Undo The Sun’s Damage To Your Skin
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s often said that our skin is our largest organ. Our brain or liver are the largest solid organs by mass (which one comes out on top will vary from person to person), our gut is the longest, and our lungs are the largest by surface area. But our skin is large, noticeable, and has a big impact on the rest of our health.
The sun is one of the main damaging factors for our skin; assorted toxins are also a major threat for many people, and once the skin barrier gets broken, it’s a field-day for bacteria.
So, what can we do about it?
Tretinoin: the skin’s rejuvenator
Tretinoin is also called retinoic acid, not to be mistaken for retinol, although they are both retinoids. Tretinoin is much stronger.
As for what it’s stronger at:
It’s usually prescribed for the treatment of sun-damage, acne, and wrinkles. Paradoxically, it works by inflaming the skin (and then making it better, and having done so, keeping it better).
In few words: it encourages your skin to speed up its life cycle, which means that cells die and are replaced sooner, which means the average age of skin cells will be considerably younger at any given time.
This is the same principle as we see at work when it comes to cellular apoptosis and autophagy in general, and specifically the same idea as we discussed when talking about senolytics, compounds that kill aging cells:
Fisetin: The Anti-Aging Assassin
About that paradoxical inflammation…
❝The topical use of tretinoin as an antiacne agent began almost a half century ago. Since that time it has been successfully used to treat comedonal and inflammatory acne.
Over the intervening years, the beneficial effects of tretinoin have grown from an understanding of its potent cornedolytie-related properties to an evolving appreciation of its antiinflammatory actions.
…
The topical use of clindamycin and tretinoin as a combination treatment modality that includes antibacterial, comedolytic, and antiinflammatoiy properties has proven to be a very effective therapy for treating the various stages of acne
…
It is now becoming increasingly clear that there may be good reasons for these observations.❞
~ Drs. Schmidt & Gans, lightly edited here for brevity
Read in full: Tretinoin: A Review of Its Anti-inflammatory Properties in the Treatment of Acne
Against damage by the sun
The older we get, the more likely sun damage is a problem than acne. And in the case of tretinoin,
❝In several well-controlled clinical trials, the proportion of patients showing improvement was significantly higher with 0.01 or 0.05% tretinoin cream than with placebo for criteria such as global assessment, fine and coarse wrinkling, pigmentation and roughness.
Improvements in the overall severity of photodamage were also significantly greater with tretinoin than with placebo.
…
Several placebo-controlled clinical studies have demonstrated that topical tretinoin has significant efficacy in the treatment of photodamaged skin. Improvements in subjective global assessment scores were recorded in:
49–100% of patients using once-daily 0.01% tretinoin,
68–100% of patients using 0.05% tretinoin, and
0–44% of patients using placebo.❞
~ Drs. Wagstaff & Noble
…which is quite compelling.
Read in full: Tretinoin: A Review of its Pharmacological Properties and Clinical Efficacy in the Topical Treatment of Photodamaged Skin
This is very well-established by now; here’s an old paper from when the mechanism of action was unknown (here in the current day, 17 mechanisms of action have been identified; beyond the scope of this article as we only have so much room, but it’s nice to see science building on science):
❝Tretinoin cream has been used extensively to reverse the changes of photoaging. It is the first topical therapy to undergo controlled clinical testing and proved to be efficacious. These results have been substantiated with photography, histopathologie examination, and skin surface replicas.
…
Tretinoin cream has an excellent safety record; a local cutaneous hypervitaminosis A reaction is the only common problem.❞
~ Dr. Goldfarb et al.
Read in full: Topical tretinoin therapy: Its use in photoaged skin
Is it safe?
For most people, when used as directed*, yes. However, it’s likely to irritate your skin at first, and that’s normal. If this persists more than a few weeks, or seems unduly severe, then you might want to stop and talk to your doctor again.
*See also: Scarring following inappropriate use of 0.05% tretinoin gel
(in the case of a young woman who used it 4x daily instead of 1x daily)
Want to try some?
Tretinoin is prescription-only, so speak with your doctor/pharmacist about that. Alternatively, retinal (not retinol) is the strongest natural alternative that works on the same principles; here’s an example product on Amazon 😎
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Walnuts vs Pecans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing walnuts to pecans, we picked the walnuts.
Why?
It was very close, though, and an argument could be made for pecans! Walnuts are nevertheless always a very good bet, and so far in our This-or-That comparisons, the only nut to beat them so far as been almonds, and that was very close too.
In terms of macros, walnuts have a lot more protein, while pecans have a little more fiber (for approximately the same carbs). Both are equally fatty (near enough; technically pecans have a little more) but where the walnuts stand out in the fat category is that while pecans have mostly healthy monounsaturated fats, walnuts have mostly healthy polyunsaturated fats, including including a good balance of omega-3 and omega-6 fatty acids. So, while we do love the extra fiber from pecans, we’re calling it for walnuts in the macros category, on account of the extra protein and the best lipids profile (not that pecans’ lipids profile is bad by any stretch; just, walnuts have it better).
In the vitamins category, walnuts have more of vitamins B2, B6, B9, and C, while pecans offer more of vitamins A, B1, B3, B5, E, K, and choline. The margins aren’t huge and walnuts are also excellent for all the vitamins that pecans narrowly beat them on, but still, the vitamins category is a win for pecans.
When it comes to minerals, walnuts take back the crown; walnuts offer more calcium, copper, iron, magnesium, phosphorus, potassium, and selenium, while pecans have a little more manganese and zinc. Once again, the margins aren’t huge and pecans are also excellent for all the minerals that walnuts narrowly beat them on, but still, the minerals category is a win for walnuts.
In short: enjoy both of these nuts for their healthy fats, vitamins, minerals, protein, and fiber, but if you’re going to pick one, walnuts come out on top.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Take care!
Share This Post
-
Behaving During the Holidays
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝It’s hard to “behave” when it comes to holiday indulging…I’m on a low sodium, sugar restricted regimen from my doctor. Trying to get interested in bell peppers as a snack…wish me luck!❞
Good luck! Other low sodium, low sugar snacks include:
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
- Mixed nuts are an especially healthy way to snack, though (assuming you don’t have an allergy, obviously)
- Air-popped popcorn (you can season it, just not with salt/sugar!)
- Fruit (but not fruit juice; it has to be in solid form)
- Peas (not a classic snack food, we know, but they can be enjoyed many ways)
- Seriously, try them frozen or raw! Frozen/raw peas are a great sweet snack.
- Chickpeas are great dried/roasted, by the way, and give much of the same pleasure as a salty snack without being salty! Obviously, this means cooking them without salt, but that’s fine, or if using tinned, choose “in water” rather than “in brine”
- Hummus is also a great healthy snack (check the ingredients for salt if not making it yourself, though) and can be enjoyed as a dip using raw vegetables (celery, carrot sticks, cruciferous vegetables, whatever you prefer)
Enjoy!
Share This Post
- Nuts! Unsalted, of course. We’re biased towards almonds 😉
-
Passion Fruit vs Blueberries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing passion fruit to blueberries, we picked the passion fruit.
Why?
It wasn’t close!
In terms of macros, the passion fruit has 3x the protein, 1.5x the carbs, and more than 4x the fiber. An easy win for passion fruit!
In the category of vitamins, passion fruit has more of vitamins A, B2, B3, B5, B6, B7, B9, C, and choline, while blueberries have more of vitamins B1, E, and K. So, blueberries are not without their merits, but all in all, another win for passion fruit here.
When it comes to minerals, passion fruit has more calcium, copper, iron, magnesium, manganese, phosphorus, potassium, and selenium, while blueberries have slightly more zinc.
Looking at polyphenols, this is one category where blueberry wins, and by a fair margin. We think that’s a great reason to enjoy blueberries, but not enough to reverse the win for passion fruit based on all the other categories!
Want to learn more?
You might like to read:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
Related Posts
-
The Metabolism Reset Diet – by Alan Christianson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The liver is an incredible organ that does a very important job, but what’s not generally talked about is how we can help it… Beyond the obvious “try to not poison it too much with alcohol, tobacco, etc”. But what can we do that’s actually positive for it?
That’s what Alan Christianson offers in this book.
Now, usually when someone speaks of a “four week cleanse” as this book advertises on its front cover, it’s a lot of bunk. The liver cleanses itself, and the liver and kidneys between them (along with some other organs and processes) detoxify your body for you. No amount of celery juice will do that. However, this book does better than that:
What it’s about, is not really about trying to do a “detox” at all, so much as supporting your liver function by:
- Giving your liver what it needs to regenerate (mostly: protein)
- Not over-taxing your liver while it does so
The liver is a self-regenerating organ (the mythological story of Prometheus aside, here in real life it can regenerate up to 80% of itself, given the opportunity), so whatever the current state of your liver, it’s probably not too late to fix it.
Maybe you’ve been drinking a little too much, or maybe you’ve been taking some meds that have hobbled it a bit (some medications strain the liver rather), or maybe your diet hasn’t been great. Christianson invites you to draw a line under that, and move forwards:
The book gives an overview of the science involved, and explains about the liver’s role in metabolism (hence the promised weight loss benefits) and our dietary habits’ impact on liver function. This is about what we eat, and also about when we eat it, and how and when our body metabolizes that.
Christianson also provides meal ideas and recipes. If we’re honest (and we always are), the science/principles part of the book are worth a lot more than the meal-plan part of the book, though.
In short: a great book for understanding how the liver works and how we can help it do its job effectively.
Click here to check out “The Metabolism Reset Diet” on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
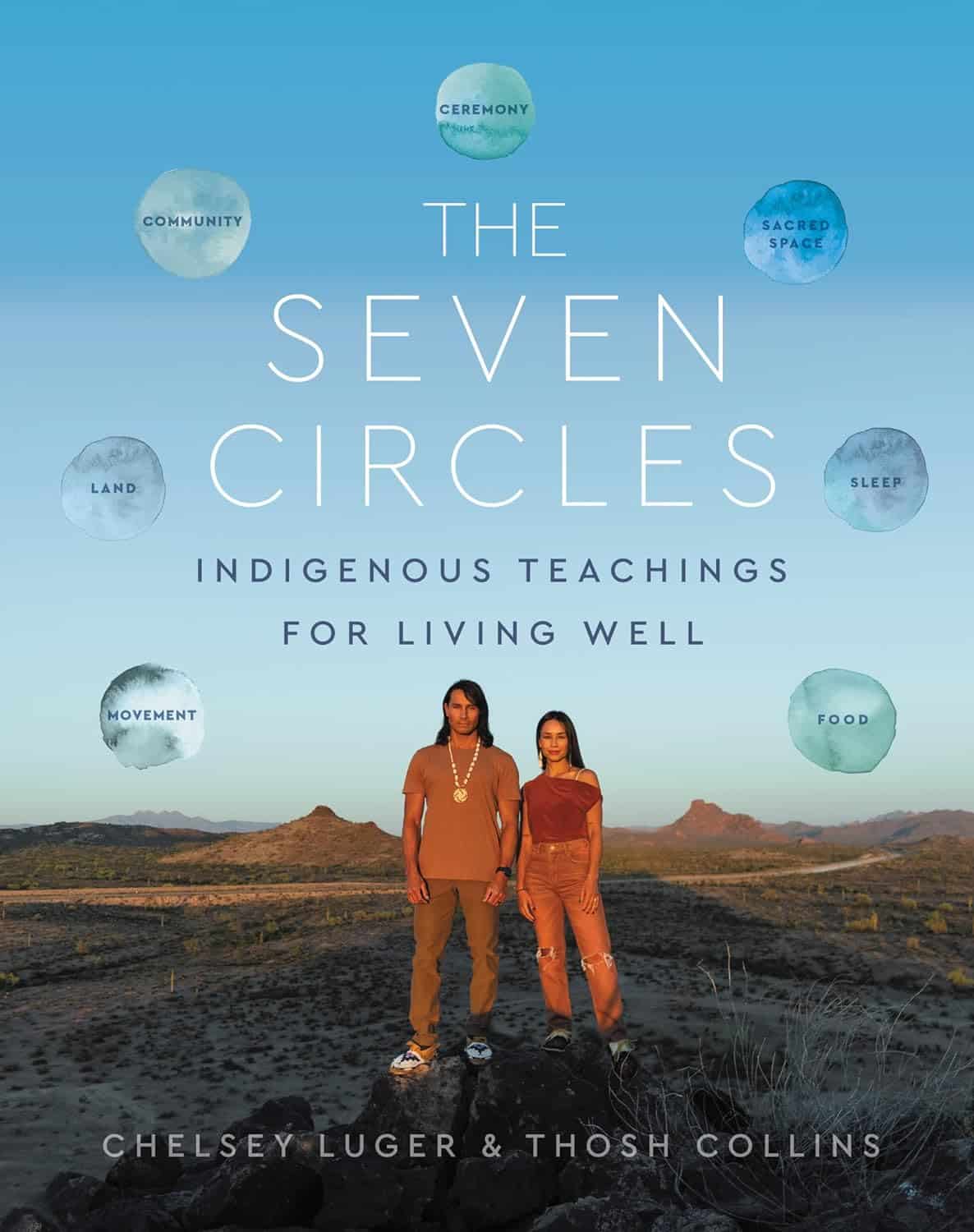
The Seven Circles – by Chelsey Luger & Thosh Collins
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
At first glance, this can seem like an unscientific book—you won’t find links to studies in this one, for sure! However, if we take a look at the seven circles in question, they are:
- Food
- Movement
- Sleep
- Ceremony
- Sacred Space
- Land
- Community
Regular 10almonds readers may notice that these seven items contain five of the things strongly associated with the “supercentenarian Blue Zones”. (If you are wondering why Native American reservations are not Blue Zones, the answer there lies less in health science and more in history and sociology, and what things have been done to a given people).
The authors—who are Native American, yes—present in one place a wealth of knowledge and know-how. Not even just from their own knowledge and their own respective tribes, but gathered from other tribes too.
Perhaps the strongest value of this book to the reader is in the explanation of noting the size of each of those circles, how they connect with each other, and providing a whole well-explained system for how we can grow each of them in harmony with each other.
Or to say the same thing in sciencey terms: how to mindfully improve integrated lifestyle factors synergistically for greater efficacy and improved health-adjusted quality-of-life years.
Bottom line: if you’re not averse to something that mostly doesn’t use sciencey terms of have citations to peer-reviewed studies peppered through the text, then this book has wisdom that’s a) older than the pyramids of Giza, yet also b) highly consistent with our current best science of Blue Zone healthy longevity.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Alzheimer’s Causative Factors To Avoid
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Best Brains Bar Nun?
This is Dr. David Snowdon. He’s an epidemiologist, and one of the world’s foremost experts on Alzheimer’s disease. He was also, most famously, the lead researcher of what has become known as “The Nun Study”.
We recently reviewed his book about this study:
…which we definitely encourage you to check out, but we’ll do our best to summarize its key points today!
Reassurance up-front: no, you don’t have to become a nun
The Nun Study
In 1991, a large number (678) of nuns were recruited for what was to be (and until now, remains) the largest study of its kind into the impact of a wide variety of factors on aging, and in particular, Alzheimer’s disease.
Why it was so important: because the nuns were all from the same Order, had the same occupation (it’s a teaching Order), with very similar lifestyles, schedules, socioeconomic status, general background, access to healthcare, similar diets, same relationship status (celibate), same sex (female), and many other factors also similar, this meant that most of the confounding variables that confound other studies were already controlled-for here.
Enrollment in the study also required consenting to donating one’s brain for study post-mortem—and of those who have since died, indeed 98% of them have been donated (the other 2%, we presume, may have run into technical administrative issues with the donation process, due to the circumstances of death and/or delays in processing the donation).
How the study was undertaken
We don’t have enough space to describe the entire methodology here, but the gist of it is:
- Genetic testing for relevant genetic factors
- Data gathered about lives so far, including not just medical records but also autobiographies that the nuns wrote when they took their vows (at ages 19–21)
- Extensive ongoing personal interviews about habits, life choices, and attitudes
- Yearly evaluations including memory tests and physical function tests
- Brain donation upon death
What they found
Technically, The Nun Study is still ongoing. Of the original 678 nuns (aged 75–106), three are still alive (based on the latest report, at least).
However, lots of results have already been gained, including…
Genes
A year into the study, in 1992, the “apolipoprotein E” (APOE) gene was established as a likely causative factor in Alzheimer’s disease. This is probably not new to our readers in 2024, but there are interesting things being learned even now, for example:
The Alzheimer’s Gene That Varies By Race & Sex
…but watch out! Because also:
Alzheimer’s Sex Differences May Not Be What They Appear
Words
Based on the autobiographies written by the nuns in their youth upon taking their vows, there were two factors that were later correlated with not getting dementia:
- Longer sentences
- Positive outlook
- “Idea density”
That latter item means the relative linguistic density of ideas and complexity thereof, and the fluency and vivacity with which they were expressed (this was not a wishy-washy assessment; there was a hard-science analysis to determine numbers).
Want to spruce up yours? You might like to check out:
Reading, Better: Reading As A Cognitive Exercise
…for specific, evidence-based ways to tweak your reading to fight cognitive decline.
Food
While the dietary habits of the nuns were fairly homogenous, those who favored eating more and cooked greens, beans, and tomatoes, lived longer and with healthier brains.
See also: Brain Food? The Eyes Have It!
Other aspects of brain health & mental health
The study also found that nuns who avoided stroke and depression, were also less likely to get dementia.
For tending to these, check out:
- Two Things You Can Do To Improve Stroke Survival Chances
- Depression, And The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
Community & Faith
Obviously, in this matter the nuns were quite a homogenous group, scoring heavily in community and faith. What’s relevant here is the difference between the nuns, and other epidemiological studies in other groups (invariably not scoring so highly).
Community & faith are considered, separately and together, to be protective factors against dementia.
Faith may be something that “you have it or you don’t” (we’re a health science newsletter, not a theological publication, but for the interested, philosopher John Stuart Mill’s 1859 essay “On Liberty“ makes a good argument for it not being something one can choose, prompting him to argue for religious tolerance, on the grounds that religious coercion is a futile effort precisely because a person cannot choose to dis/believe something)
…but community can definitely be chosen, nurtured, and grown. We’ve written about this a bit before:
You might also like to check out this great book on the topic:
Purpose: Design A Community And Change Your Life – by Gina Bianchini
Want more?
We gave a ground-up primer on avoiding Alzheimer’s and other dementias; check it out:
How To Reduce Your Alzheimer’s Risk
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: