Vaginal Probiotics: What Does The Science Say?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Is there any merit to vaginal probiotics?❞
What a fun question! First let’s break it down, as this could mean two different things:
- Probiotics, which you consume, using your mouth, which are marketed as benefiting vaginal health
- Probiotics taken as a vaginal pessary/suppository, to act directly there
The former has limited evidence for it, but generally speaking, improving one’s gut health improves all other areas of health, so it’s not surprising if it helps this too.
See for example:
Some notes:
- candidal vaginitis means a yeast infection causing vaginal inflammation
- bacterial vaginosis means a vaginal bacterial imbalance (generally also featuring vaginal inflammation, though it can be asymptomatic)
In the latter case, the “imbalance” in question is usually a shortage of Lactobacillus sp. (that is to say, the diverse species of the Lactobacillus genus) resulting in an overgrowth of other kinds of bacteria, which in turn results in changing the vaginal microbiome to make it warmer and more acidic than it should be.
While a healthy vagina shouldn’t smell of roses, it shouldn’t smell fishy either; if it does, that’s a sign of bacterial vaginosis.
What it’s supposed to be like: slightly bitter, slightly salty, distinctly umami, along with a cocktail of personal pheromones (and if menstruating or otherwise* vaginally bleeding, then of course add: iron/”metallic”). The pheromones will also reflect any hormonal changes, but should never make anything smell bad, just different.
*e.g. due to PCOS, fibroids, etc. Note that in the case of PCOS, it may also smell a little different (if it does, then usually: a little more musky), due to often different hormone levels. Again: it still shouldn’t smell bad, though, just different.
In the above-linked study, taking more live Lactobacillus acidophilus (in yogurt, eating it, with their mouths) improved levels of L. acidophilus in the vagina. While the study authors concluded “this ingestion of yogurt may have reduced episodes of bacterial vaginosis”, which is rather a weak claim, it can be argued that it merely improving the levels of L. acidophilus in the vagina was already a win.
That was a small (n=42, and only 7 followed through to completion) and old (1996) study, and it bears mentioning that most of the studies into this seem to be small and old, but conclude similarly with weakly positive statements.
However, it does make a difference what kind of Lactobacillus is used, for example in this next study…
- L. fermentum RC-14 worked well (90% success rate)
- L. rhamnosus GR-1 worked somewhat (40% success rate)
- L. rhamnosus GG did not work (0% success rate)
So, diversity is key, and getting a wide range of Lactobacillus sp. seems to be a safe bet.
Short version: enjoying probiotics as part of your diet probably improves vaginal health, just like it improves pretty much everything else.
See also: Make Friends With Your Gut (You Can Thank Us Later)
You would think that this would mean that taking probiotics as a vaginal pessary/suppository would be even better, but the results are weaker, as in this study, which produced temporary improvements in about half the study group, with only 3 out of 28 being free of bacterial vaginosis the next month:
Treatment of bacterial vaginosis with lactobacilli
This study got better results, with a 61% success rate:
Important note
Do note that this last category, involving topical treatments (i.e., manually introducing Lactobacillus sp. to the vagina) were all in cases of pre-existing bacterial vaginosis, not as a prophylactic and/or general health-improving thing.
If your vagina seems happy right now, then do not mess with its happy bacterial balance!
And at all times (regardless of whether it seems happy right now or not): do not douche (it does not need it and will not benefit from it; the vagina is self-cleaning*) as this will wash out many of your Lactobacilli and will do absolutely nothing against any Candida there (C. albicans being a rooted fungus, whereas Lactobacillus is a sausage-shaped bacterium with many tiny appendages but no actual ability to stay put), so Candida will flourish in the Lactobacillus’s absence.
*by the vagina, we are referring to the vaginal canal. The vulva—the outside part consisting of the two pairs of labia, the glans clitoris, and clitoral hood—are not self-cleaning, and should just be washed gently per your normal bath/shower routine; that’s perfectly fine and good.
And definitely don’t put any “cleansing” toiletries inside the vagina (or any toiletries at all, for that matter), even if they are sold and marketed for that purpose; they will not help and they will harm.
Also, due to their neighborliness, messing up the microbiome inside the vagina is a common way to also get Candida inside the urethra:
How To Avoid Urinary Tract Infections (UTIs)
One other option
Finally, unless you have a “very good friend” you have a pressing urge to swap germs with, you might want to leave this one to the scientists, but we share this paper just for interest:
Lastly…
Going back to oral supplementation, if you’d like to try that then check out this for further notes on what, why, how, etc:
How Much Difference Do Probiotic Supplements Make To Health?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Plant-Based Diet Revolution – by Dr. Alan Desomond
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Is this just another gut-healthy cooking guide? Not entirely…
For a start, it’s not just about giving you a healthy gut; it also covers a healthy heart and a healthy brain. There’s lots of science in here!
It’s also aimed as a transitional guide to eating more plants and fewer animal products, if you so choose. And if you don’t so choose, at least having the flexibility to cook both ways.
The recipes themselves (organized into basics, breakfasts, lunches, mains, desserts) are clear and easy while also being calculated to please readers (and their families) who are used to eating more meat. There are, for instance, plenty of healthy proteins, healthy fats, and comfort foods.
The “28 days” of the title refers to a meal plan using the recipes from the book; it’s not a big feature of the book though, so use it or don’t, but the cooking advice itself is more than worth the price of the book and the recipes are certainly great.
Bottom line: if you’re thinking of taking a “Meatless Mondays” approach to making your diet healthier, this book can help you do that in style!
Click here to check out The Plant-Based Diet Revolution, and upgrade your culinary repertoire!
Share This Post
-
Tomatoes vs Carrots – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tomatoes to carrots, we picked the carrots.
Why?
Both known for being vitamin-A heavyweights, there is nevertheless a clear winner:
In terms of macros, carrots have a little over 2x the carbs, and/but also a little over 2x the fiber, so we consider category this a win for carrots.
In the category of vitamins, tomatoes have more vitamin C, while carrots have more of vitamins A, B1, B2, B3, B5, B6, B9, E, K, and choline. And about that vitamin A specifically: carrots have over 20x the vitamin A of tomatoes. An easy win for carrots here!
When it comes to minerals, tomatoes have a little more copper, while carrots have more calcium, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. Another clear win for carrots.
Looking at polyphenols, carrots are good but tomatoes have more, including a good healthy dose of quercetin; they also have more lycopene, not technically a polyphenol by virtue of its chemical structure (it’s a carotenoid), but a powerful phytochemical nonetheless (and much more prevalent in sun-dried tomatoes, in any case, which is not what we were looking at today—perhaps another day we’ll do sun-dried tomatoes and carrots head-to-head!).
Still, a) carrots are not short of carotenoids either (including lycopene), and b) we don’t think the moderate win on polyphenols is enough to outdo carrots having won all the other categories.
All in all, carrots win the day, but of course, do enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Lycopene’s Benefits For The Gut, Heart, Brain, & More
Enjoy!
Share This Post
-
How To Actually Get Abs (10 Annoying Tips That Work!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cori Lefkowitz, of “Strong At Any Age”, advises…
The method
It may not be fun, but here’s what she finds works:
- Be boring: stick to a simple, repetitive diet to track progress easily, and make hitting macros simpler.
- Cut back on protein bars: processed protein bars are calorie-dense but not filling (due to their small volume), so limit them, especially when trying to get lean.
- Stop daily fluctuations: she advises to be precise with macros and calories daily, not just weekly, to see consistent results.
- Focus on fiber: aim for 25–30g of fiber daily to improve gut health, reduce cravings, and maintain health while cutting fat.
- Get 30–40g of protein per meal: ensure each meal has enough protein to fuel muscle growth and support overall body function.
- Prioritize carbs around workouts: eat carbs before and after training to fuel performance, aid muscle repair, and maintain lean mass.
- Take diet breaks: incorporate 1–2 week maintenance phases to prevent metabolic adaptation, maintain muscle, and thus stay consistent in the long-term.
- Be careful with fat burners & preworkout: these can harm sleep, recovery, and long-term fat loss; opt for natural dietary energy sources instead.
- Don’t set-and-forget: regularly assess and adjust your diet and macros as your body and lifestyle change.
- “Suck it up, buttercup”: fat loss requires persistence, discipline, and pushing through tough moments when you feel like quitting.
For more on all of this, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
Is A Visible Six-Pack Obtainable Regardless Of Genetic Predisposition?
Take care!
Share This Post
Related Posts
-
Kidney Beans or Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing kidney beans to black beans, we picked the black beans.
Why?
First, do note that black beans are also known as turtle beans, or if one wants to hedge one’s bets, black turtle beans. It’s all the same bean. As a small linguistic note, kidney beans are known as “red beans” in many languages, so we could have called this “red beans vs black beans”, but that wouldn’t have landed so well with our largely anglophone readership. So, kidney beans vs black beans it is!
They’re certainly both great, and this is a close one today…
In terms of macros, they’re equal on protein and black beans have more carbs and/but also more fiber. So far, so equal—or rather, if one pulls ahead of the other here, it’s a matter of subjective priorities.
In the category of vitamins, they’re equal on vitamins B2, B3, and choline, while kidney beans have more of vitamins B6, B9, C, and K, and black beans have more of vitamins A, B1, B5, and E. In other words, the two beans are still tied with a 4:4 split, unless we want to take into account that that vitamin E difference is that black beans have 29x more vitamin E, in which case, black beans move ahead.
When it comes to minerals, finally the winner becomes apparent; while kidney beans have a little more manganese and zinc, on the other hand black beans have more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium. However, it should be noted that honestly, the margins aren’t huge here and kidney beans are almost as good for all of these minerals.
In short, black beans win the day, but kidney beans are very close behind, so enjoy whichever you prefer, or better yet, both! They go great together in tacos, burritos, or similar, by the way.
Want to learn more?
You might like to read:
- Kidney Beans vs Fava Beans – Which is Healthier?
- Chickpeas vs Black Beans – Which is Healthier?
- Bold Beans – by Amelia Christie-Miller ← this is a recipe book; if you’re looking to incorporate more beans into your diet and want to make it good, this cookbook can lead the way!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The 5 Resets – by Dr. Aditi Nerurkar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What this book isn’t: an advice to go on a relaxing meditation retreat, or something like that.
What this is: a science-based guide to what actually works.
There’s no need to be mysterious, so we’ll mention that the titular “5 resets” are:
- What matters most
- Quiet in a noisy world
- Leveraging the brain-body connection
- Coming up for air (regaining perspective)
- Bringing your best self forward
All of these are things we can easily lose sight of in the hustle and bustle of daily life, so having a system for keeping them on track can make a huge difference!
The style is personable and accessible, while providing a lot of strongly science-backed tips and tricks along the way.
Bottom line: if life gets away from you a little too often for comfort, this book can help you keep on top of things with a lot less stress.
Click here to check out “The 5 Resets”, and take control with conscious calm!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
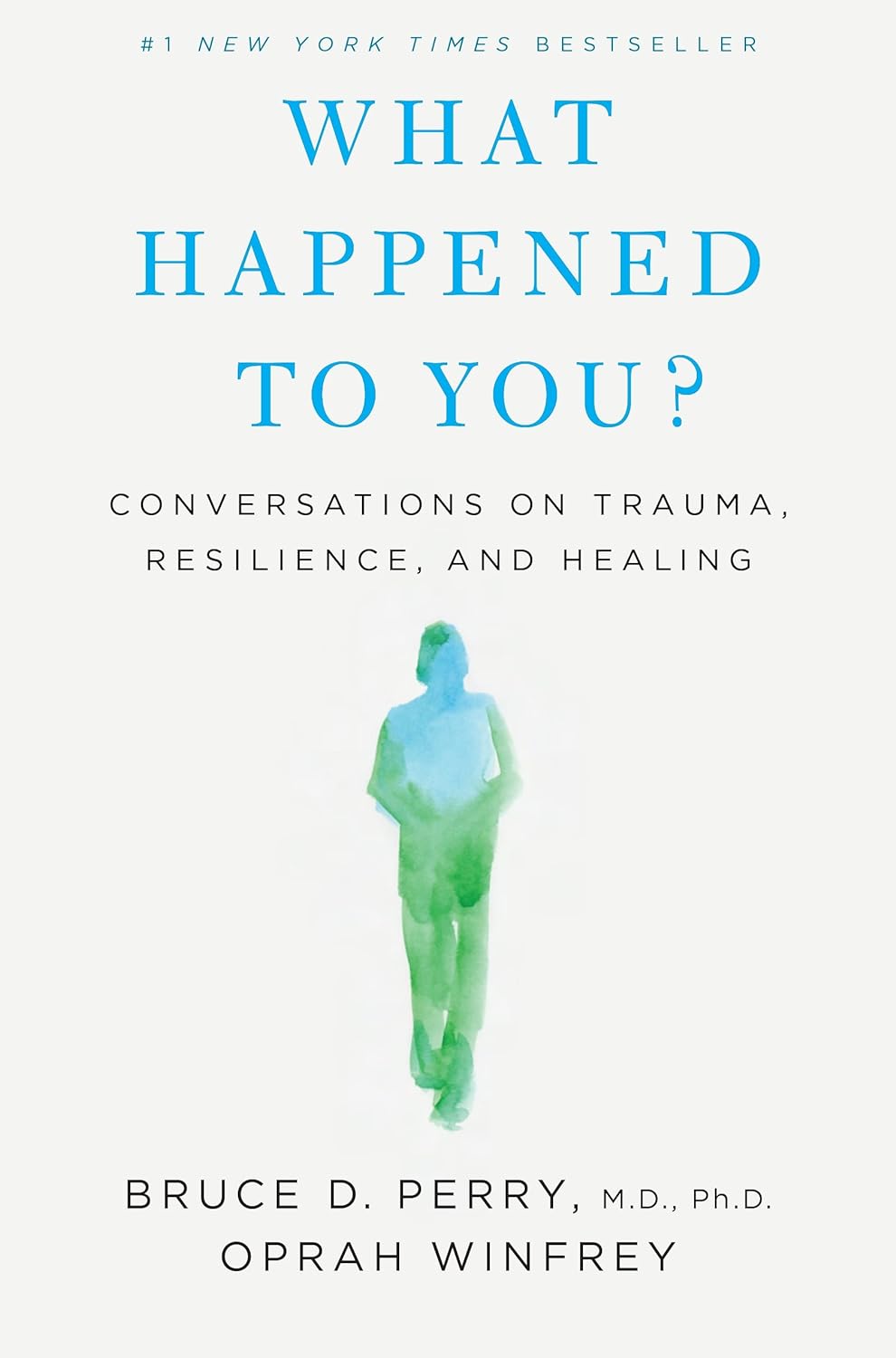
What Happened to You? – by Dr. Bruce Perry and Oprah Winfrey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The very title “What Happened To You?” starts with an assumption that the reader has suffered trauma. This is not just a sample bias of “a person who picks up a book about healing from trauma has probably suffered trauma”, but is also a statistically safe assumption. Around 60% of adults report having suffered some kind of serious trauma.
The authors examine, as the subtitle suggests, these matters in three parts:
- Trauma
- Resilience
- Healing
Trauma can take many forms; sometimes it is a very obvious dramatic traumatic event; sometimes less so. Sometimes it can be a mountain of small things that eroded our strength leaving us broken. But what then, of resilience?
Resilience (in psychology, anyway) is not imperviousness; it is the ability to suffer and recover from things.
Healing is the tail-end part of that. When we have undergone trauma, displayed whatever amount of resilience we could at the time, and now have outgrown our coping strategies and looking to genuinely heal.
The authors present many personal stories and case studies to illustrate different kinds of trauma and resilience, and then go on to outline what we can do to grow from there.
Bottom line: if you or a loved one has suffered trauma, this book may help a lot in understanding and processing that, and finding a way forwards from it.
Click here to check out “What Happened To You?” and give yourself what you deserve.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: