be feasible and acceptable in dementia care, there remains some contention about their benefits.
While some studies have shown positive outcomes, including reduced agitation, others show no improvement in cognition, behaviour or quality of life among people with dementia.
Advances in artificial intelligence are also being used to help support people living with dementia and inform the community.
Viv and Friends, for example, are AI companions who appear on a screen and can interact with the person with dementia in real time. The AI character Viv has dementia and was co-created with women living with dementia using verbatim scripts of their words, insights and experiences. While Viv can share her experience of living with dementia, she can also be programmed to talk about common interests, such as gardening.
These companions are currently being trialled in some residential aged care facilities and to help educate people on the lived experience of dementia.
How should you respond to your loved one’s empathy doll?
While child representation can be a useful adjunct in dementia care, it requires sensitivity and appropriate consideration of the person’s needs.
People living with dementia may not perceive the social world the same way as a person without dementia. But a person living with dementia is not a child and should never be treated as one.
Ensure all family, friends and care workers are informed about the attachment to the empathy doll to help avoid unintentionally causing distress from inappropriate handling of the doll.
If using an interactive doll, ensure spare batteries are on hand.
Finally, it is important to reassess the attachment over time as the person’s response to the empathy doll may change.
Nikki-Anne Wilson, Postdoctoral Research Fellow, Neuroscience Research Australia (NeuRA), UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: