The Yoga of Breath – by Richard Rosen
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
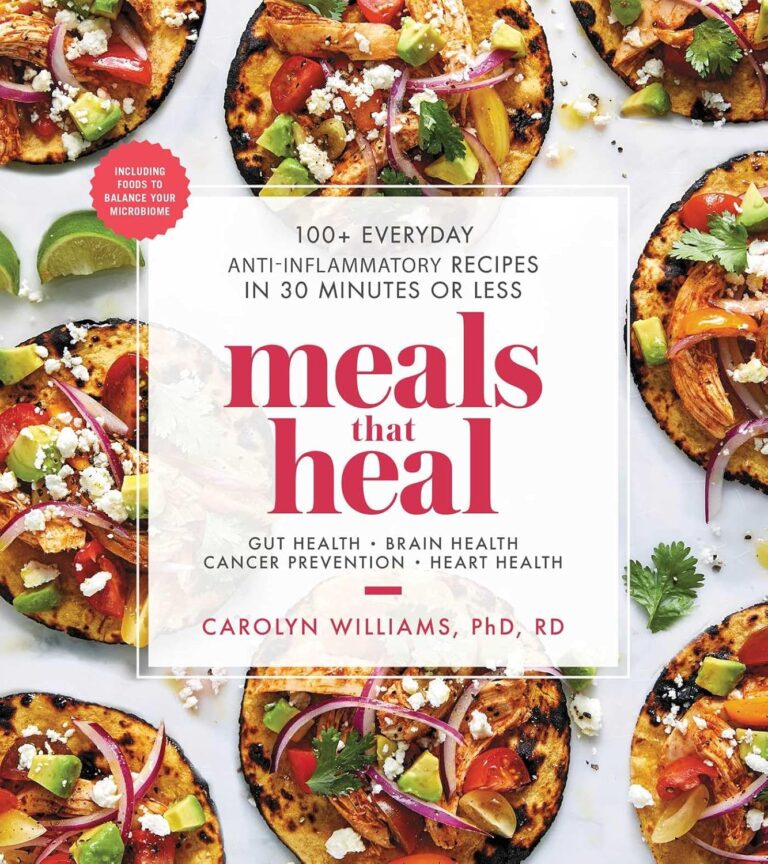
You probably know to breathe through your nose, and to breathe with your diaphragm. But did you know you’re usually only breathing through one nostril at a time, and alternate between nostrils every few hours? And did you know how to breathe through both nostrils equally instead, and the benefits that can bring?
The above is one example of many, of things that make this book stand out from the crowd when it comes to breathing exercises. Author Richard Rosen has a deep expertise in this topic, and explains everything clearly and comprehensively, without leaving room for ambiguity.
While most of the book focuses on the mechanics and physical techniques of breathing, he does also cover some more mindstate-related things too—without which, it wouldn’t be yoga.
If the book has a downside, it’s that its comprehensive nature could be off-putting to readers new to breathing work in general. However, since he does explain everything from the ground up, that’s no reason to be put off this book, iff you’re serious about learning.
Bottom line: if you’d like a deeper understanding of breathwork than “breathe slowly through your nose, using your diaphragm”, this book will teach you depths of breathing you probably didn’t know were possible.
Click here to check out The Yoga of Breath, and catch yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
A drug that can extend your life by 25%? Don’t hold your breath
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Every few weeks or months, the media reports on a new study that tantalisingly dangles the possibility of a new drug to give us longer, healthier lives.
The latest study centres around a drug involved in targeting interleukin-11, a protein involved in inflammation. Blocking this protein appeared to help mice stave off disease and extend their life by more than 20%.
If only defying the ravages of time could be achieved through such a simple and effort-free way – by taking a pill. But as is so often the case, the real-world significance of these findings falls a fair way short of the hype.
Halfpoint/Shutterstock The role of inflammation in disease and ageing
Chronic inflammation in the body plays a role in causing disease and accelerating ageing. In fact, a relatively new label has been coined to represent this: “inflammaging”.
While acute inflammation is an important response to infection or injury, if inflammation persists in the body, it can be very damaging.
A number of lifestyle, environmental and societal drivers contribute to chronic inflammation in the modern world. These are largely the factors we already know are associated with disease and ageing, including poor diet, lack of exercise, obesity, stress, lack of sleep, lack of social connection and pollution.
While addressing these issues directly is one of the keys to addressing chronic inflammation, disease and ageing, there are a number of research groups also exploring how to treat chronic inflammation with pharmaceuticals. Their goal is to target and modify the molecular and chemical pathways involved in the inflammatory process itself.
What the latest research shows
This new interleukin-11 research was conducted in mice and involved a number of separate components.
In one component of this research, interleukin-11 was genetically knocked out in mice. This means the gene for this chemical mediator was removed from these mice, resulting in the mice no longer being able to produce this mediator at all.
In this part of the study, the mice’s lives were extended by over 20%, on average.
Another component of this research involved treating older mice with a drug that blocks interleukin-11.
Injecting this drug into 75-week old mice (equivalent to 55-year-old humans) was found to extend the life of mice by 22-25%.
These treated mice were less likely to get cancer and had lower cholesterol levels, lower body weight and improved muscle strength and metabolism.
From these combined results, the authors concluded, quite reasonably, that blocking interleukin-11 may potentially be a key to mitigating age-related health effects and improving lifespan in both mice and humans.
Why you shouldn’t be getting excited just yet
There are several reasons to be cautious of these findings.
First and most importantly, this was a study in mice. It may be stating the obvious, but mice are very different to humans. As such, this finding in a mouse model is a long way down the evidence hierarchy in terms of its weight.
Research shows only about 5% of promising findings in animals carry over to humans. Put another way, approximately 95% of promising findings in animals may not be translated to specific therapies for humans.
Second, this is only one study. Ideally, we would be looking to have these findings confirmed by other researchers before even considering moving on to the next stage in the knowledge discovery process and examining whether these findings may be true for humans.
We generally require a larger body of evidence before we get too excited about any new research findings and even consider the possibility of human trials.
Third, even if everything remains positive and follow-up studies support the findings of this current study, it can take decades for a new finding like this to be translated to successful therapies in humans.
Until then, we can focus on doing the things we already know make a huge difference to health and longevity: eating well, exercising, maintaining a healthy weight, reducing stress and nurturing social relationships.
Hassan Vally, Associate Professor, Epidemiology, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Peanuts vs Hazelnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing peanuts to hazelnuts, we picked the hazelnuts.
Why?
It was close!
In terms of macros, peanuts have more protein while hazelnuts have more fiber and fat; the fat is healthy (mostly monounsaturated, some polyunsaturated, and very little saturated; less saturated fat than peanuts), so all in all, we’ll call this category a modest, subjective win for hazelnuts (since it depends on what we consider most important).
In the category of vitamins, peanuts have more of vitamins B2, B3, B5, B9, and choline, while hazelnuts have more of vitamins A, B1, B6, C, E, and K, making this one a marginal win for hazelnuts.
When it comes to minerals, peanuts have more magnesium, phosphorus, selenium, and zinc, while hazelnuts have more calcium, copper, iron, and manganese, so we’re calling it a tie on minerals.
Adding up the sections makes for a very close win for hazelnuts, but by all means enjoy both (unless you are allergic, of course)!
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts!
Enjoy!
Share This Post
-
6 Worst Foods That Cause Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How many do you consume?
The hit list
Dr. Li bids us avoid:
High carb, low fiber foods: consuming a diet high in carbohydrates, particularly refined carbs like cakes, white bread, pizza, and sugary syrups, can significantly harm brain health. Over time, imbalanced (i.e. not balanced with fiber) carbohydrate consumption leads to the growth of visceral fat (not the same as subcutaneous fat, which is the squishy bits just under your skin; visceral fat is further underneath, around your viscera), , which triggers systemic inflammation and oxidative stress. These processes disrupt communication between brain cells, impair memory, and increase the risk of diseases like Alzheimer’s and Parkinson’s. High carb diets can also contribute to metabolic syndrome—a cluster of conditions, including diabetes, obesity and high blood pressure—that damage blood vessels, leading to strokes and vascular dementia.
Trans fats: these are region-bound, as they’re banned in some places and not others—check your local regulations. Found in processed foods such as fried items, baked goods, packaged snacks, and margarine, trans fats are created through hydrogenation, which makes fats more stable at room temperature. These artificial fats raise bad cholesterol, lower good cholesterol, and promote atherosclerosis. This damages the brain by reducing oxygen supply, triggering chronic inflammation, and increasing the risk of Alzheimer’s and dementia.
Sodas: regular consumption of sodas, whether sugary or artificially sweetened, is harmful to brain health. A single can of soda contains around 9 teaspoons of sugar, which overwhelms metabolism, contributes to insulin resistance, and leads to inflammation. These effects damage blood vessels and brain tissue, disrupt neuron function, and increase the risk of type 2 diabetes and dementia. Furthermore, insulin resistance caused by excessive sugar intake can impair neuronal survival, activate immune responses, and exacerbate cognitive decline. As for the artificial sweeteners, the mechanism of harm depends on the sweetener (and some can also mess up insulin response, for reasons that are not entirely clear yet, but they measurably do), but even picking the healthiest artificial sweetener, training your palate to enjoy hyper-sweetened things will tend to lead to more sugar-laden food choices in other parts of one’s diet.
Processed foods: arguably a broad category that encompasses some of the above, but it’s important to consider it separately for catch-all purposes: these convenience foods, laden with artificial preservatives, colors, and sweeteners, harm brain health through chronic inflammation and usually a lack of essential nutrients. Processed foods are also a significant source of microplastics, which have been found to accumulate in the arteries, contributing to plaque build-up, atherosclerosis, and reduced blood flow to the brain. This combination of inflammation and oxidative stress from microplastics damages brain cells, paving the way for cognitive decline and dementia.
Seafood with high mercury levels: large fish such as tuna, swordfish, sharks, and tilefish accumulate high amounts of mercury, a potent neurotoxin. Fish that are larger, older, and/or higher up the food chain will have the most mercury (and other cumulative contaminants, for that matter, but we’re considering mercury here). Mercury disrupts essential brain chemicals like dopamine and serotonin, triggering oxidative stress and damaging brain cells. Chronic exposure to mercury leads to inflammation and neuroinflammation, both of which increase the risk of Alzheimer’s and dementia.
Alcohol: contrary to popular belief, any amount of alcohol is detrimental to brain health. While red wine is often promoted for its health benefits, the purported positive effects come from polyphenols, not the alcohol itself, and (for example) resveratrol from red wine cannot be delivered in meaningful doses without drinking an impossibly large quantity. Alcohol is a neurotoxin that can damage or kill brain cells, impair neuronal communication, and lead to cognitive decline. Excessive drinking results in hangover symptoms like headaches and brain fog, which are indicators of its harmful impact on the brain. Chronic alcohol consumption exacerbates neuron death, increases inflammation, and raises the risk of dementia.
As for what to eat instead?
Dr. Li recommends including foods such as:
- foods rich in omega-3s that aren’t mercury-laden fish, e.g. flaxseeds, chia seeds, walnuts, and hemp seeds, as they reduce inflammation, protect blood vessel linings, and prevent vascular dementia.
- berries, and in particular he recommends organic strawberries, which are rich in ellagic acid and anthocyanins, which improve memory, reduce depressive symptoms, and enhance cognitive function.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
Related Posts
-
The Best 4 Pool Exercises to Strengthen Your Core & Tone Up
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of people don’t love working on their core strength, but exercising in the pool can make it a lot more enjoyable, as well as minimizing risk of injury.
Dr Alyssa Kuhn, arthritis specialist, also advises “being in the water also helps to control for balance and can offload the joints so they aren’t as painful”:
The gentlest exercise
The specific exercises she recommends are:
Wood Chops
Stagger your feet, clasp your hands, and submerge them in the water. Now, move your hands diagonally from one side to the other. This engages your core and balance using water resistance. Perform 10–20 reps per side, exhaling on the hardest part.
Front Kick with Opposite Arm Press
Kick one leg forward while pushing the opposite arm out or overhead—higher kicks increase difficulty by requiring more balance. If balance isn’t sufficient for you yet, hold onto the pool wall if needed. Either way, engage the core to lift the leg. Do 20–30 reps alternating sides.
Wall Push-Ups
Place your hands on the pool wall, shoulder-width apart. Keep feet together and hips slightly tucked for core engagement. Next, move your chest toward the wall and push back while maintaining a straight body—avoid arching your back. Do 10–20 reps.
Arm Circles
Stand with your feet wider than shoulder-width. Clasp your hands, extend your arms, and submerge them in the water. Make large circular motions for resistance training. This can be done with straight or bent arms for different difficulty levels. Do 10–20 circles in each direction.
For more on each of these plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Osteoporosis & Exercises: Which To Do (And Which To Avoid)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Keep Cellulite At Bay
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Does anything actually get rid of cellulite? Nothing seems to❞
Let’s get the bad news over with in one go:
Nothing (that the scientific world currently knows of) can get rid of cellulite permanently, nor completely guard against it proactively. Which, given that it affects up to 98% of women to some degree, and often shows up not long after puberty (though it can appear at any time and often increases later in life), any pre-emptive health regime would need to be started as a child in any case.
As with many things that predominantly affect women, the world of medicine isn’t entirely sure what causes it, let alone how to effectively treat it.
Obviously hormones are implicated, namely estrogen.
Obviously adiposity is implicated, because one can’t have dimples in one’s fat if one doesn’t have enough fat to dimple.
Other hypothesized contributory factors include genetics, poor diet, inactivity, unhealthy lifestyle (in ways not previously mentioned, e.g. use of alcohol, tobacco, etc), accumulated toxins, and pregnancy.
Here’s an old paper (from 2004); today’s reviews say pretty much the same thing, but we love how succinctly (albeit, somewhat depressingly) this abstract states how little we know and how little we can do:
Cellulite: a review of its physiology and treatment
However, all is not lost!
There are some things that can affect how much cellulite we get, and there are some things that can reduce it, and even some things that can get rid of it completely—albeit temporarily.
First, a quick refresher on what it actually is, physiologically speaking: cellulite occurs when connective tissue bands pull the skin down in places, where fat tissue has been able to squeeze through. One of the reasons it is hypothesized women get this more than men is because our fat is not merely different in distribution and overall percentage, but also in how the fat cells stack up; we generally have have of a vertical stacking structure going on, while men generally have a more horizontal structure. This means that it can be easier for ours to get moved about differently, causing the connective tissue to pull on the skin unevenly in places.
With that in mind…
Prevention is, as we say, probably impossible if your body is running on estrogen. However, those contributory factors we mentioned above? Most of those are modifiable, including these things that it is hypothesized can reduce it:
Diet: as it seems to be worsened by inflammation (what isn’t?), an anti-inflammatory diet is recommended.
Exercise: there are three things here: 1) exercises to improve circulation and thus the body’s ability to sort things out by itself 2) HIIT exercise to reduce body fat percentage, if one has a high enough starting body fat percentage for that to be a healthy goal 3) mobility exercises, to ensure our connective tissues are the right amount of mobile.
Creams and lotions
These reduce the superficial appearance of cellulite, without actually treating the thing itself. Mostly they are caffeine-based, which when used topically increases blood flow and works as a local diuretic, reducing the water content of the fat cells, diminishing the appearance of the cellulite by making each fat cell physically smaller (while still containing the same amount of fat, and it’ll bounce back in size as soon as the body can restore osmotic balance).
Medical procedures
There are too many of these to discuss them all separately, but they all work on the principle of breaking up the tough bands of connective tissue to eliminate the dimpling of cellulite.
The methods they use vary from ultrasound to cryolipolysis to lasers to “vacuum-assisted precise tissue release”, which involves a suction pump and a multipronged robotic assembly with needles to administer anaesthetic as it goes and small blades to cut the connective tissues under the skin:
Tissue Stabilized–Guided Subcision for the Treatment of Cellulite
That last one definitely sounds like the least fun, but it’s also the only one that doesn’t take months to maybe see results.
Cellulite can and almost certainly will come back after all of these.
Home remedies
Aside from at-home versions of the above (not the robots with vacuum pumps and needles and microblades, hopefully, but for example homemade caffeine creams), and of course diet and exercise which can be considered “home remedies”, there are two more things worth mentioning:
Dry brushing: using a body brush to, as the name suggests, simply brush one’s skin. The “dry” aspect here is simply that it’s not done in the bath or shower; it’s done while dry. It can improve local circulation of blood and lymph, allowing for better detoxification and redistribution of needed bodily resources.
Here’s an example dry brushing body brush on Amazon; this writer has one and hates it, but I’ve also tried with other kinds of brush and hate them too, so it seems to be a me thing rather than a brush thing, and I have desisted in trying, now. Maybe you will like it better; many people do.
Self-massage: or massage by someone else, if that’s an option for you and you prefer. In this case, it works by a different mechanism than dry brushing; this time it’s working by the same principle as the medical techniques described in the previous section; it’s physically breaking down the toughened bits of connective tissue.
Here’s an example wooden massage roller on Amazon; this writer has one and loves it; it’s sooooooo good. I got it as a matter of general maintenance for my fascia, but it’s also very good if I get a muscular pain now and again. As for cellulite, I personally get just a little cellulite sometimes (in the backs of my thighs), and whenever I use this regularly, it goes away for at least a while.
A quick note in closing
Cellulite is normal for women and is not unhealthy. Much like gray hair for example, it’s something that can be increased by poor health, but the thing itself isn’t intrinsically unhealthy, and most of us get it to some degree at some point.
Nevertheless, aesthetic factors can also have a role to play in mental health, and we tend to feel best when we like the way our body looks. If for you that means wanting less/no cellulite, then the above are some ways towards that.
As a bonus, most of the nonmedical options are directly good for the physical health anyway, so doing them is of course good.
In particular that last one (the wooden massage roller), because that connective tissue we talked about? It matters for a lot more than just cellulite, and is heavily implicated in a lot of kinds of chronic pain, so it pays to keep it in good health:
Fascia: Why (And How) You Should Take Care Of Yours
(that article, also written by this same writer by the way, suggests a vibrating foam roller—those are very popular; I just really love my wooden one, and find it more effective)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
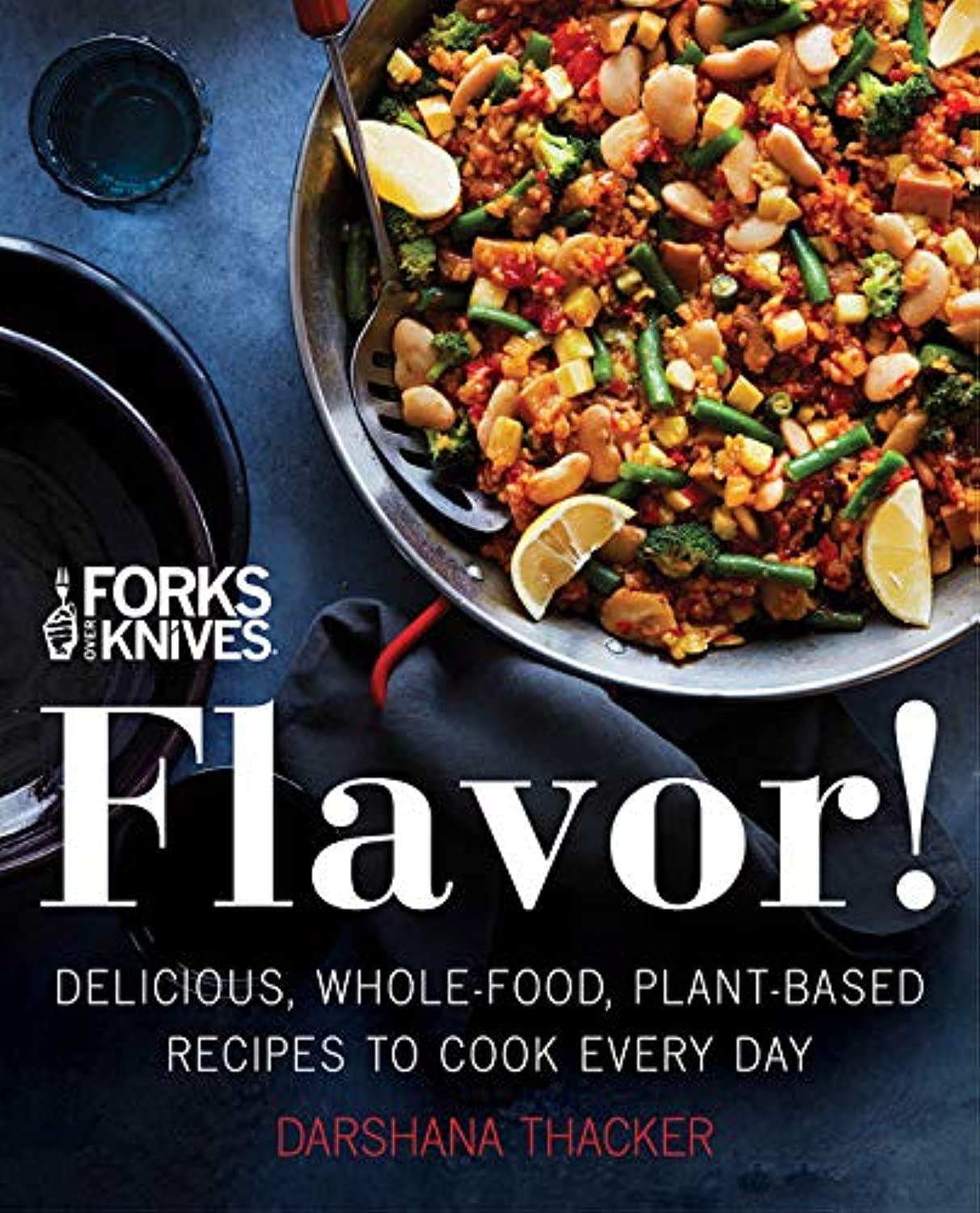
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: