What pathogen might spark the next pandemic? How scientists are preparing for ‘disease X’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Before the COVID pandemic, the World Health Organization (WHO) had made a list of priority infectious diseases. These were felt to pose a threat to international public health, but where research was still needed to improve their surveillance and diagnosis. In 2018, “disease X” was included, which signified that a pathogen previously not on our radar could cause a pandemic.
While it’s one thing to acknowledge the limits to our knowledge of the microbial soup we live in, more recent attention has focused on how we might systematically approach future pandemic risks.
Former US Secretary of Defense Donald Rumsfeld famously talked about “known knowns” (things we know we know), “known unknowns” (things we know we don’t know), and “unknown unknowns” (the things we don’t know we don’t know).
Although this may have been controversial in its original context of weapons of mass destruction, it provides a way to think about how we might approach future pandemic threats.

Influenza: a ‘known known’
Influenza is largely a known entity; we essentially have a minor pandemic every winter with small changes in the virus each year. But more major changes can also occur, resulting in spread through populations with little pre-existing immunity. We saw this most recently in 2009 with the swine flu pandemic.
However, there’s a lot we don’t understand about what drives influenza mutations, how these interact with population-level immunity, and how best to make predictions about transmission, severity and impact each year.
The current H5N1 subtype of avian influenza (“bird flu”) has spread widely around the world. It has led to the deaths of many millions of birds and spread to several mammalian species including cows in the United States and marine mammals in South America.
Human cases have been reported in people who have had close contact with infected animals, but fortunately there’s currently no sustained spread between people.
While detecting influenza in animals is a huge task in a large country such as Australia, there are systems in place to detect and respond to bird flu in wildlife and production animals.

It’s inevitable there will be more influenza pandemics in the future. But it isn’t always the one we are worried about.
Attention had been focused on avian influenza since 1997, when an outbreak in birds in Hong Kong caused severe disease in humans. But the subsequent pandemic in 2009 originated in pigs in central Mexico.
Coronaviruses: an ‘unknown known’
Although Rumsfeld didn’t talk about “unknown knowns”, coronaviruses would be appropriate for this category. We knew more about coronaviruses than most people might have thought before the COVID pandemic.
We’d had experience with severe acute respiratory syndrome (SARS) and Middle Eastern respiratory syndrome (MERS) causing large outbreaks. Both are caused by viruses closely related to SARS-CoV-2, the coronavirus that causes COVID. While these might have faded from public consciousness before COVID, coronaviruses were listed in the 2015 WHO list of diseases with pandemic potential.
Previous research into the earlier coronaviruses proved vital in allowing COVID vaccines to be developed rapidly. For example, the Oxford group’s initial work on a MERS vaccine was key to the development of AstraZeneca’s COVID vaccine.
Similarly, previous research into the structure of the spike protein – a protein on the surface of coronaviruses that allows it to attach to our cells – was helpful in developing mRNA vaccines for COVID.
It would seem likely there will be further coronavirus pandemics in the future. And even if they don’t occur at the scale of COVID, the impacts can be significant. For example, when MERS spread to South Korea in 2015, it only caused 186 cases over two months, but the cost of controlling it was estimated at US$8 billion (A$11.6 billion).

The 25 viral families: an approach to ‘known unknowns’
Attention has now turned to the known unknowns. There are about 120 viruses from 25 families that are known to cause human disease. Members of each viral family share common properties and our immune systems respond to them in similar ways.
An example is the flavivirus family, of which the best-known members are yellow fever virus and dengue fever virus. This family also includes several other important viruses, such as Zika virus (which can cause birth defects when pregnant women are infected) and West Nile virus (which causes encephalitis, or inflammation of the brain).
The WHO’s blueprint for epidemics aims to consider threats from different classes of viruses and bacteria. It looks at individual pathogens as examples from each category to expand our understanding systematically.
The US National Institute of Allergy and Infectious Diseases has taken this a step further, preparing vaccines and therapies for a list of prototype pathogens from key virus families. The goal is to be able to adapt this knowledge to new vaccines and treatments if a pandemic were to arise from a closely related virus.
Pathogen X, the ‘unknown unknown’
There are also the unknown unknowns, or “disease X” – an unknown pathogen with the potential to trigger a severe global epidemic. To prepare for this, we need to adopt new forms of surveillance specifically looking at where new pathogens could emerge.
In recent years, there’s been an increasing recognition that we need to take a broader view of health beyond only thinking about human health, but also animals and the environment. This concept is known as “One Health” and considers issues such as climate change, intensive agricultural practices, trade in exotic animals, increased human encroachment into wildlife habitats, changing international travel, and urbanisation.
This has implications not only for where to look for new infectious diseases, but also how we can reduce the risk of “spillover” from animals to humans. This might include targeted testing of animals and people who work closely with animals. Currently, testing is mainly directed towards known viruses, but new technologies can look for as yet unknown viruses in patients with symptoms consistent with new infections.
We live in a vast world of potential microbiological threats. While influenza and coronaviruses have a track record of causing past pandemics, a longer list of new pathogens could still cause outbreaks with significant consequences.
Continued surveillance for new pathogens, improving our understanding of important virus families, and developing policies to reduce the risk of spillover will all be important for reducing the risk of future pandemics.
This article is part of a series on the next pandemic.
Allen Cheng, Professor of Infectious Diseases, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Topping Up Testosterone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Testosterone Drop
Testosterone levels decline amongst men over a certain age. Exactly when depends on the individual and also how we measure it, but the age of 45 is a commonly-given waypoint for the start of this decline.
(the actual start is usually more like 20, but it’s a very small decline then, and speeds up a couple of decades later)
This has been called “the male menopause”, or “the andropause”.
Both terms are a little misleading, but for lack of a better term, “andropause” is perhaps not terrible.
Why “the male menopause” is misleading:
To call it “the male menopause” suggests that this is when men’s menstruation stops. Which for cis men at the very least, is simply not a thing they ever had in the first place, to stop (and for trans men it’s complicated, depending on age, hormones, surgeries, etc).
Why “the andropause” is misleading:
It’s not a pause, and unlike the menopause, it’s not even a stop. It’s just a decline. It’s more of an andro-pitter-patter-puttering-petering-out.
Is there a better clinical term?
Objectively, there is “late-onset hypogonadism” but that is unlikely to be taken up for cultural reasons—people stigmatize what they see as a loss of virility.
Terms aside, what are the symptoms?
❝Andropause or late-onset hypogonadism is a common disorder which increases in prevalence with advancing age. Diagnosis of late-onset of hypogonadism is based on presence of symptoms suggestive of testosterone deficiency – prominent among them are sexual symptoms like…❞
…and there we’d like to continue the quotation, but if we list the symptoms here, it won’t get past a lot of filters because of the words used. So instead, please feel free to click through:
Source: Andropause: Current concepts
Can it be safely ignored?
If you don’t mind the sexual symptoms, then mostly, yes!
However, there are a few symptoms we can mention here that are not so subjective in their potential for harm:
- Depression
- Loss of muscle mass
- Increased body fat
Depression kills, so this does need to be taken seriously. See also:
The Mental Health First-Aid That You’ll Hopefully Never Need
(the above is a guide to managing depression, in yourself or a loved one)
Loss of muscle mass means being less robust against knocks and falls later in life
Loss of muscle mass also means weaker bones (because the body won’t make bones stronger than it thinks they need to be, so bone will follow muscle in this regard—in either direction)
See also:
- Resistance Is Useful! (Especially As We Get Older)
- Protein vs Sarcopenia
- Fall Special (How to Proof Yourself Against Falls)
Increased body fat means increased risk of diabetes and heart disease, as a general rule of thumb, amongst other problems.
Will testosterone therapy help?
That’s something to discuss with your endocrinologist, but for most men whose testosterone levels are lower than is ideal for them, then yes, taking testosterone to bring them [back] to “normal” levels can make you happier and healthier (though it’s certainly not a cure-all).
See for example:
Testosterone Therapy Improves […] and […] in Hypogonadal Men
(Sorry, we’re not trying to be clickbaity, there are just some words we can’t use without encountering software problems)
Here’s a more comprehensive study that looked at 790 men aged 65 or older, with testosterone levels below a certain level. It looked at the things we can’t mention here, as well as physical function and general vitality:
❝The increase in testosterone levels was associated with significantly increased […] activity, as assessed by the Psychosexual Daily Questionnaire (P<0.001), as well as significantly increased […] desire and […] function.
The percentage of men who had an increase of at least 50 m in the 6-minute walking distance did not differ significantly between the two study groups in the Physical Function Trial but did differ significantly when men in all three trials were included (20.5% of men who received testosterone vs. 12.6% of men who received placebo, P=0.003).
Testosterone had no significant benefit with respect to vitality, as assessed by the Functional Assessment of Chronic Illness Therapy–Fatigue scale, but men who received testosterone reported slightly better mood and lower severity of depressive symptoms than those who received placebo❞
Source: Effects of Testosterone Treatment in Older Men
We strongly recommend, by the way, when a topic is of interest to you to read the paper itself, because even the extract above contains some subjectivity, for example what is “slightly better”, and what is “no significant benefit”.
That “slightly better mood and lower severity of depressive symptoms”, for example, has a P value of 0.004 in their data, which is an order of magnitude more significant than the usual baseline for significance (P<0.05).
And furthermore, that “no significant benefit with respect to vitality” is only looking at either the primary outcome aggregated goal or the secondary FACIT score whose secondary outcome had a P value of 0.06, which just missed the cut-off for significance, and neglects to mention that all the other secondary outcome metrics for men involved in the vitality trial were very significant (ranging from P=0.04 to P=0.001)
Click here to see the results table for the vitality trial
Will it turn me into a musclebound angry ragey ‘roidmonster?
Were you that kind of person before your testosterone levels declined? If not, then no.
Testosterone therapy seeks only to return your testosterone levels to where they were, and this is done through careful monitoring and adjustment. It’d take a lot more than (responsible) endocrinologist-guided hormonal therapy to turn you into Marvel’s “Wolverine”.
Is testosterone therapy safe?
A question to take to your endocrinologist because everyone’s physiology is different, but a lot of studies do support its general safety for most people who are prescribed it.
As with anything, there are risks to be aware of, though. Perhaps the most critical risk is prostate cancer, and…
❝In a large meta-analysis of 18 prospective studies that included over 3500 men, there was no association between serum androgen levels and the risk of prostate cancer development
For men with untreated prostate cancer on active surveillance, TRT remains controversial. However, several studies have shown that TRT is not associated with progression of prostate cancer as evidenced by either PSA progression or gleason grade upstaging on repeat biopsy.
Men on TRT should have frequent PSA monitoring; any major change in PSA (>1 ng/mL) within the first 3-6 months may reflect the presence of a pre-existing cancer and warrants cessation of therapy❞
Those are some select extracts, but any of this may apply to you or your loved one, we recommend to read in full about this and other risks:
Risks of testosterone replacement therapy in men
See also: Prostate Health: What You Should Know
Beyond that… If you are prone to baldness, then taking testosterone will increase that tendency. If that’s a problem for you, then it’s something to know about. There are other things you can take/use for that in turn, so maybe we’ll do a feature on those one of these days!
For now, take care!
Share This Post
-
Yoga that Helps You on the Loo
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How This Video Helps You Poo
When you’re feeling a bit bloated, Yoga With Bird’s 10-minute yoga routine promises to help you release…your gas. And, perhaps, more.
From a tabletop flow to soothing twists, each pose allows you to sync your breath with movement, helping to promote organic relief.
With options to modify with pillows for extra support, this video (below) caters to everyone needing a digestive reset.
Other Toilet Tricks
If yoga isn’t your thing, or you’re interested in trying to use different methods to make your visits to the bathroom a bit easier, we’ve spoken about the ways to manage gut health, and use of probiotics or fiber, and even the prevention of hemorrhoids.
Namaste and goodbye to bloat!
How was the video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
-
Avocado vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing avocado to blueberries, we picked the avocado.
Why?
These two fruits aren’t as similar as some of the comparisons we’ve made—we often go for “can be used in the same way culinarily” comparisons. But! They are both popularly in the “superfood” category, so it’s interesting to consider:
In terms of macros, avocado has more protein, (healthy!) fat, and fiber, while blueberries have more carbs. An easy win for avocado here, unless you’re on a calorie-controlled diet perhaps, since avocado is also higher in those. About that fat; it’s mostly monounsaturated, with some polyunsaturated and saturated, and is famously a good source of omega-3 in the form of ALA.
In the category of vitamins, avocado has more of vitamins A, B1, B2, B3, B5, B6, B7, B9, C, E, K, and choline, while blueberries are not higher in any vitamins. So, not a tricky decision here.
When it comes to minerals, avocado has more calcium, copper, iron, magnesium, phosphorus, potassium, selenium, and zinc, while blueberries are higher in manganese. Another win for avocados.
There is one other category that’s important to consider in this case, and that’s polyphenols. We’d be here all day if we listed them all, but in total, blueberries have about 1193x the polyphenol content that avocados do. Blueberries got the reputation for antioxidant properties for a reason; it is well-deserved!
So, out of the two, we declare avocado the overall more nutritious of the two, but blueberries absolutely deserve the acclaim they get also.
Want to learn more?
You might like to read:
Give Us This Day Our Daily Dozen
Take care!
Share This Post
Related Posts
-
Good (Or Bad) Health Starts With Your Blood
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Blood Should Be Only Slightly Thicker Than Water
This is Dr. Casey Means, a physician, lecturer (mostly at Stanford), and CMO of a metabolic health company, Levels, as well as being Associate Editor of the International Journal of Diabetes Reversal and Prevention, where she serves alongside such names as Dr. Colin Campbell, Dr. Joel Fuhrman, Dr. Michael Greger, Dr. William Li, Dr. Dean Ornish, and you get the idea: it’s a star-studded cast.
What does she want us to know?
The big blood problem:
❝We’re spending 3.8 trillion dollars a year on healthcare costs in the U.S., and the reality is that people are getting sicker, fatter, and more depressed.
Over 50% of Americans have pre-diabetes or type 2 diabetes; it’s insane, that number should be close to zero.❞
~ Dr. Casey Means
Indeed, pre-diabetes and especially type 2 diabetes should be very avoidable in any wealthy nation.
Unfortunately, the kind of diet that avoids it tends to rely on having at least 2/3 of the following:
- Money
- Time
- Knowledge
For example:
- if you have money and time, you can buy lots of fresh ingredients without undue worry, and take the time to carefully prep and cook them
- if you have money and knowledge you can have someone else shop and cook for you, or at least get meal kits delivered
- if you have time and knowledge, you can actually eat very healthily on a shoestring budget
If you have all three, then the world’s your oyster mushroom steak sautéed in extra virgin olive oil with garlic and cracked black pepper served on a bed of Swiss chard and lashed with Balsamic vinegar.
However, many Americans aren’t in the happy position of having at least 2/3, and a not-insignificant portion of the population don’t even have 1/3.
As an aside: there is a food scientist and chef who’s made it her mission to educate people about food that’s cheap, easy, and healthy:
…but today is about Dr. Means, so, what does she suggest?
Know
thyselfthy blood sugarsDr. Means argues (reasonably; this is well-backed up by general scientific consensus) that much of human disease stems from the diabetes and pre-diabetes that she mentioned above, and so we should focus on that most of all.
Our blood sugar levels being unhealthy will swiftly lead to other metabolic disorders:
Heart disease and non-alcoholic fatty liver disease are perhaps first in line, but waiting in the wings are inflammation-mediated autoimmune disorders, and even dementia, because neuroinflammation is at least as bad as inflammation anywhere else, arguably worse, and our brain can only be as healthy as the blood that feeds it and takes things that shouldn’t be there away.
Indeed,
❝Alzheimer’s dementia is now being called type 3 diabetes because it’s so related to blood sugar❞
~ Dr. Casey Means
…which sounds like a bold claim, but it’s true, even if the name is not “official” yet, it’s well-established in professional circulation:
❝We conclude that the term “type 3 diabetes” accurately reflects the fact that AD represents a form of diabetes that selectively involves the brain and has molecular and biochemical features that overlap with both T1DM and T2DM❞
~ Dr. Suzanne M. de la Monte & Dr. Jack Wands
Read in full: Alzheimer’s Disease Is Type 3 Diabetes–Evidence Reviewed ← this is from the very respectable Journal of Diabetes Science and Technology.
What to do about it
Dr. Means suggests we avoid the “glucose roller-coaster” that most Americans are on, meaning dramatic sugar spikes, or to put it in sciencese: high glycemic variability.
This leads to inflammation, oxidative stress, glycation (where sugar sticks to proteins and DNA), and metabolic dysfunction. Then there’s the flipside: reactive hypoglycemia, a result of a rapid drop in blood sugar after a spike, can cause anxiety, fatigue, weakness/trembling, brain fog, and of course cravings. And so the cycle repeats.
But it doesn’t have to!
By taking it upon ourselves to learn about what causes our blood sugars to rise suddenly or gently, we can manage our diet and other lifestyle factors accordingly.
And yes, it’s not just about diet, Dr. Means tells us. While added sugar and refined carbohydrates or indeed the main drivers of glycemic variability, our sleep, movement, stress management, and even toxin exposure play important parts too.
One way to do this, that Dr. Means recommends, is with a continuous glucose monitor:
Track Your Blood Sugars For Better Personalized Health
Another way is to just apply principles that work for almost everyone:
10 Ways To Balance Blood Sugars
Want to know more from Dr. Means?
You might like her book:
Good Energy – by Dr. Casey Means
…which goes into this in far more detail than we have room to today.
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healthiest-Three-Nut Butter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’re often telling you to “diversify your nuts”, so here’s a great way to get in three at once with no added sugar, palm oil, or preservatives, and only the salt you choose to put in. We’ve picked three of the healthiest nuts around, but if you happen to be allergic, don’t worry, we’ve got you covered too.
You will need
- 1 cup almonds (if allergic, substitute a seed, e.g. chia, and make it ½ cup)
- 1 cup walnuts (if allergic, substitute a seed, e.g. pumpkin, and make it ½ cup)
- 1 cup pistachios (if allergic, substitute a seed, e.g. poppy, and make it ½ cup)
- 1 tbsp almond oil (if allergic, substitute extra virgin olive oil) (if you prefer sweet nut butter, substitute 1 tbsp maple syrup; the role here is to emulsify the nuts, and this will do the same job)
- Optional: ¼ tsp MSG or ½ tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1a) If using nuts, heat your oven to 350℉ / 180℃. Place the nuts on a baking tray lined with baking paper, and bake/roast for about 10 minutes, but keep an eye on it to ensure the nuts don’t burn, and jiggle them if necessary to ensure they toast evenly. Once done, allow to cool.
1b) If using seeds, you can either omit that step, or do the same for 5 minutes if you want to, but really it’s not necessary.
2) Blend all ingredients (nuts/seeds, oil, MSG/salt) in a high-speed blender. Note: this will take about 10 minutes in total, and we recommend you do it in 30-second bursts so as to not overheat the motor. You also may need to periodically scrape the mixture down the side of the blender, to ensure a smooth consistency.
3) Transfer to a clean jar, and enjoy at your leisure:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Why You Should Diversify Your Nuts!
- Sesame Seeds vs Poppy Seeds – Which is Healthier?
- If You’re Not Taking Chia, You’re Missing Out
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
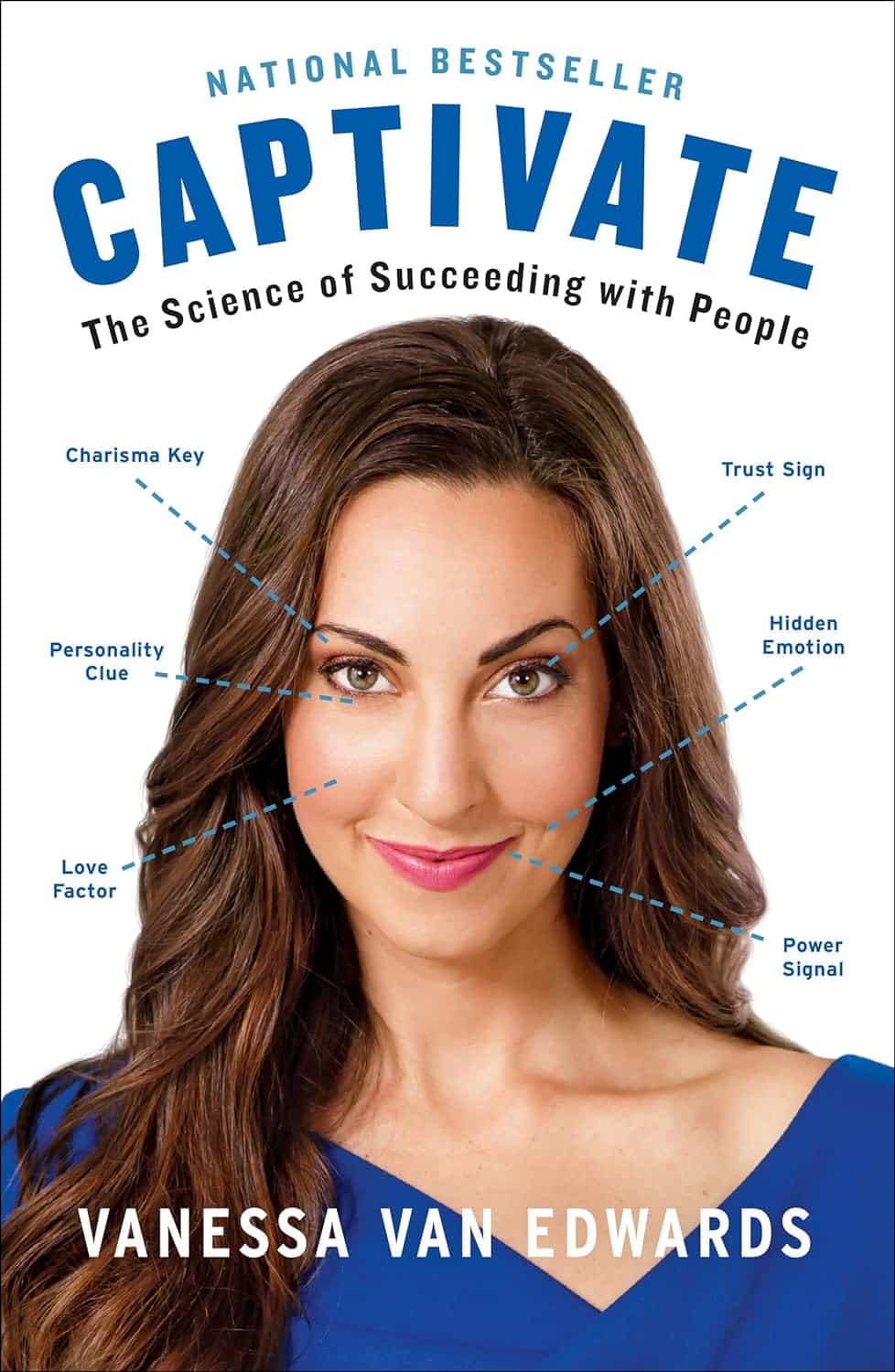
Captivate – by Vanessa van Edwards
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book isn’t just for one area of human interactions. It covers everything from the boardroom to the bedroom (not necessarily a progression with the same person!), business associates, friends, partners, kids, and more.
She presents information in a layered manner, covering for example, chapter-by-chapter:
- the first five minutes
- the first five hours
- the first five days
She also covers such things as:
- starting conversations in a way that makes you memorable (without making it weird!)
- the importance of really listening (and how to do that)
- collecting like-minded people appropriately
- introducing other people! Because a) it’s not all about you, but also b) you’re the person who knows everybody now
- where to stand at parties / networking events!
- dating and early-days dating messages
- reading the room, reading the people
All in all, a great resource for anyone who wants to make (and maintain!) meaningful relationships with those around you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: