The Worry Trick – by Dr. David Carbonell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Worry is a time-sink that rarely does us any good, and often does us harm. Many books have been written on how to fight anxiety… That’s not what this book’s about.
Dr. David Carbonell, in contrast, encourages the reader to stop trying to avoid/resist anxiety, and instead, lean into it in a way that detoothes it.
He offers various ways of doing this, from scheduling time to worry, to substituting “what if…” with “let’s pretend…”, and guides the reader through exercises to bring about a sort of worry-desensitization.
The style throughout is very much pop-psychology and is very readable.
If the book has a weak point, it’s that it tends to focus on worrying less about unlikely outcomes, rather than tackling worry that occurs relating to outcomes that are likely, or even known in advance. However, some of the techniques will work for such also! That’s when Dr. Carbonell draws from Acceptance and Commitment Therapy (ACT).
Bottom line: if you would like to lose less time and energy to worrying, then this is a fine book for you.
Click here to check out The Worry Trick, and repurpose your energy reserves!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Exercise with Type 1 Diabetes – by Ginger Vieira
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you or a loved one has Type 1 Diabetes, you’ll know that exercise can be especially frustrating…
- If you don’t do it, you risk weight gain and eventual insulin resistance.
- If you do it, you risk dangerous hypos, or perhaps hypers if you took off your pump or skipped a bolus.
Unfortunately, the popular medical advice is “well, just do your best”.
Ginger Vieira is Type 1 Diabetic, and writes with 20+ experience of managing her diabetes while being a keen exerciser. As T1D folks out there will also know, comorbidities are very common; in her case, fibromyalgia was the biggest additional blow to her ability to exercise, along with an underactive thyroid. So when it comes to dealing with the practical nuts and bolts of things, she (while herself observing she’s not a doctor, let alone your doctor) has a lot more practical knowledge than an endocrinologist (without diabetes) behind a desk.
Speaking of nuts and bolts, this book isn’t a pep talk.
It has a bit of that in, but most of it is really practical information, e.g: using fasted exercise (4 hours from last meal+bolus) to prevent hypos, counterintuitive as that may seem—the key is that timing a workout for when you have the least amount of fast-acting insulin in your body means your body can’t easily use your blood sugars for energy, and draws from your fat reserves instead… Win/Win!
That’s just one quick tip because this is a 1-minute review, but Vieira gives:
- whole chapters, with example datasets (real numbers)
- tech-specific advice, e.g. pump, injection, etc
- insulin-specific advice, e.g. fast vs slow, and adjustments to each in the context of exercise
- timing advice re meal/bolus/exercise for different insulins and techs
- blood-sugar management advice for different exercise types (aerobic/anaerobic, sprint/endurance, etc)
…and lots more that we don’t have room to mention here
Basically… If you or a loved one has T1D, we really recommend this book!
Order a copy of “Exercise with Type 1 Diabetes” from Amazon today!
Share This Post
-
Do Hard Things – by Steve Magness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s easy to say that we must push ourselves if we want to achieve worthwhile things—and it’s also easy to push ourselves into an early grave by overreaching. So, how to do the former, without doing the latter?
That’s what this book’s about. The author, speaking from a background in the science of sports psychology, applies his accumulated knowledge and understanding to the more general problems of life.
Most of us are, after all, not sportspeople or if we are, not serious ones. Those few who are, will get benefit from this book too! But it’s mostly aimed at the rest of us who are trying to work out whether/when we should scale up, scale back, change track, or double down:
- How much can we really achieve in our career?
- How about in retirement?
- Do we ever really get too old for athletic feats, or should we keep pressing on?
Magness brings philosophy and psychological science together, to help us sort our way through.
Nor is this just a pep talk—there’s readily applicable, practical, real-world advice here, things to enable us to do our (real!) best without getting overwhelmed.
The style is pop-science, very easy-reading, and clear and comprehensible throughout—without succumbing to undue padding either.
Bottom line: this is a very pleasant read, that promises to make life more meaningful and manageable at the same time. Highly recommendable!
Click here to check out Do Hard Things, and get the most out of life!
Share This Post
-
Qigong: A Breath Of Fresh Air?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Qigong: Breathing Is Good (Magic Remains Unverified)
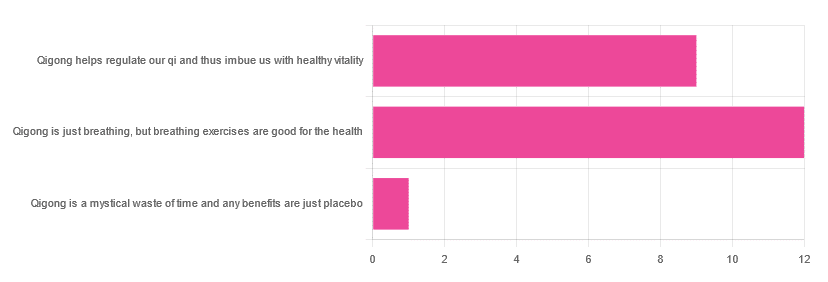
In Tuesday’s newsletter, we asked you for your opinions of qigong, and got the above-depicted, below-described, set of responses:
- About 55% said “Qigong is just breathing, but breathing exercises are good for the health”
- About 41% said “Qigong helps regulate our qi and thus imbue us with healthy vitality”
- One (1) person said “Qigong is a mystical waste of time and any benefits are just placebo”
The sample size was a little low for this one, but the results were quite clearly favorable, one way or another.
So what does the science say?
Qigong is just breathing: True or False?
True or False, depending on how we want to define it—because qigong ranges in its presentation from indeed “just breathing exercises”, to “breathing exercises with visualization” to “special breathing exercises with visualization that have to be exactly this way, with these hand and sometimes body movements also, which also must be just right”, to far more complex definitions that involve qi by various mystical definitions, and/or an appeal to a scientific analog of qi; often some kind of bioelectrical field or such.
There is, it must be said, no good quality evidence for the existence of qi.
Writer’s note, lest 41% of you want my head now: I’ve been practicing qigong and related arts for about 30 years and find such to be of great merit. This personal experience and understanding does not, however, change the state of affairs when it comes to the availability (or rather, the lack) of high quality clinical evidence to point to.
Which is not to say there is no clinical evidence, for example:
Acute Physiological and Psychological Effects of Qigong Exercise in Older Practitioners
…found that qigong indeed increased meridian electrical conductance!
Except… Electrical conductance is measured with galvanic skin responses, which increase with sweat. But don’t worry, to control for that, they asked participants to dry themselves with a towel. Unfortunately, this overlooks the fact that a) more sweat can come where that came from, because the body will continue until it is satisfied of adequate homeostasis, and b) drying oneself with a towel will remove the moisture better than it’ll remove the salts from the skin—bearing in mind that it’s mostly the salts, rather than the moisture itself, that improve the conductivity (pure distilled water does conduct electricity, but not very well).
In other words, this was shoddy methodology. How did it pass peer review? Well, here’s an insight into that journal’s peer review process…
❝The peer-review system of EBCAM is farcical: potential authors who send their submissions to EBCAM are invited to suggest their preferred reviewers who subsequently are almost invariably appointed to do the job. It goes without saying that such a system is prone to all sorts of serious failures; in fact, this is not peer-review at all, in my opinion, it is an unethical sham.❞
~ Dr. Edzard Ernst, a founding editor of EBCAM (he since left, and decries what has happened to it since)
One of the other key problems is: how does one test qigong against placebo?
Scientists have looked into this question, and their answers have thus far been unsatisfying, and generally to the tune of the true-but-unhelpful statement that “future research needs to be better”:
Problems of scientific methodology related to placebo control in Qigong studies: A systematic review
Most studies into qigong are interventional studies, that is to say, they measure people’s metrics (for example, blood pressure, heart rate, maybe immune function biomarkers, sleep quality metrics of various kinds, subjective reports of stress levels, physical biomarkers of stress levels, things like that), then do a course of qigong (perhaps 6 weeks, for example), then measure them again, and see if the course of qigong improved things.
This almost always results in an improvement when looking at the before-and-after, but it says nothing for whether the benefits were purely placebo.
We did find one study that claimed to be placebo-controlled:
…but upon reading the paper itself carefully, it turned out that while the experimental group did qigong, the control group did a reading exercise. Which is… Saying how well qigong performs vs reading (qigong did outperform reading, for the record), but nothing for how well it performs vs placebo, because reading isn’t a remotely credible placebo.
See also: Placebo Effect: Making Things Work Since… Well, A Very Long Time Ago ← this one explains a lot about how placebo effect does work
Qigong is a mystical waste of time: True or False?
False! This one we can answer easily. Interventional studies invariably find it does help, and the fact remains that even if placebo is its primary mechanism of action, it is of benefit and therefore not a waste of time.
Which is not to say that placebo is its only, or even necessarily primary, mechanism of action.
Even from a purely empirical evidence-based medicine point of view, qigong is at the very least breathing exercises plus (usually) some low-impact body movement. Those are already two things that can be looked at, mechanistic processes pointed to, and declarations confidently made of “this is an activity that’s beneficial for health”.
See for example:
- Effects of Qigong practice in office workers with chronic non-specific low back pain: A randomized control trial
- Qigong for the Prevention, Treatment, and Rehabilitation of COVID-19 Infection in Older Adults
- Impact of Medical Qigong on quality of life, fatigue, mood and inflammation in cancer patients: a randomized controlled trial
…and those are all from respectable journals with meaningful peer review processes.
None of them are placebo-controlled, because there is no real option of “and group B will only be tricked into believing they are doing deep breathing exercises with low-impact movements”; that’s impossible.
But! They each show how doing qigong reliably outperforms not doing qigong for various measurable metrics of health.
And, we chose examples with physical symptoms and where possible empirically measurable outcomes (such as COVID-19 infection levels, or inflammatory responses); there are reams of studies showings qigong improves purely subjective wellbeing—but the latter could probably be claimed for any enjoyable activity, whereas changes in inflammatory biomarkers, not such much.
In short: for most people, it indeed reliably helps with many things. And importantly, it has no particular risks associated with it, and it’s almost universally framed as a complementary therapy rather than an alternative therapy.
This is critical, because it means that whereas someone may hold off on taking evidence-based medicines while trying out (for example) homeopathy, few people are likely to hold off on other treatments while trying out qigong—since it’s being viewed as a helper rather than a Hail-Mary.
Want to read more about qigong?
Here’s the NIH’s National Center for Complementary and Integrative Health has to say. It cites a lot of poor quality science, but it does mention when the science it’s citing is of poor quality, and over all gives quite a rounded view:
Enjoy!
Share This Post
Related Posts
-
The Sugary Food That Lowers Blood Sugars
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Loved the article on goji berries! I read they are good for blood sugars, is that true despite the sugar content?❞
Most berries are! Fruits that are high in polyphenols (even if they’re high in sugar), like berries, have a considerable net positive impact on glycemic health:
- Polyphenols and Glycemic Control
- Polyphenols and their effects on diabetes management: A review
- Dietary polyphenols as antidiabetic agents: Advances and opportunities
And more specifically:
Dietary berries, insulin resistance and type 2 diabetes: an overview of human feeding trials
Read more: Which Sugars Are Healthier, And Which Are Just The Same?
As for goji berries specifically, they’re very high indeed in polyphenols, and also have a hypoglycemic effect, i.e., they lower blood sugar levels (and as a bonus, increases HDL (“good” cholesterol) levels too, but that’s not the topic here):
❝The results of our study indicated a remarkable protective effect of LBP in patients with type 2 diabetes. Serum glucose was found to be significantly decreased and insulinogenic index increased during OMTT after 3 months administration of LBP. LBP also increased HDL levels in patients with type 2 diabetes. It showed more obvious hypoglycemic efficacy for those people who did not take any hypoglycemic medicine compared to patients taking hypoglycemic medicines. This study showed LBP to be a good potential treatment aided-agent for type 2 diabetes.❞
- LBP = Lycium barbarum polysaccharide, i.e. polysaccharide in/from goji berries
- OMTT = Oral metabolic tolerance test, a test of how well the blood sugars avoid spiking after a meal
For more about goji berries (and also where to get them), for reference our previous article is at:
Goji Berries: Which Benefits Do They Really Have?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Psychedelics and Psychotherapy – Edited by Dr. Tim Read & Maria Papaspyrou
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A quick note on authorship, first: this book is edited by the psychiatrist and psychotherapist credited above, but after the introductory section, the rest of the chapters are written by experts on the individual topics.As such, the style will vary somewhat, from chapter to chapter.
What this book isn’t: “try drugs and feel better!”
Rather, the book explores the various ways in which assorted drugs can help people to—even if just briefly—shed things they didn’t know they were carrying, or otherwise couldn’t put down, and access parts of themselves they otherwise couldn’t.
We also get to read a lot about the different roles the facilitator can play in guiding the therapeutic process, and what can be expected out of each kind of experience. This varies a lot from one drug to another, so it makes for very worthwhile reading, if that’s something you might consider pursuing. Knowledge makes for much more informed choices!
Bottom line: if you’re curious about the therapeutic potential of psychedelics, and want a reference that’s more personal than dry clinical studies, but still more “safe and removed” than diving in by yourself, this is the book for you.
Click here to check out Psychedelics and Psychotherapy, and expand your understanding!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Willpower: A Muscle To Flex, Or Spoons To Conserve?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Willpower: A Muscle To Flex, Or Spoons To Conserve?
We have previously written about motivation; this one’s not about that.
Rather, it’s about willpower itself, and especially, the maintenance of such. Which prompts the question…
Is willpower something that can be built up through practice, or something that is a finite resource that can be expended?
That depends on you—and your experiences.
- Some people believe willpower is a metaphorical “muscle” that must be exercised to be built up
- Some people believe willpower is a matter of metaphorical “spoons” that can be used up
A quick note on spoon theory: this traces its roots to Christine Miserandino’s 2003 essay about chronic illness and the management of limited energy. She details how she explained this to a friend in a practical fashion, she gave her a bunch of spoons from her kitchen, as an arbitrary unit of energy currency. These spoons would then need to be used to “pay” for tasks done; soon her friend realised that if she wanted to make it through the day, she was going to have to give more forethought to how she would “spend” her spoons, or she’d run out and be helpless (and perhaps hungry and far from home) before the day’s end. So, the kind of forethought and planning that a lot of people with chronic illnesses have to give to every day’s activities.
You can read it here: But You Don’t Look Sick? The Spoon Theory
So, why do some people believe one way, and some believe the other? It comes down to our experiences of our own willpower being built or expended. Researchers (Dr. Vanda Siber et al.) studied this, and concluded:
❝The studies support the idea that what people believe about willpower depends, at least in part, on recent experiences with tasks as being energizing or draining.❞
Source: Autonomous Goal Striving Promotes a Nonlimited Theory About Willpower
In other words, there’s a difference between going out running each morning while healthy, and doing so with (for example) lupus.
On a practical level, this translates to practicable advice:
- If something requires willpower but is energizing, this is the muscle kind! Build it.
- If something requires willpower and is draining, this is the spoons kind! Conserve it.
Read the above two bullet-points as many times as necessary to cement them into your hippocampus, because they are the most important message of today’s newsletter.
Do you tend towards the “nonlimited” belief, despite getting tired? If so, here’s why…
There is something that can continue to empower us even when we get physically fatigued, and that’s the extent to which we truly get a choice about what we’re doing. In other words, that “Autonomous” at the front of the title of the previous study, isn’t just word salad.
- If we perceive ourselves as choosing to do what we are doing, with free will and autonomy (i.e., no externally created punitive consequences), we will feel much more empowered, and that goes for our willpower too.
- If we perceive ourselves as doing what we have to (or suffer the consequences), we’ll probably do it, but we’ll find it draining, and that goes for our willpower too.
Until such a time as age-related physical and mental decline truly take us, we as humans tend to gradually accumulate autonomy in our lives. We start as literal babies, then are children with all important decisions made for us, then adolescents building our own identity and ways of doing things, then young adults launching ourselves into the world of adulthood (with mixed results), to a usually more settled middle-age that still has a lot of external stressors and responsibilities, to old age, where we’ve often most things in order, and just ourselves and perhaps our partner to consider.
Consequently…
Age differences in implicit theories about willpower: why older people endorse a nonlimited theory
…which explains why the 30-year-old middle-manager might break down and burn out and stop going to work, while an octogenarian is busy training for a marathon daily before getting back to their daily book-writing session, without fail.
One final thing…
If you need a willpower boost, have a snack*. If you need to willpower boost to avoid snacking, then plan for this in advance by finding a way to keep your blood sugars stable. Because…
The physiology of willpower: linking blood glucose to self-control
*Something that will keep your blood sugars stable, not spike them. Nuts are a great example, unless you’re allergic to such, because they have a nice balance of carbohydrates, protein, and healthy fats.
Want more on that? Read: 10 Ways To Balance Blood Sugars
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: