Vaping: A Lot Of Hot Air?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Vaping: A Lot Of Hot Air?
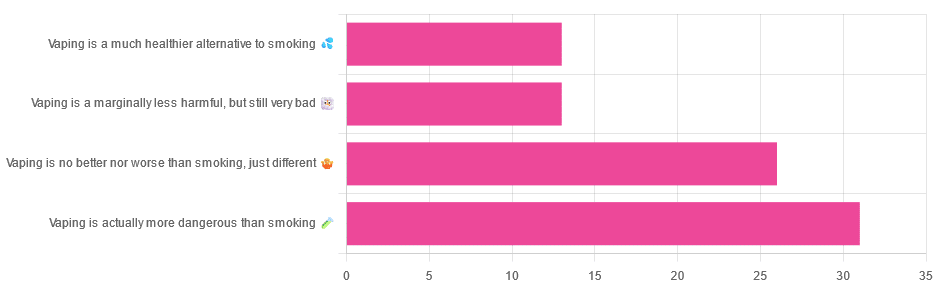
Yesterday, we asked you for your (health-related) opinions on vaping, and got the above-depicted, below-described, set of responses:
- A little over a third of respondents said it’s actually more dangerous than smoking
- A little under a third of respondents said it’s no better nor worse, just different
- A little over 10% of respondents said it’s marginally less harmful, but still very bad
- A little over 10% of respondents said it’s a much healthier alternative to smoking
So what does the science say?
Vaping is basically just steam inhalation, plus the active ingredient of your choice (e.g. nicotine, CBD, THC, etc): True or False?
False! There really are a lot of other chemicals in there.
And “chemicals” per se does not necessarily mean evil green glowing substances that a comicbook villain would market, but there are some unpleasantries in there too:
- Potential harmful health effects of inhaling nicotine-free shisha-pen vapor: a chemical risk assessment of the main components propylene glycol and glycerol
- Inflammatory and Oxidative Responses Induced by Exposure to Commonly Used e-Cigarette Flavoring Chemicals and Flavored e-Liquids without Nicotine
So, the substrate itself can cause irritation, and flavorings (with cinnamaldehyde, the cinnamon flavoring, being one of the worst) can really mess with our body’s inflammatory and oxidative responses.
Vaping can cause “popcorn lung”: True or False?
True and False! Popcorn lung is so-called after it came to attention when workers at a popcorn factory came down with it, due to exposure to diacetyl, a chemical used there.
That chemical was at that time also found in most vapes, but has since been banned in many places, including the US, Canada, the EU and the UK.
Vaping is just as bad as smoking: True or False?
False, per se. In fact, it’s recommended as a means of quitting smoking, by the UK’s famously thrifty NHS, that absolutely does not want people to be sick because that costs money:
Of course, the active ingredients (e.g. nicotine, in the assumed case above) will still be the same, mg for mg, as they are for smoking.
Vaping is causing a health crisis amongst “kids nowadays”: True or False?
True—it just happens to be less serious on a case-by-case basis to the risks of smoking.
However, it is worth noting that the perceived harmlessness of vapes is surely a contributing factor in their widespread use amongst young people—decades after actual smoking (thankfully) went out of fashion.
On the other hand, there’s a flipside to this:
Flavored vape restrictions lead to higher cigarette sales
So, it may indeed be the case of “the lesser of two evils”.
Want to know more?
For a more in-depth science-ful exploration than we have room for here…
BMJ | Impact of vaping on respiratory health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Are You Stuck Playing These Three Roles in Love?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The psychology of Transactional Analysis holds that our interpersonal dynamics can be modelled in the following fashion:
The roles
- Child: vulnerable, trusting, weak, and support-seeking
- Parent: strong, dominant, responsible—but also often exhausted and critical
- Adult: balanced, thoughtful, creative, and kind
Ideally we’d be able to spend most of our time in “Adult” mode, and occasionally go into “Child” or “Parent” mode when required, e.g. child when circumstances have rendered us vulnerable and we need help; parent when we need to go “above and beyond” in the pursuit of looking after others. That’s all well and good and healthy.
However, in relationships, often it happens that partners polarize themselves and/or each other, with one shouldering all of the responsibility, and the other willfully losing their own agency.
The problem lies in that either role can be seductive—on the one hand, it’s nice to be admired and powerful and it’s a good feeling to look after one’s partner; on the other hand, it’s nice to have someone who will meet your every need. What love and trust!
Only, it becomes toxic when these roles stagnate, and each forgets how to step out of them. Each can become resentful of the other (for not pulling their weight, on one side, and for not being able to effortlessly solve all life problems unilaterally and provide endlessly in both time and substance, on the other), digging in to their own side and exacerbating the less healthy qualities.
As to the way out? It’s about self-exploration and mutual honesty—and mutual support:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
While we haven’t (before today) written about TA per se, we have previously written about AT (Attachment Theory), and on this matter, the two can overlap, where certain attachment styles can result in recreating parent/child/adult dynamics:
How To Leverage Attachment Theory In Your Relationship ← this is about understanding and recognizing attachment styles, and then making sure that both you and your partner(s) are armed with the necessary knowledge and understanding to meet each other’s needs.
Take care!
Share This Post
-
Blood-Brain Barrier Breach Blamed For Brain-Fog
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move Over, Leaky Gut. Now It’s A Leaky Brain.
…which is not a headline that promises good news, and indeed, the only good news about this currently is “now we know another thing that’s happening, and thus can work towards a treatment for it”.
Back in February (most popular media outlets did not rush to publish this, as it rather goes against the narrative of “remember when COVID was a thing?” as though the numbers haven’t risen since the state of emergency was declared over), a team of Irish researchers made a discovery:
❝For the first time, we have been able to show that leaky blood vessels in the human brain, in tandem with a hyperactive immune system may be the key drivers of brain fog associated with long covid❞
~ Dr. Matthew Campbell (one of the researchers)
Let’s break that down a little, borrowing some context from the paper itself:
- the leaky blood vessels are breaching the blood-brain-barrier
- that’s a big deal, because that barrier is our only filter between our brain and Things That Definitely Should Not Go In The Brain™
- a hyperactive immune system can also be described as chronic inflammation
- in this case, that includes chronic neuroinflammation which, yes, is also a major driver of dementia
You may be wondering what COVID has to do with this, and well:
- these blood-brain-barrier breaches were very significantly associated (in lay terms: correlated, but correlated is only really used as an absolute in write-ups) with either acute COVID infection, or Long Covid.
- checking this in vitro, exposure of brain endothelial cells to serum from patients with Long Covid induced the same expression of inflammatory markers.
How important is this?
As another researcher (not to mention: professor of neurology and head of the school of medicine at Trinity) put it:
❝The findings will now likely change the landscape of how we understand and treat post-viral neurological conditions.
It also confirms that the neurological symptoms of long covid are measurable with real and demonstrable metabolic and vascular changes in the brain.❞
~ Dr. Colin Doherty (see mini-bio above)
You can read a pop-science article about this here:
Irish researchers discover underlying cause of “brain fog” linked with long covid
…and you can read the paper in full here:
Want to stay safe?
Beyond the obvious “get protected when offered boosters/updates” (see also: The Truth About Vaccines), other good practices include the same things most people were doing when the pandemic was big news, especially avoiding enclosed densely-populated places, washing hands frequently, and looking after your immune system. For that latter, see also:
Beyond Supplements: The Real Immune-Boosters!
Take care!
Share This Post
- the leaky blood vessels are breaching the blood-brain-barrier
-
Pistachios vs Pine Nuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing pistachios to pine nuts, we picked the pistachios.
Why?
First looking at the macros, pistachios have nearly 2x the protein while pine nuts have nearly 2x the fat. The fats are healthy in moderation (mostly polyunsaturated, a fair portion of monounsaturated, and a little saturated), but we’re going to value the protein content higher. Also, pistachios have approximately 2x the carbs, and/but nearly 3x the fiber. All in all, we’ll call this section a moderate win for pistachios.
When it comes to vitamins, pistachios have more of vitamins A, B1, B5, B6, B9, and C, while pine nuts have more of vitamins B2, B3, E, K, and choline. All in all, pistachios are scraping a 6:5 win here, or we could call it a tie if we want to value pine nuts’ vitamins more (due to the difference in how many foods each vitamin is found in, and thus the likelihood of having a deficiency or not).
In the category of minerals, pistachios have more calcium, copper, potassium, and selenium, while pine nuts have more iron, magnesium, manganese, and zinc. This would be a tie if we just call it 4:4, but what’s worth noting is that while both of these nuts are a good source of most of the minerals mentioned, pine nuts aren’t a very good source of calcium or selenium, so we’re going to declare this section a very marginal win for pistachios.
Adding up the moderate win, the scraped win, and the barely scraped win, all adds up to a win for pistachios. However, as you might have noticed, both are great so do enjoy both if you can!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Share This Post
Related Posts
-
PTSD, But, Well…. Complex.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PTSD is typically associated with military veterans, for example, or sexual assault survivors. There was a clear, indisputable, Bad Thing™ that was experienced, and it left a psychological scar. When something happens to remind us of that—say, there are fireworks, or somebody touches us a certain way—it’ll trigger an immediate strong response of some kind.
These days the word “triggered” has been popularly misappropriated to mean any adverse emotional reaction, often to something trivial.
But, not all trauma is so clear. If PTSD refers to the result of that one time you were smashed with a sledgehammer, C-PTSD (Complex PTSD) refers to the result of having been hit with a rolled-up newspaper every few days for fifteen years, say.
This might have been…
- childhood emotional neglect
- a parent with a hair-trigger temper
- bullying at school
- extended financial hardship as a young adult
- “just” being told or shown all too often that your best was never good enough
- the persistent threat (real or imagined) of doom of some kind
- the often-reinforced idea that you might lose everything at any moment
If you’re reading this list and thinking “that’s just life though”, you might be in the estimated 1 in 5 people with (often undiagnosed) C-PTSD.
How About You? Take The (5mins) Test Here
Now, we at 10almonds are not doctors or therapists and even if we were, we certainly wouldn’t try to diagnose from afar. But, even if there’s only a partial match, sometimes the same advice can help.
So what are the symptoms of C-PTSD?
- A feeling that nothing is safe; we might suddenly lose what we have gained
- The body keeps the score… And it shows. We may have trouble relaxing, an aversion to exercise for reasons that don’t really add up, or an aversion to being touched.
- Trouble sleeping, born of nagging sense that to sleep is to be vulnerable to attack, and/or lazy, and/or negligent of our duties
- Poor self-image, about our body and/or about ourself as a person.
- We’re often drawn to highly unavailable people—or we are the highly unavailable person to which our complementary C-PTSD sufferers are attracted.
- We are prone to feelings of rage. Whether we keep a calm lid on it or lose our temper, we know it’s there. We’re angry at the world and at ourselves.
- We are not quick to trust—we may go through the motions of showing trust, but we’re already half-expecting that trust to have been misplaced.
- “Hell is other people” has become such a rule of life that we may tend to cloister ourselves away from company.
- We may try to order our environment around us as a matter of safety, and be easily perturbed by sudden changes being imposed on us, even if ostensibly quite minor or harmless.
- In a bid to try to find safety, we may throw ourselves into work—whatever that is for us. It could be literally our job, or passion projects, or our family, or community, and in and of itself that’s great! But the motivation is more of an attempt to distract ourselves from The Horrors™.
“Alright, I scored more of those than I care to admit. What now?”
A lot of the answer lies in first acknowledging to yourself what happened, to make you feel the way you do now. If you, for example, have an abject hatred of Christmas, what were your childhood Christmases like? If you fear losing money that you’ve accumulated, what underpins that fear? It could be something that directly happened to you, but it also could just be repeated messages you received from your parents, for example.
It could even be that you had superficially an idyllic perfect childhood. Health, wealth, security, a loving family… and simply a chemical imbalance in your brain made it a special kind of Hell for you that nobody understood, and perhaps you didn’t either.
Unfortunately, a difficult task now lies ahead: giving love, understanding, compassion, and reassurance to the person for whom you may have the most contempt in the world: yourself.
If you’d like some help with that, here are some resources:
ComplexTrauma.org (a lot of very good free resources, with no need for interaction)
CPTSD Foundation (mostly paid courses and the like)
Some final words about healing…
- You are in fact amazing,
- You can do it, and
- You deserve it.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No, beetroot isn’t vegetable Viagra. But here’s what else it can do
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Beetroot has been in the news for all the wrong reasons. Supply issues in recent months have seen a shortage of tinned beetroot on Australian supermarket shelves. At one point, a tin was reportedly selling on eBay for more than A$65.
But as supplies increase, we turn our attention to beetroot’s apparent health benefits.
Is beetroot really vegetable Viagra, as UK TV doctor Michael Mosley suggests? What about beetroot’s other apparent health benefits – from reducing your blood pressure to improving your daily workout? Here’s what the science says.
What’s so special about beetroot?
Beetroot – alongside foods such as berries, nuts and leafy greens – is a “superfood”. It contains above-average levels per gram of certain vitamins and minerals.
Beetroot is particularly rich in vitamin B and C, minerals, fibre and antioxidants.
Most cooking methods don’t significantly alter its antioxidant levels. Pressure cooking does, however, lower levels of carotenoid (a type of antioxidant) compared to raw beetroot.
Processing into capsules, powders, chips or juice may affect beetroot’s ability to act as an antioxidant. However, this can vary between products, including between different brands of beetroot juice.
Is beetroot really vegetable Viagra?
The Romans are said to have used beetroot and its juice as an aphrodisiac.
But there’s limited scientific evidence to say beetroot improves your sex life. This does not mean it doesn’t. Rather, the vast number of scientific studies looking at the effect of beetroot have not measured libido or other aspects of sexual health.
How could it work?
When we eat beetroot, chemical reactions involving bacteria and enzymes transform the nitrate in beetroot into nitrite, then to nitric oxide. Nitric oxide helps dilate (widen) blood vessels, potentially improving circulation.
The richest sources of dietary nitric oxide that have been tested in clinical studies are beetroot, rocket and spinach.
Nitric oxide is also thought to support testosterone in its role in controlling blood flow before and during sex in men.
Beetroot’s ability to improve blood flow can benefit the circulatory system of the heart and blood vessels. This may positively impact sexual function, theoretically in men and women.
Therefore, it is reasonable to suggest there could be a modest link between beetroot and preparedness for sex, but don’t expect it to transform your sex life.
What else could it do?
Beetroot has received increasing attention over recent years due to its antioxidant and anti-tumour effect in humans.
Clinical trials have not verified all beetroot’s active ingredients and their effects. However, beetroot may be a potentially helpful treatment for various health issues related to oxidative stress and inflammation, such as cancer and diabetes. The idea is that you can take beetroot supplements or eat extra beetroot alongside your regular medicines (rather than replace them).
There is evidence beetroot juice can help lower systolic blood pressure (the first number in your blood pressure reading) by 2.73-4.81 mmHg (millimetres of mercury, the standard unit of measuring blood pressure) in people with high blood pressure. Some researchers say this reduction is comparable to the effects seen with certain medications and dietary interventions.
Other research finds even people without high blood pressure (but at risk of it) could benefit.
Beetroot may also improve athletic performance. Some studies show small benefits for endurance athletes (who run, swim or cycle long distances). These studies looked at various forms of the food, such as beetroot juice as well as beetroot-based supplements.
How to get more beetroot in your diet
There is scientific evidence to support positive impacts of consuming beetroot in whole, juice and supplement forms. So even if you can’t get hold of tinned beetroot, there are plenty of other ways you can get more beetroot into your diet. You can try:
- raw beetroot – grate raw beetroot and add it to salads or coleslaw, or slice beetroot to use as a crunchy topping for sandwiches or wraps
- cooked beetroot – roast beetroot with olive oil, salt and pepper for a flavour packed side dish. Alternatively, steam beetroot and serve it as a standalone dish or mixed into other dishes
- beetroot juice – make fresh beetroot juice using a juicer. You can combine it with other fruits and vegetables for added flavour. You can also blend raw or cooked beetroot with water and strain to make a juice
- smoothies – add beetroot to your favourite smoothie. It pairs well with fruits such as berries, apples and oranges
- soups – use beetroot in soups for both flavour and colour. Borscht is a classic beetroot soup, but you can also experiment with other recipes
- pickled beetroot – make pickled beetroot at home, or buy it from the supermarket. This can be a tasty addition to salads or sandwiches
- beetroot hummus – blend cooked beetroot into your homemade hummus for a vibrant and nutritious dip. You can also buy beetroot hummus from the supermarket
- grilled beetroot – slice beetroot and grill it for a smoky flavour
- beetroot chips – slice raw beetroot thinly, toss the slices with olive oil and your favourite seasonings, then bake or dehydrate them to make crispy beetroot chips
- cakes and baked goods – add grated beetroot to muffins, cakes, or brownies for a moist and colourful twist.
You can add beetroot to baked goods. Ekaterina Khoroshilova/Shutterstock Are there any downsides?
Compared to the large number of studies on the beneficial effects of beetroot, there is very little evidence of negative side effects.
If you eat large amounts of beetroot, your urine may turn red or purple (called beeturia). But this is generally harmless.
There have been reports in some countries of beetroot-based dietary supplements contaminated with harmful substances, yet we have not seen this reported in Australia.
What’s the take-home message?
Beetroot may give some modest boost to sex for men and women, likely by helping your circulation. But it’s unlikely to transform your sex life or act as vegetable Viagra. We know there are many contributing factors to sexual wellbeing. Diet is only one.
For individually tailored support talk to your GP or an accredited practising dietitian.
Lauren Ball, Professor of Community Health and Wellbeing, The University of Queensland and Emily Burch, Lecturer, Southern Cross University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Infections Here, Infections There…
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This week in health news, let’s take a look at infections outside and in, and how to walk away from it all (in a good way):
The bird that flu away
This one cannot be described as good news. Basically, bird flu is now already epidemic amongst cows in the US, with 845 herds (not 845 cows; 845 herds) testing positive across 16 states. The US Department of Agriculture earlier this month announced a federal order to test milk nationwide. Researchers welcomed the news, but said it should have happened months ago—before the virus was so entrenched. It currently has a fatality rate of 2–5% in cows; we don’t have enough data to reasonably talk about its fatality rate in humans—yet.
❝It’s disheartening to see so many of the same failures that emerged during the COVID-19 crisis re-emerge❞
~ Tom Bollyky, director of the Global Health Program at the Council on Foreign Relations
Read in full: How America lost control of the bird flu, setting the stage for another pandemic
Related: Cows’ Milk, Bird Flu, & You
Alzheimer’s from the gut upwards
Alzheimer’s is generally thought of as being a purely brain thing, but there’s a link between a [specific] chronic gut infection, and the development of Alzheimer’s disease. This infection is called human cytomegalovirus, or HCMV for short, and usually we’ve all been exposed to it by young adulthood. However, for some people, it lingers in an active state in the gut, wherefrom it may travel to the brain via the vagus nerve “gut-brain highway”. And once there, well, you can guess the rest:
Read in full: The surprising role of gut infection in Alzheimer’s disease
Related: How To Reduce Your Alzheimer’s Risk
Walking back to happiness
Analyzing data from 96,138 adults around the world, showed that more steps meant less depression for participants.
You may be thinking “well yes, depressed people walk less”, but more specifically, increases in activity showed increases in anti-depressive benefits, with even small incremental increases showing correspondingly incremental benefits. Specifically, each additional 1,000 steps per day corresponded to a 9% reduction in depression:
Read in full: Higher daily step counts associated with fewer depressive symptoms
Related: Walking… Better.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: