What are plyometric exercises? How all that hopping and jumping builds strength, speed and power
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you’ve ever seen people at the gym or the park jumping, hopping or hurling weighted balls to the ground, chances are they were doing plyometric exercises.
Examples include:
- box jumps, where you repeatedly leap quickly on and off a box
- lateral skater hops, where you bound from side to side like a speeding ice skater
- rapidly throwing a heavy medicine ball against a wall, or to the ground
- single leg hops, which may involve hopping on the spot or through an obstacle course
- squat jumps, where you repeatedly squat and then launch yourself into the air.

There are many more examples of plyometric exercises.
What ties all these moves together is that they use what’s known as the “stretch shortening cycle”. This is where your muscles rapidly stretch and then contract.

Potential benefits
Research shows incorporating plyometric exercise into your routine can help you:
- jump higher
- sprint faster
- reduce the chances of getting a serious sporting injuries such as anterior cruciate ligament (ACL) tears
- build muscle strength
- improve bone mineral density (especially when combined with resistance training such as weight lifting), which is particularly important for women and older people at risk of falls.
Studies have found plyometric exercises can help:
- older people who want to retain and build muscle strength, boost bone health, improve posture and reduce the risk of falls
- adolescent athletes who want to build the explosive strength needed to excel in sports such as athletics, tennis, soccer, basketball and football
- female athletes who want to jump higher or change direction quickly (a useful skill in many sports)
- endurance runners who want to boost physical fitness, run time and athletic performance.
And when it comes to plyometric exercises, you get out what you put in.
Research has found the benefits of plyometrics are significantly greater when every jump was performed with maximum effort.

Potential risks
All exercise comes with risk (as does not doing enough exercise!)
Plyometrics are high-intensity activities that require the body to absorb a lot of impact when landing on the ground or catching medicine balls.
That means there is some risk of musculoskeletal injury, particularly if the combination of intensity, frequency and volume is too high.
You might miss a landing and fall, land in a weird way and crunch your ankle, or get a muscle tear if you’re overdoing it.
The National Strength and Conditioning Association, a US educational nonprofit that uses research to support coaches and athletes, recommends:
- a maximum of one to three plyometric sessions per week
- five to ten repetitions per set and
- rest periods of one to three minutes between sets to ensure complete muscle recovery.

One meta-analysis, where researchers looked at many studies, found plyometric training was feasible and safe, and could improve older people’s performance, function and health.
Overall, with appropriate programming and supervision, plyometric exercise can be a safe and effective way to boost your health and athletic performance.
Justin Keogh, Associate Dean of Research, Faculty of Health Sciences and Medicine, Bond University and Mandy Hagstrom, Senior Lecturer, Exercise Physiology. School of Health Sciences, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Kiwi vs Passion Fruit – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kiwi to passion fruit, we picked the passion fruit.
Why?
This fruit is so passionate about delivery nutrient-dense goodness, that at time of writing, nothing has beaten it yet!
In terms of macros, passion fruit has a little more protein, as well as 50% more carbs, and/but more than 3x the fiber. That last stat is particularly impressive, and also results in passion fruit having a much lower glycemic index, too. In short, a clear win for passion fruit in the macros category.
In the category of vitamins, kiwi has more of vitamins B9, C, E, and K, while passion fruit has more of vitamins A, B2, B3, and B6, making for a tie this time.
As for minerals, kiwi has more calcium, copper, manganese, and zinc, while passion fruit has more iron, magnesium, phosphorus, potassium, and selenium, resulting in a modest, marginal win for passion fruit in this category.
Adding up the categories gives a convincing win for passion fruit, but by all means enjoy either or both; diversity is good! And kiwi has its merits too (for example, it’s particularly high in vitamin K, appropriately enough).
Want to learn more?
You might like to read:
Top 8 Fruits That Prevent & Kill Cancer
Enjoy!
Share This Post
-
Elon Musk says ‘disc replacement’ worked for him. But evidence this surgery helps chronic pain is lacking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Last week in a post on X, owner of the platform Elon Musk recommended people look into disc replacement if they’re experiencing severe neck or back pain.
According to a biography of the billionaire, he’s had chronic back and neck pain since he tried to “judo throw” a 350-pound sumo wrestler in 2013 at a Japanese-themed party for his 42nd birthday, and blew out a disc at the base of his neck.
In comments following the post, Musk said the surgery was a “gamechanger” and reduced his pain significantly.
Musk’s original post has so far had more than 50 million views and generated controversy. So what is disc replacement surgery and what does the evidence tells us about its benefits and harms?
What’s involved in a disc replacement?
Disc replacement is a type of surgery in which one or more spinal discs (a cushion between the spine bones, also known as vertebrae) are removed and replaced with an artificial disc to retain movement between the vertebrae. Artificial discs are made of metal or a combination of metal and plastic.
Disc replacement may be performed for a number of reasons, including slipped discs in the neck, as appears to be the case for Musk.
Disc replacement is major surgery. It requires general anaesthesia and the operation usually takes 2–4 hours. Most people stay in hospital for 2–7 days. After surgery patients can walk but need to avoid things like strenuous exercise and driving for 3–6 weeks. People may be required to wear a neck collar (following neck surgery) or a back brace (following back surgery) for about 6 weeks.
Costs vary depending on whether you have surgery in the public or private health system, if you have private health insurance, and your level of coverage if you do. In Australia, even if you have health insurance, a disc replacement surgery may leave you more than A$12,000 out of pocket.
Disc replacement surgery is not performed as much as other spinal surgeries (for example, spinal fusion) but its use is increasing.
In New South Wales for example, rates of privately-funded disc replacement increased six-fold from 6.2 per million people in 2010–11 to 38.4 per million in 2019–20.
What are the benefits and harms?
People considering surgery will typically weigh that option against not having surgery. But there has been very little research comparing disc replacement surgery with non-surgical treatments.
Clinical trials are the best way to determine if a treatment is effective. You first want to show that a new treatment is better than doing nothing before you start comparisons with other treatments. For surgical procedures, the next step might be to compare the procedure to non-surgical alternatives.
Unfortunately, these crucial first research steps have largely been skipped for disc replacement surgery for both neck and back pain. As a result, there’s a great deal of uncertainty about the treatment.
There are no clinical trials we know of investigating whether disc replacement is effective for neck pain compared to nothing or compared to non-surgical treatments.
For low back pain, the only clinical trial that has been conducted to our knowledge comparing disc replacement to a non-surgical alternative found disc replacement surgery was slightly more effective than an intensive rehabilitation program after two years and eight years.
Many people experience chronic pain. Yan Krukau/Pexels Complications are not uncommon, and can include disclocation of the artificial disc, fracture (break) of the artificial disc, and infection.
In the clinical trial mentioned above, 26 of the 77 surgical patients had a complication within two years of follow up, including one person who underwent revision surgery that damaged an artery leading to a leg needing to be amputated. Revision surgery means a re-do to the primary surgery if something needs fixing.
Are there effective alternatives?
The first thing to consider is whether you need surgery. Seeking a second opinion may help you feel more informed about your options.
Many surgeons see disc replacement as an alternative to spinal fusion, and this choice is often presented to patients. Indeed, the research evidence used to support disc replacement mainly comes from studies that compare disc replacement to spinal fusion. These studies show people with neck pain may recover and return to work faster after disc replacement compared to spinal fusion and that people with back pain may get slightly better pain relief with disc replacement than with spinal fusion.
However, spinal fusion is similarly not well supported by evidence comparing it to non-surgical alternatives and, like disc replacement, it’s also expensive and associated with considerable risks of harm.
Fortunately for patients, there are new, non-surgical treatments for neck and back pain that evidence is showing are effective – and are far cheaper than surgery. These include treatments that address both physical and psychological factors that contribute to a person’s pain, such as cognitive functional therapy.
While Musk reported a good immediate outcome with disc replacement surgery, given the evidence – or lack thereof – we advise caution when considering this surgery. And if you’re presented with the choice between disc replacement and spinal fusion, you might want to consider a third alternative: not having surgery at all.
Giovanni E Ferreira, NHMRC Emerging Leader Research Fellow, Institute of Musculoskeletal Health, University of Sydney; Christine Lin, Professor, Institute for Musculoskeletal Health, University of Sydney; Christopher Maher, Professor, Sydney School of Public Health, University of Sydney; Ian Harris, Professor of Orthopaedic Surgery, UNSW Sydney, and Joshua Zadro, NHMRC Emerging Leader Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
How To Really Look After Your Joints
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Other Ways To Look After Your Joints
When it comes to joint health, most people have two quick go-to items:
- Stretching
- Supplements like omega-3 and glucosamine sulfate
Stretching, and specifically, mobility exercises, are important! We’ll have to do a main feature on these sometime soon. But for today, we’ll just say: yes, gentle daily stretches go a long way, as does just generally moving more.
And, those supplements are not without their merits. For example:
- Effect of omega-3 on painful symptoms of patients with osteoarthritis of the synovial joints: systematic review and meta-analysis
- Glucosamine sulfate in the treatment of knee osteoarthritis symptoms: a randomized, double-blind, placebo-controlled study using acetaminophen as a side comparator
Of those, glucosamine sulfate may have an extra benefit in now just alleviating the symptoms, but also slowing the progression of degenerative joint conditions (like arthritis of various kinds). This is something it shares with chondroitin sulfate:
Effect of glucosamine or chondroitin sulfate on the osteoarthritis progression: a meta-analysis
An unlikely extra use for the humble cucumber…
As it turns out, cucumber extract beats glucosamine and chondroitin by 200%, at 1/135th of the dose.
You read that right, and it’s not a typo. See for yourself:
Reduce inflammation, have happier joints
Joint pain and joint degeneration in general is certainly not just about inflammation; there is physical wear-and-tear too. But combatting inflammation is important, and turmeric, which we’ve done a main feature on before, is a potent helper in this regard:
See also: Keep Inflammation At Bay
(a whole list of tips for, well, keeping inflammation at bay)
About that wear-and-tear…
Your bones and joints are made of stuff, and that stuff needs to be replaced. As we get older, the body typically gets worse at replacing it in a timely and efficient fashion. We can help it do its job, by giving it more of the stuff it needs.
And what stuff is that?
Well, minerals like calcium and phosphorus are important, but a lot is also protein! Specifically, collagen. We did a main feature on this before, which is good, as it’d take us a lot of space to cover all the benefits here:
We Are Such Stuff As Fish Are Made Of
Short version? People take collagen for their skin, but really, its biggest benefit is for our bones and joints!
Wrap up warmly and… No wait, skip that.
If you have arthritis, you may indeed “feel it in your bones” when the weather changes. But the remedy for that is not to try to fight it, but rather, to strengthen your body’s ability to respond to it.
The answer? Cryotherapy, with ice baths ranking top:
- Effects of an Exercise Program and Cold-Water Immersion Recovery in Patients with Rheumatoid Arthritis (RA): Feasibility Study
- Effectiveness of home-based conventional exercise and cryotherapy on daily living activities in patients with knee osteoarthritis: A randomized controlled clinical trial
- Local Cryotherapy, Comparison of Cold Air and Ice Massage on Pain and Handgrip Strength in Patients with Rheumatoid Arthritis
Note that this can be just localized, so for example if the problem joints are your wrists, a washing-up bowl with water and ice will do just nicely.
Note also that, per that last study, a single session will only alleviate the pain, not the disease itself. For that (per the other studies) more sessions are required.
We did a main feature about cryotherapy a while back, and it explains how and why it works:
A Cold Shower A Day Keeps The Doctor Away?
Take care!
Share This Post
Related Posts
-
Alzheimer’s Causative Factors To Avoid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Best Brains Bar Nun?
This is Dr. David Snowdon. He’s an epidemiologist, and one of the world’s foremost experts on Alzheimer’s disease. He was also, most famously, the lead researcher of what has become known as “The Nun Study”.
We recently reviewed his book about this study:
…which we definitely encourage you to check out, but we’ll do our best to summarize its key points today!
Reassurance up-front: no, you don’t have to become a nun
The Nun Study
In 1991, a large number (678) of nuns were recruited for what was to be (and until now, remains) the largest study of its kind into the impact of a wide variety of factors on aging, and in particular, Alzheimer’s disease.
Why it was so important: because the nuns were all from the same Order, had the same occupation (it’s a teaching Order), with very similar lifestyles, schedules, socioeconomic status, general background, access to healthcare, similar diets, same relationship status (celibate), same sex (female), and many other factors also similar, this meant that most of the confounding variables that confound other studies were already controlled-for here.
Enrollment in the study also required consenting to donating one’s brain for study post-mortem—and of those who have since died, indeed 98% of them have been donated (the other 2%, we presume, may have run into technical administrative issues with the donation process, due to the circumstances of death and/or delays in processing the donation).
How the study was undertaken
We don’t have enough space to describe the entire methodology here, but the gist of it is:
- Genetic testing for relevant genetic factors
- Data gathered about lives so far, including not just medical records but also autobiographies that the nuns wrote when they took their vows (at ages 19–21)
- Extensive ongoing personal interviews about habits, life choices, and attitudes
- Yearly evaluations including memory tests and physical function tests
- Brain donation upon death
What they found
Technically, The Nun Study is still ongoing. Of the original 678 nuns (aged 75–106), three are still alive (based on the latest report, at least).
However, lots of results have already been gained, including…
Genes
A year into the study, in 1992, the “apolipoprotein E” (APOE) gene was established as a likely causative factor in Alzheimer’s disease. This is probably not new to our readers in 2024, but there are interesting things being learned even now, for example:
The Alzheimer’s Gene That Varies By Race & Sex
…but watch out! Because also:
Alzheimer’s Sex Differences May Not Be What They Appear
Words
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Food
While the dietary habits of the nuns were fairly homogenous, those who favored eating more and cooked greens, beans, and tomatoes, lived longer and with healthier brains.
See also: Brain Food? The Eyes Have It!
Other aspects of brain health & mental health
The study also found that nuns who avoided stroke and depression, were also less likely to get dementia.
For tending to these, check out:
- Two Things You Can Do To Improve Stroke Survival Chances
- Depression, And The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
Community & Faith
Obviously, in this matter the nuns were quite a homogenous group, scoring heavily in community and faith. What’s relevant here is the difference between the nuns, and other epidemiological studies in other groups (invariably not scoring so highly).
Community & faith are considered, separately and together, to be protective factors against dementia.
Faith may be something that “you have it or you don’t” (we’re a health science newsletter, not a theological publication, but for the interested, philosopher John Stuart Mill’s 1859 essay “On Liberty“ makes a good argument for it not being something one can choose, prompting him to argue for religious tolerance, on the grounds that religious coercion is a futile effort precisely because a person cannot choose to dis/believe something)
…but community can definitely be chosen, nurtured, and grown. We’ve written about this a bit before:
You might also like to check out this great book on the topic:
Purpose: Design A Community And Change Your Life – by Gina Bianchini
Want more?
We gave a ground-up primer on avoiding Alzheimer’s and other dementias; check it out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Viruses aren’t always harmful. 6 ways they’re used in health care and pest control
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We tend to just think of viruses in terms of their damaging impacts on human health and lives. The 1918 flu pandemic killed around 50 million people. Smallpox claimed 30% of those who caught it, and survivors were often scarred and blinded. More recently, we’re all too familiar with the health and economic impacts of COVID.
But viruses can also be used to benefit human health, agriculture and the environment.
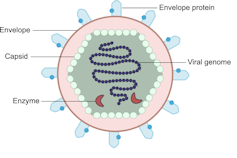
Viruses are comparatively simple in structure, consisting of a piece of genetic material (RNA or DNA) enclosed in a protein coat (the capsid). Some also have an outer envelope.
Viruses get into your cells and use your cell machinery to copy themselves.
Here are six ways we’ve harnessed this for health care and pest control.1. To correct genes
Viruses are used in some gene therapies to correct malfunctioning genes. Genes are DNA sequences that code for a particular protein required for cell function.
If we remove viral genetic material from the capsid (protein coat) we can use the space to transport a “cargo” into cells. These modified viruses are called “viral vectors”.
Viruses consist of a piece of RNA or DNA enclosed in a protein coat called the capsid.
DEXiViral vectors can deliver a functional gene into someone with a genetic disorder whose own gene is not working properly.
Some genetic diseases treated this way include haemophilia, sickle cell disease and beta thalassaemia.
2. Treat cancer
Viral vectors can be used to treat cancer.
Healthy people have p53, a tumour-suppressor gene. About half of cancers are associated with the loss of p53.
Replacing the damaged p53 gene using a viral vector stops the cancerous cell from replicating and tells it to suicide (apoptosis).
Viral vectors can also be used to deliver an inactive drug to a tumour, where it is then activated to kill the tumour cell.
This targeted therapy reduces the side effects otherwise seen with cytotoxic (cell-killing) drugs.
We can also use oncolytic (cancer cell-destroying) viruses to treat some types of cancer.
Tumour cells have often lost their antiviral defences. In the case of melanoma, a modified herpes simplex virus can kill rapidly dividing melanoma cells while largely leaving non-tumour cells alone.
3. Create immune responses
Viral vectors can create a protective immune response to a particular viral antigen.
One COVID vaccine uses a modified chimp adenovirus (adenoviruses cause the common cold in humans) to transport RNA coding for the SARS-CoV-2 spike protein into human cells.
The RNA is then used to make spike protein copies, which stimulate our immune cells to replicate and “remember” the spike protein.
Then, when you are exposed to SARS-CoV-2 for real, your immune system can churn out lots of antibodies and virus-killing cells very quickly to prevent or reduce the severity of infection.
4. Act as vaccines
Viruses can be modified to act directly as vaccines themselves in several ways.
We can weaken a virus (for an attenuated virus vaccine) so it doesn’t cause infection in a healthy host but can still replicate to stimulate the immune response. The chickenpox vaccine works like this.
The Salk vaccine for polio uses a whole virus that has been inactivated (so it can’t cause disease).
Others use a small part of the virus such as a capsid protein to stimulate an immune response (subunit vaccines).
An mRNA vaccine packages up viral RNA for a specific protein that will stimulate an immune response.
5. Kill bacteria
Viruses can – in limited situations in Australia – be used to treat antibiotic-resistant bacterial infections.
Bacteriophages are viruses that kill bacteria. Each type of phage usually infects a particular species of bacteria.
Unlike antibiotics – which often kill “good” bacteria along with the disease-causing ones – phage therapy leaves your normal flora (useful microbes) intact.
Bacteriophages (red) are viruses that kill bacteria (green).
Shutterstock6. Target plant, fungal or animal pests
Viruses can be species-specific (infecting one species only) and even cell-specific (infecting one type of cell only).
This occurs because the proteins viruses use to attach to cells have a shape that binds to a specific type of cell receptor or molecule, like a specific key fits a lock.
The virus can enter the cells of all species with this receptor/molecule. For example, rabies virus can infect all mammals because we share the right receptor, and mammals have other characteristics that allow infection to occur whereas other non-mammal species don’t.
When the receptor is only found on one cell type, then the virus will infect that cell type, which may only be found in one or a limited number of species. Hepatitis B virus successfully infects liver cells primarily in humans and chimps.
We can use that property of specificity to target invasive plant species (reducing the need for chemical herbicides) and pest insects (reducing the need for chemical insecticides). Baculoviruses, for example, are used to control caterpillars.
Similarly, bacteriophages can be used to control bacterial tomato and grapevine diseases.
Other viruses reduce plant damage from fungal pests.
Myxoma virus and calicivirus reduce rabbit populations and their environmental impacts and improve agricultural production.
Just like humans can be protected against by vaccination, plants can be “immunised” against a disease-causing virus by being exposed to a milder version.
Thea van de Mortel, Professor, Nursing, School of Nursing and Midwifery, Griffith University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Reduce Cortisol Levels Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cortisol is a hormone that is important for us (we’d struggle to get up in the morning without it, for a start), but in this modern world we often have too much of it, too much of the time. How can we rebalance it? Dr. Mindy Pelz explains:
Lifestyle adjustments
A note in advance: the video makes frequent reference to things that “spike cortisol levels”, but this is probably intended as a stand-in for “raise cortisol levels”. Because, unlike for some things, in the case of cortisol, spikes aren’t usually a problem (indeed, they can be beneficial, and this is a large part of why cold showers and ice baths can be healthy; it’s an artificially induced cortisol spike, and this hormesis has an assortment of healthy benefits, each related to improving our body’s ability to switch quickly between states as appropriate); rather, it’s chronically high cortisol levels that are the problem. However, the video discusses things that can increase resting cortisol levels, so where she says “spike”, we suggest to read “raise”.
Dr. Pelz, an advocate of intermittent fasting, mentions that done incorrectly and/or for the same way for too long, fasting can raise cortisol levels and thus sabotage our efforts—so varying our fasting style can help avoid that. For example, 16:8, 5:2, longer fasts less frequently, etc.
On the topic of food, she also warns us of the dangers of ultra-processed food, harmful oils, and foods with added sugar, as these can all raise cortisol levels.
When it comes to exercise, she notes that intense exercise without adequate recovery can raise cortisol levels, so again it’s good to mix up one’s methods, vary one’s exercise routine, and allow each well-worked muscle-group adequate rest afterwards.
Dr. Pelz also talks mindset, and has her own interesting way of framing the well-established science that chronic stress means chronically high stress hormone (cortisol) levels; Dr. Pelz prefers to see it as negative vs positive thoughts, environments, etc.
Any discussion of cortisol management would be incomplete without discussing the importance of good quality sleep. Dr. Pelz doesn’t mention this at all in her video, but it’s important to bear in mind too!
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Lower Your Cortisol! (Here’s Why & How)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: