The Princess of Wales wants to stay cancer-free. What does this mean?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Catherine, Princess of Wales, has announced she has now completed a course of preventive chemotherapy.
The news comes nine months after the princess first revealed she was being treated for an unspecified form of cancer.
In the new video message released by Kensington Palace, Princess Catherine says she’s focused on doing what she can to stay “cancer-free”. She acknowledges her cancer journey is not over and the “path to recovery and healing is long”.
While we don’t know the details of the princess’s cancer or treatment, it raises some questions about how we declare someone fully clear of the disease. So what does being – and staying – “cancer-free” mean?

What’s the difference between being cancer-free and in remission?
Medically, “cancer-free” means two things. First, it means no cancer cells are able to be detected in a patient’s body using the available testing methods. Second, there is no cancer left in the patient.
These might sound basically the same. But this second aspect of “cancer-free” can be complicated, as it’s essentially impossible to be sure no cancer cells have survived a treatment.

It only takes a few surviving cells for the cancer to grow back. But these cells may not be detectable via testing, and can lie dormant for some time. The possibility of some cells still surviving means it is more accurate to say a patient is “in remission”, rather than “cancer-free”.
Remission means there is no detectable cancer left. Once a patient has been in remission for a certain period of time, they are often considered to be fully “cancer-free”.
Princess Catherine was not necessarily speaking in the strict medical sense. Nonetheless, she is clearly signalling a promising step in her recovery.
What happens during remission?
During remission, patients will usually undergo surveillance testing to make sure their cancer hasn’t returned. Detection tests can vary greatly depending on both the patient and their cancer type.
Many tests involve simply looking at different organs to see if there are cancer cells present, but at varying levels of complexity.
Some cancers can be detected with the naked eye, such as skin cancers. In other cases, technology is needed: colonoscopies for colorectal cancers, X-ray mammograms for breast cancers, or CT scans for lung cancers. There are also molecular tests, which test for the presence of cancer cells using protein or DNA from blood or tissue samples.
For most patients, testing will continue for years at regular intervals. Surveillance testing ensures any returning cancer is caught early, giving patients the best chance of successful treatment.
Remaining in remission for five years can be a huge milestone in a patient’s cancer journey. For most types of cancer, the chances of cancer returning drop significantly after five years of remission. After this point, surveillance testing may be performed less frequently, as the patients might be deemed to be at a lower risk of their cancer returning.

Measuring survival rates
Because it is very difficult to tell when a cancer is “cured”, clinicians may instead refer to a “five-year survival rate”. This measures how likely a cancer patient is to be alive five years after their diagnosis.
For example, data shows the five-year survival rate for bowel cancer among Australian women (of all ages) is around 70%. That means if you had 100 patients with bowel cancer, after five years you would expect 70 to still be alive and 30 to have succumbed to the disease.
These statistics can’t tell us much about individual cases. But comparing five-year survival rates between large groups of patients after different cancer treatments can help clinicians make the often complex decisions about how best to treat their patients.
The likelihood of cancer coming back, or recurring, is influenced by many factors which can vary over time. For instance, approximately 30% of people with lung cancer develop a recurrent disease, even after treatment. On the other hand, breast cancer recurrence within two years of the initial diagnosis is approximately 15%. Within five years it drops to 10%. After ten, it falls below 2%.
These are generalisations though – recurrence rates can vary greatly depending on things such as what kind of cancer the patient has, how advanced it is, and whether it has spread.
Staying cancer-free
Princess Catherine says her focus now is to “stay cancer-free”. What might this involve?
How a cancer develops and whether it recurs can be influenced by things we can’t control, such as age, ethnicity, gender, genetics and hormones.
However, there are sometimes environmental factors we can control. That includes things like exposure to UV radiation from the sun, or inhaling carcinogens like tobacco.
Lifestyle factors also play a role. Poor diet and nutrition, a lack of exercise and excessive alcohol consumption can all contribute to cancer development.
Research estimates more than half of all cancers could potentially be prevented through regular screening and maintaining a healthy lifestyle (not to mention preventing other chronic conditions such as heart disease and diabetes).
Recommendations to reduce cancer risk are the same for everyone, not just those who’ve had treatment like Princess Catherine. They include not smoking, eating a nutritious and balanced diet, exercising regularly, cutting down on alcohol and staying sun smart.
Amali Cooray, PhD Candidate in Genetic Engineering and Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) ; John (Eddie) La Marca, Senior Research Officer, Blood Cells and Blood Cancer, WEHI (Walter and Eliza Hall Institute of Medical Research) , and Sarah Diepstraten, Senior Research Officer, Blood Cells and Blood Cancer Division, WEHI (Walter and Eliza Hall Institute of Medical Research)
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why We’re Called “10almonds”, And Other Questions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Avid coffee drinker so very interested in the results Also question Is there something that you could take or eat that would prevent the caffeine from stimulating the kidneys? I tried to drink decaf from morning to night not a good result! Thanks❞
That is a good question! The simple answer is “no” (but keep reading, because all is not lost)
There’s no way (that we yet know of) to proof the kidneys against the stimulating effect of caffeine. This is especially relevant because part of caffeine’s stimulating effect is noradrenergic, and that “ren” in the middle there? It’s about the kidneys. This is just because the adrenal gland is situated next to them (actually, it’s pretty much sitting on top of them), hence the name, but it does mean that the kidneys are about the hardest thing in the body to have not affected by caffeine.
However! The effects of caffeine in general can be softened a little with l-theanine (found in tea, or it can be taken as a supplement). It doesn’t stop it from working, but it makes the curve of the effect a little gentler, and so it can reduce some unwanted side effects.
You can read more about l-theanine here:
❝How to jump start a inactive metabolism and keep it going? THANKYOU❞
The good news is, if you’re alive, your metabolism is active (it never stops!). So, it may just need perking up a little.
As for keeping it going, well, that’s what we’re here for! We’re all in favor of healthy longevity.
We’ll do a main feature soon on what we can do to influence our metabolism in either direction, but to give some quick notes here:
- A lot of our metabolism is influenced by genes and is unalterable (without modifying our genes, anyway)
- Metabolism isn’t just one thing—it’s many. And sometimes, parts of our metabolism can be much quicker or slower than others.
- When people talk about wanting a “faster metabolism”, they’re usually referring to fat-burning, and that’s just a small part of the picture, but we understand that it’s a focal point for many.
There really is enough material for a whole main feature on metabolic tweaks, though, so watch this space!
❝Why the name “10 Almonds?” Is this recommended by the Doctor? A daily dosage? And, if so, why? Thanks! Please answer me…I truly want to know!❞
Almonds are very nutritionally dense, and for example 20g of almonds (so, about 20 almonds) would give a 100% daily dose of zinc, amongst other nutrients.
We also do like to think that we give our readers an easily digestible dose of condensed “nutrition” in the form of health information.
However! That’s not actually the reason at all. It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was circulating online! So, calling ourselves 10almonds was a bit of a nod to that story, but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
-
Skincare – by Caroline Hirons
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our skin is our largest organ, and it affects (and is affected by) most of what it contains. In other words, us.
So how do we look after this organ? Caroline Hirons lays it bare for us, in this very clear (and well-illustrated with many photos) book that gives a ground-upwards explanation of:
- Our skin’s layers and features and what they do
- The many ways our skin can be different from others
- What lifestyle factors to worry about (or not)
- What exactly the many kinds of skincare products do
- How to understand which ones are actually for our skin
- How to craft the ideal skincare routine for any individual
- What should go into a personalized skincare kit
Because, as it turns out, shockingly we can’t trust advertising. Not only is it advertising, but also, they don’t know us. What will be perfect for one person’s skin may ruin another’s, and labels can be very misleading.
A strength of this book is how Hirons demystifies all that, so we can ignore the claims and just know what a product will actually do, from its ingredients.
She also covers the changes that occur in various life processes, including puberty, pregnancy, menopause, and just plain aging. In other words, what to do when what’s been working suddenly doesn’t anymore.
Bottom line: this is a great book for anyone (though: especially those of us with female hormones) who wants to understand the skin you’re in and how to keep it well-nourished and glowingly healthy.
Click here to check out “Skincare” and take good care of yourself!
Share This Post
-
5 dental TikTok trends you probably shouldn’t try at home
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
TikTok is full of videos that demonstrate DIY hacks, from up-cycling tricks to cooking tips. Meanwhile, a growing number of TikTok videos offer tips to help you save money and time at the dentist. But do they deliver?
Here are five popular dental TikTok trends and why you might treat them with caution.
1. Home-made whitening solutions
Many TikTok videos provide tips to whiten teeth. These include tutorials on making your own whitening toothpaste using ingredients such as hydrogen peroxide, a common household bleaching agent, and baking soda (sodium bicarbonate).
In this video, the influencer says:
And then you’re going to pour in your hydrogen peroxide. There’s really no measurement to this.
But hydrogen peroxide in high doses is poisonous if swallowed, and can burn your gums, mouth and throat, and corrode your teeth.
High doses of hydrogen peroxide may infiltrate holes or microscopic cracks in your teeth to inflame or damage the nerves and blood vessels in the teeth, which can cause pain and even nerve death. This is why dental practitioners are bound by rules when we offer whitening treatments.
Sodium bicarbonate and hydrogen peroxide are among the components in commercially available whitening toothpastes. While these commercial products may be effective at removing surface stains, their compositions are carefully curated to keep your smile safe.
2. Oil pulling
Oil pulling involves swishing one tablespoon of sesame or coconut oil in your mouth for up to 20 minutes at a time. It has roots in Ayurvedic medicine, a traditional medicine practice that originates from the Indian subcontinent.
While oil pulling should be followed by brushing and flossing, I’ve had patients who believe oil pulling is a replacement for these practices.
There has been some research on the potential of oil pulling to treat gum disease or other diseases in the mouth. But overall, evidence that supports the effectiveness of oil pulling is of low certainty.
For example, studies that test the effectiveness of oil pulling have been conducted on school-aged children and people with no dental problems, and often measure dental plaque growth over a few days to a couple of weeks.
Chlorhexidine is an ingredient found in some commercially available mouthwashes.
In one study, people who rinsed with chlorhexidine mouthwash (30 seconds twice daily) developed less plaque on their teeth compared to those who undertook oil pulling for eight to 10 minutes.Ultimately, it’s unlikely you will experience measurable gain to your oral health by adding oil pulling to your daily routine. If you’re time-poor, you’re better off focusing on brushing your teeth and gums well alongside flossing.
3. Using rubber bands to fix gaps
This TikTok influencer shows his followers he closed the gaps between his front teeth in a week using cheap clear rubber bands.
But this person may be one of the lucky few to successfully use bands to close a gap in his teeth without any mishaps. Front teeth are slippery and taper near the gums into cone-shaped roots. This can cause bands to slide and disappear into the gums to surround the tooth roots, which can cause infections and pain.
If this happens, you may require surgery that involves cutting your gums to remove the bands. If the bands have caused an infection, you may lose the affected teeth. So it’s best to leave this sort of work to a dental professional trained in orthodontics.
4. Filing or cutting teeth to shape them
My teeth hurt just watching this video.
Cutting or filing teeth unnecessarily can expose the second, more sensitive tooth layer, called dentine, or potentially, the nerve and blood vessels inside the tooth. People undergoing this sort of procedure could experience anything from sensitive teeth through to a severe toothache that requires root canal treatment or tooth removal.
You may notice dentist drills spray water when cutting to protect your teeth from extreme heat damage. The drill in this video is dry with no water used to cool the heat produced during cutting.
It may also not be sterile. We like to have everything clean and sterile to prevent contaminated instruments used on one patient from potentially spreading an infection to another person.
Importantly, once you cut or file your teeth away, it’s gone forever. Unlike bone, hair or nails, our teeth don’t have the capacity to regrow.
5. DIY fillings
Many people on TikTok demonstrate filling cavities (holes) or replacing gaps between teeth with a material made from heated moulded plastic beads. DIY fillings can cause a lot of issues – I’ve seen this in my clinic first hand.
While we may make it look simple in dental surgeries, the science behind filling materials and how we make them stick to teeth to fill cavities is sophisticated.
Filling a cavity with the kind of material made from these beads will be as effective as using sticky tape on sand. Not to mention the cavity will continue to grow bigger underneath the untreated “filled” teeth.
I know it’s easy to say “see a dentist about that cavity” or “go to an orthodontist to fix that gap in your teeth you don’t like”, but it can be expensive to actually do these things. However if you end up requiring treatment to fix the issues caused at home, it may end up costing you much more.
So what’s the take-home message? Stick with the funny cat and dog videos on TikTok – they’re safer for your smile.
Arosha Weerakoon, Senior Lecturer and General Dentist, School of Dentistry, The University of Queensland
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Beyond Burger vs Beef Burger – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing the Beyond Burger to a grass-fed beef burger, we picked the Beyond Burger—but it was very close.
Why?
The macronutrient profiles of the two are almost identical, including the amount of protein, the amount of fat, and the amount of that fat that’s saturated.
Where they stand apart is in two ways:
1) Red meat is classed as a group 2A carcinogen
2) The Beyond Burger contains more sodium (about 1/5 of the daily allowance according to the AHA, or 1/4 of the daily allowance according to the WHO)Neither of those things are great, so how to decide which is worse?
• Cancer and heart disease are both killers, with heart disease claiming more victims.
• However, we do need some sodium to live, whereas we don’t need carcinogens to live.Tie-breaker: the sodium content in the Beyond Burger is likely to be offset by the fact that it’s a fully seasoned burger and will be eaten as-is, whereas the beef burger will doubtlessly have seasonings added before it’s eaten—which may cause it to equal or even exceed the salt content of the Beyond Burger.
The cancer risk for the beef burger, meanwhile, stays one-sided.
One thing’s for sure though: neither of them are exactly a cornerstone of a healthy diet, and either are best enjoyed as an occasional indulgence.
Some further reading:
• Lesser-Known Salt Risks
• Food Choices And Cancer Risk
• Hypertension: Factors Far More Relevant Than SaltDon’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Beat Osteoporosis with Exercise – by Dr. Karl Knopf
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of books about beating osteoporosis, and yet when it comes to osteoporosis exercises, it took us some work to find a good one. But, this one’s it!
A lot of books give general principles and a few sample exercises. This one, in contrast, gives:
- An overview of osteopenia and osteoporosis, first
- A brief overview of non-exercise osteoporosis considerations
- Principles for exercising a) to reduce one’s risk of osteoporosis b) if one has osteoporosis
- Clear explanations of about 150 exercises that fit both categories
This last item’s important, because a lot of popular advice is exercises that are only good for one or the other (given that a lot of things that strengthen a healthy person’s bones can break the bones of someone with osteoporosis), so having 150 exercises that are safe and effective in both cases, is a real boon.
That doesn’t mean you have to do all 150! If you want to, great. But even just picking and choosing and putting together a little program is good.
Bottom line: if you’d like a comprehensive guide to exercise to keep you strong in the face of osteoporosis, this is a great one.
Click here to check out Beat Osteoporosis With Exercise, and stay strong!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
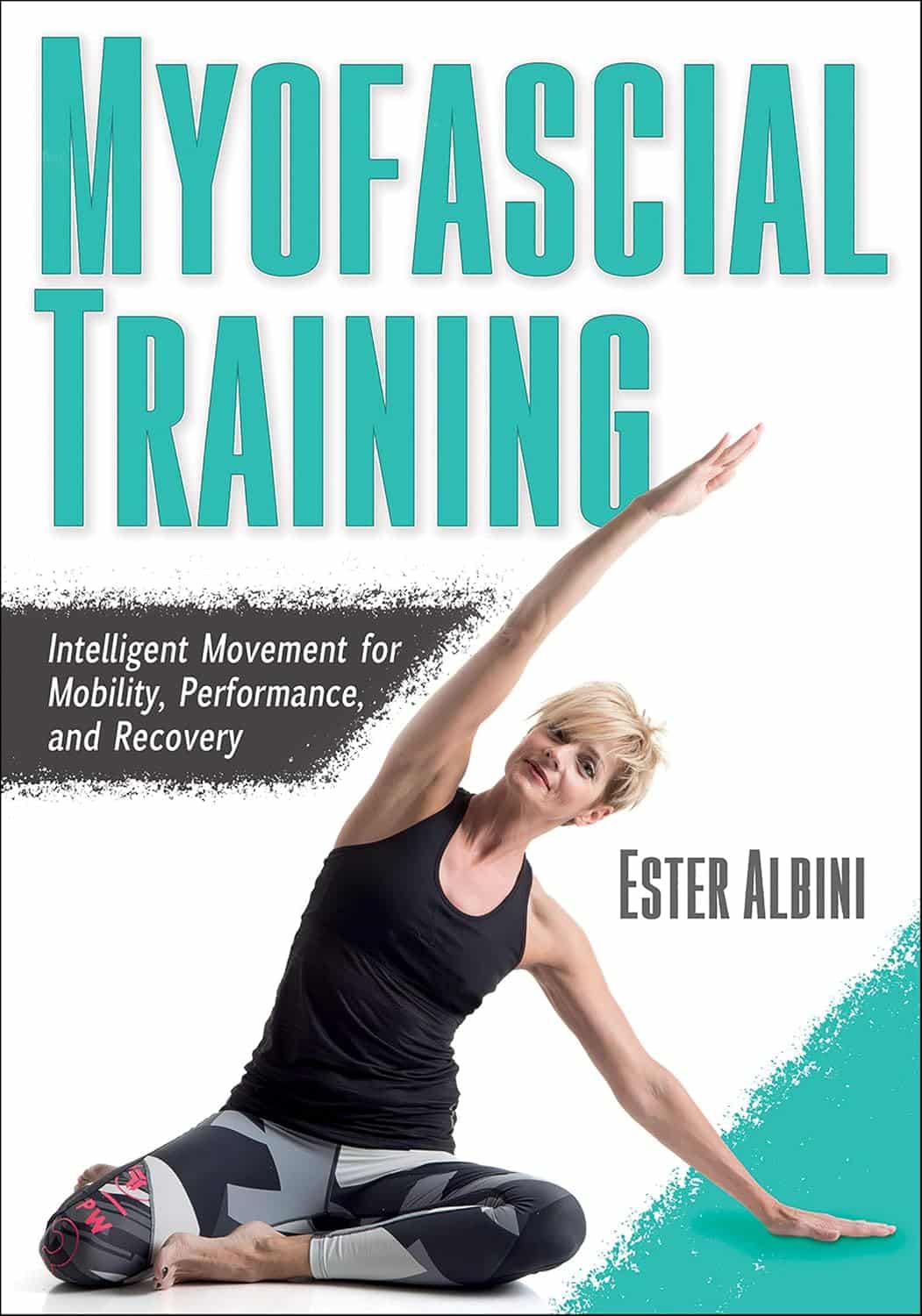
Myofascial Training – by Ester Albini
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fascia is an oft-forgotten part of the body—if something that is so ubiquitous and varied can be described as a single part. And yet, it arguably is—precisely because it is the connective tissue that holds everything else together, so by its nature, it’s ultimately a one-piece thing.
This “one-piece thing” is responsible for permitting us movement, and is also responsible for restricting our movement. As such, when it comes to mobility, we can stretch our muscles all day long and it won’t mean a thing if our fascia is stiff. And notably, fascia has a much slower turnover time (in terms of how quickly the body replaces it) than muscle, so fascia is almost always going to be the limiting factor.
Pilates instructor (with many certifications) Albini gives the reader the tools to loosen up that limiting factor. It’ll take time and consistency (it takes the body around 18 months to fully rebuild fascia, so that’s the timeframe for an ultimate “job done” to then just be maintained), but there are also some results to be enjoyed immediately, by virtue of myofascial release
In style, the book is half textbook, half workbook. She explains a lot of the anatomy and physiology of fascia (and does so very well). This book is, in this reviewer’s opinion, better than the usual go-to professional guidebook to fascia (i.e., for physiotherapists etc) that costs more than twice the price and is half as clear (the other book’s diagrams are unnecessarily abstract, the photos fuzzy, and the prose tedious). This book, in contrast, has very clear diagrams, hundreds of high-quality color photos, and excellent explanations that are aimed at the layperson, and/but aren’t afraid to get technical either; she just explains the technicalities well too.
The workbook side of things is a vast array of exercises to do, including for specific issues and to combat various lifestyle problems, as well as to just support general health and more mobility than most people think is possible for them.
Bottom line: if you’d like better mobility and have been neglecting your fascia (or have been a bit confused by it), this book is going to be your new best friend.
Click there to check out Myofascial Training, and free your body’s movements!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: