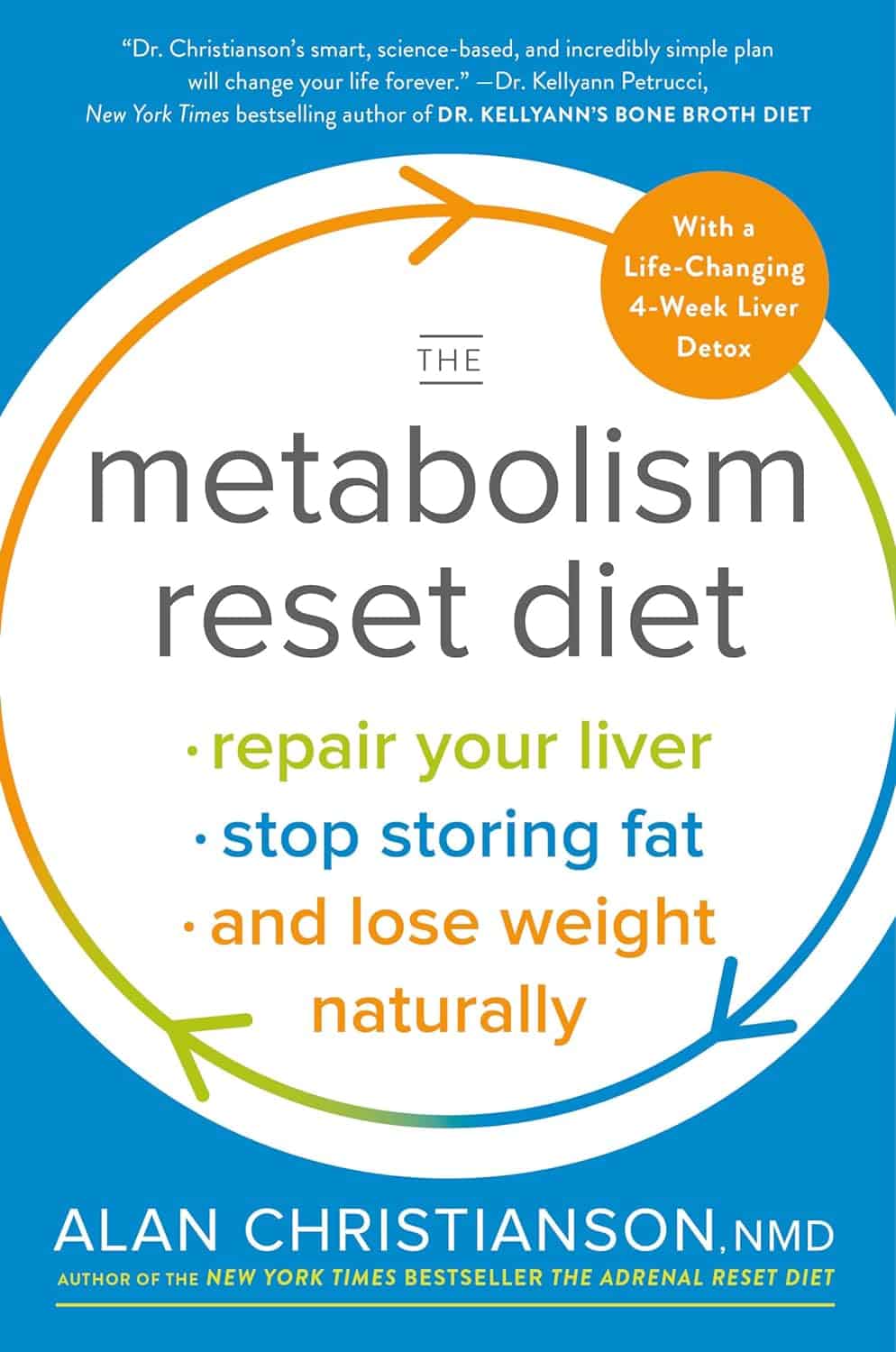
The Metabolism Reset Diet – by Alan Christianson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The liver is an incredible organ that does a very important job, but what’s not generally talked about is how we can help it… Beyond the obvious “try to not poison it too much with alcohol, tobacco, etc”. But what can we do that’s actually positive for it?
That’s what Alan Christianson offers in this book.
Now, usually when someone speaks of a “four week cleanse” as this book advertises on its front cover, it’s a lot of bunk. The liver cleanses itself, and the liver and kidneys between them (along with some other organs and processes) detoxify your body for you. No amount of celery juice will do that. However, this book does better than that:
What it’s about, is not really about trying to do a “detox” at all, so much as supporting your liver function by:
- Giving your liver what it needs to regenerate (mostly: protein)
- Not over-taxing your liver while it does so
The liver is a self-regenerating organ (the mythological story of Prometheus aside, here in real life it can regenerate up to 80% of itself, given the opportunity), so whatever the current state of your liver, it’s probably not too late to fix it.
Maybe you’ve been drinking a little too much, or maybe you’ve been taking some meds that have hobbled it a bit (some medications strain the liver rather), or maybe your diet hasn’t been great. Christianson invites you to draw a line under that, and move forwards:
The book gives an overview of the science involved, and explains about the liver’s role in metabolism (hence the promised weight loss benefits) and our dietary habits’ impact on liver function. This is about what we eat, and also about when we eat it, and how and when our body metabolizes that.
Christianson also provides meal ideas and recipes. If we’re honest (and we always are), the science/principles part of the book are worth a lot more than the meal-plan part of the book, though.
In short: a great book for understanding how the liver works and how we can help it do its job effectively.
Click here to check out “The Metabolism Reset Diet” on Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Counterintuitive Dos and Don’ts of Nail Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝I take a vitamin supplement for strengthening my nails (particularly one of my big toes!) – but they are running out! What do you recommend for strengthening nails? What is/are the key ingredient(s)?❞
Vitamin-wise, biotin (vitamin B7) is an underrated and very important one. As a bonus, it’s really good for your hair too (hair and nails being made of fundamentally the same “stuff”. Because it has exceptionally low toxicity, it can be taken up to 10,000% of the NRV, so if shopping for supplements, a high biotin content is better than a low one.
A lot of products marketed as for “skin, hair, and nails” focus on vitamins A and E, which are good for the skin but aren’t so relevant for nails.
Nutritionally, getting plenty of protein (whatever form you normally take it is fine) is also important since keratin (as nails are made of) is a kind of protein.
Outside of nutritional factors, a few other considerations:
- Testosterone strengthens nails, and declining testosterone levels (as experienced by most men over the age of 45) can result in weaker nails. So for men over 45 especially, a diet that favors testosterone (think foods rich in magnesium and zinc) is good.
- Because estrogen doesn’t do for women’s nails what testosterone does for men’s nails, increasing our magnesium and zinc intake won’t help our nails (but it’s still good for other things, including energy levels in the day and good sleep at night, and most people are deficient in magnesium anyway)
- Those of us who enjoy painted nails would do well to let our nails go without polish sometimes, as it can dry them out. And, acrylic nails are truly ruinous to nail health, as are gel nails (the kind that use a UV lamp to harden them—which is also bad for the skin)
- When nails are brittle, it can be tempting to soak them to reduce their brittleness. However, this is actually counterproductive, as the water will leech nutrients from the nails, and by the time you’ve been out of the footbath (for example) for about an hour, your nails will bemore brittle than before you soaked them.
- Use a moisturizing lotion or nail-oil instead—bonus if it contains biotin, keratin, and/or other helpful nutrients.
- Keep yourself hydrated, too! Hydration that comes to your nails from the inside will deliver nutrients, rather than removing them.
About those supplements: we don’t sell them (or anything else) but for your convenience, here are some great ones (this writer takes pretty much the same, just a different brand because I’m in a different country):
Magnesium Gummies (600mg) & Biotin Gummies (10,000µg)
Enjoy!
❝I was wondering whether there were very simple, clear bullet points or instructions on things to be wary of in Yoga.❞
That’s quite a large topic, and not one that lends itself well to being conveyed in bullet points, but first we’ll share the article you sent us when sending this question:
Tips for Avoiding Yoga Injuries
…and next we’ll recommend the YouTube channel @livinleggings, whose videos we feature here from time to time. She (Liv) has a lot of good videos on problems/mistakes/injuries to avoid.
Here’s a great one to get you started:
! Share This Post
-
Infrared-Reflecting Patches For Health?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Hi! I’ve been reading about LifeWave patches, would you recommend them?❞
For reference first, this is talking about these: LifeWave.com
Short answer: no
Longer answer: their main premise seems to be that the patches (subscription prices seem to start from about $100–$300 per month) reflect infrared energy back into your body, making you more energized and healthy.
Fun fact: aluminum foil reflects infrared energy (which we feel as heat), by the way, and that is why space blankets (of the kind used in emergencies and by some athletes) are made shiny like that, often with aluminized mylar.
We cannot comment too closely on the rest of the presented science of their products, as it seems quite unlike anything we’re accustomed to reading, and we were not able to make a lot of sense of it.
They do cite research papers to back their claims, including research conducted by the company’s founder and published via an open journal.
Many others are independent studies conducted by often the same researchers as each other, mostly experts in acupuncture and acupressure.
For the papers we looked at, the sample sizes were very small, but the conclusions were very positive.
They were published in a variety of journals, of which we cannot claim any prior knowledge (i.e:, they were not the peer-reviewed journals from which we cite most of our sources).
Also, none were registered with ClinicalTrials.gov.
To be on the safe side, their disclaimer does advise:
❝LifeWave products are only intended to maintain or encourage a general state of health or healthy activity and are not intended to diagnose, treat, cure, mitigate, or prevent any disease or medical condition of the body❞
They do have a Frequently Asked Questions page, which tells about ancient Egyptian use of colored glass, as well as more modern considerations including joining, ordering, their commissions system, binary commissions and matching bonuses, and “how to rank up in LifeWave” as well as a lot of information about subscribing as a preferred customer or a brand partner, opting in to their multi-level marketing opportunities.
Here’s what “Honest Brand Reviews” had to say:
Honest Brand Reviews | LifeWave Review
Our position:
We cannot honestly claim to understand their science, and thus naturally won’t actively recommend what we can’t speak for.
An expert’s position:
Since we couldn’t understand how this would work, here’s what Dr. Paul Knoepfler has to say about their flagship product, the LifeWave X39 patch:
LifeWave X39 stem cell patch story has holes
Take care!
Share This Post
-
Latest Alzheimer’s Prevention Research Updates
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Questions and Answers at 10almonds
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
This newsletter has been growing a lot lately, and so have the questions/requests, and we love that! In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I am now in the “aging” population. A great concern for me is Alzheimers. My father had it and I am so worried. What is the latest research on prevention?
One good thing to note is that while Alzheimer’s has a genetic component, it doesn’t appear to be hereditary per se. Still, good to be on top of these things, and it’s never too early to start with preventive measures!
You might like a main feature we did on this recently:
Share This Post
Related Posts
-
Lemon Balm For Stressful Times And More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Balm For The Mind: In More Ways Than One!
Lemon balm(Melissa officinalis) is quite unrelated to lemons, and is actually a closer relative to mint. It does have a lemony fragrance, though!
You’ll find it in a lot of relaxing/sleepy preparations, so…
What does the science say?
Relaxation
Lemon balm has indeed been found to be a potent anti-stress herb. Laboratories that need to test anything to do with stress generally create that stress in one of two main ways:
- If it’s not humans: a forced swimming test that’s a lot like waterboarding
- If it is humans: cognitive tests completed under time-pressure while multitasking
Consequently, studies that have set out to examine lemon balm’s anti-stress potential in humans, have often ended up also highlighting its potential as a cognitive enhancer, like this one in which…
❝Both active lemon balm treatments were generally associated with improvements in mood and/or cognitive performance❞
~ Dr. Anastasia Ossoukhova et al.
Read in full: Anti-Stress Effects of Lemon Balm-Containing Foods
And this one, which found…
❝The results showed that the 600-mg dose of Melissa ameliorated the negative mood effects of the DISS, with significantly increased self-ratings of calmness and reduced self-ratings of alertness.
In addition, a significant increase in the speed of mathematical processing, with no reduction in accuracy, was observed after ingestion of the 300-mg dose.❞
The appropriately named “DISS” is the Defined Intensity Stress Simulation we talked about.
Sleep
There’s a lot less research for lemon balm’s properties in this regard than for stress/anxiety, and it’s probably because sleep studies are much more expensive than stress studies.
It’s not for a lack of popular academic interest—for example, typing “Melissa officinalis” into PubMed (the vast library of studies we often cite from) autosuggests “Melissa officinalis sleep”. But alas, autosuggestions do not Randomized Controlled Trials make.
There are some, but they’re often small, old, and combined with other things, like this one:
This is interesting, because generally speaking there is little to no evidence that valerian actually helps sleep, so if this mixture worked, we might reasonably assume it was because of the lemon balm—but there’s an outside chance it could be that it only works in the presence of valerian (unlikely, but in science we must consider all possibilities).
Beyond that, we just have meta-reviews to work from, like this one that noted:
❝M. officinalis contains several phytochemicals such as phenolic acids, flavonoids, terpenoids, and many others at the basis of its pharmacological activities. Indeed, the plant can have antioxidant, anti-inflammatory, antispasmodic, antimicrobial, neuroprotective, nephroprotective, antinociceptive effects.
Given its consolidated use, M. officinalis has also been experimented with clinical settings, demonstrating interesting properties against different human diseases, such as anxiety, sleeping difficulties, palpitation, hypertension, depression, dementia, infantile colic, bruxism, metabolic problems, Alzheimer’s disease, and sexual disorders. ❞
You see why we don’t try to cover everything here, by the way!
But if you want to read this one in full, you can, at:
An Updated Review on The Properties of Melissa officinalis L.: Not Exclusively Anti-anxiety
Is it safe?
Lemon balm is generally recognized as safe, and/but please check with your doctor/pharmacist in case of any contraindications due to medicines you may be on or conditions you may have.
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon
Want to know your other options?
You might like our previous main features:
What Teas To Drink Before Bed (By Science!)
and
Safe Effective Sleep Aids For Seniors
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What does it mean to be transgender?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Transgender media coverage has surged in recent years for a wide range of reasons. While there are more transgender television characters than ever before, hundreds of bills are targeting transgender people’s access to medical care, sports teams, gender-specific public spaces, and other institutions.
Despite the increase in conversation about the transgender community, public confusion around transgender identity remains.
Read on to learn more about what it means to be transgender and understand challenges transgender people may face.
What does it mean to be transgender?
Transgender—or “trans”—is an umbrella term for people whose gender identity or gender expression does not conform to their sex assigned at birth. People can discover they are trans at any age.
Gender identity refers to a person’s inner sense of being a woman, a man, neither, both, or something else entirely. Trans people who don’t feel like women or men might describe themselves as nonbinary, agender, genderqueer, or two-spirit, among other terms.
Gender expression describes the way a person communicates their gender through their appearance—such as their clothing or hairstyle—and behavior.
A person whose gender expression doesn’t conform to the expectations of their assigned sex may not identify as trans. The only way to know for sure if someone is trans is if they tell you.
Cisgender—or “cis”—describes people whose gender identities match the sex they were assigned at birth.
How long have transgender people existed?
Being trans isn’t new. Although the word “transgender” only dates back to the 1960s, people whose identities defy traditional gender expectations have existed across cultures throughout recorded history.
How many people are transgender?
A 2022 Williams Institute study estimates that 1.6 million people over the age of 13 identify as transgender in the United States.
Is being transgender a mental health condition?
No. Conveying and communicating about your gender in a way that feels authentic to you is a normal and necessary part of self-expression.
Social and legal stigma, bullying, discrimination, harassment, negative media messages, and barriers to gender-affirming medical care can cause psychological distress for trans people. This is especially true for trans people of color, who face significantly higher rates of violence, poverty, housing instability, and incarceration—but trans identity itself is not a mental health condition.
What is gender dysphoria?
Gender dysphoria describes a feeling of unease that some trans people experience when their perceived gender doesn’t match their gender identity, or their internal sense of gender. A 2021 study of trans adults pursuing gender-affirming medical care found that most participants started experiencing gender dysphoria by the time they were 7.
When trans people don’t receive the support they need to manage gender dysphoria, they may experience depression, anxiety, social isolation, suicidal ideation, substance use disorder, eating disorders, and self-injury.
How do trans people manage gender dysphoria?
Every trans person’s experience with gender dysphoria is unique. Some trans people may alleviate dysphoria by wearing gender-affirming clothing or by asking others to refer to them by a new name and use pronouns that accurately reflect their gender identity. The 2022 U.S. Trans Survey found that nearly all trans participants who lived as a different gender than the sex they were assigned at birth reported that they were more satisfied with their lives.
Some trans people may also manage dysphoria by pursuing medical transition, which may involve taking hormones and getting gender-affirming surgery.
Access to gender-affirming medical care has been shown to reduce the risk of depression and suicide among trans youth and adults.
To learn more about the trans community, visit resources from the National Center for Transgender Equality, the Trevor Project, PFLAG, and Planned Parenthood.
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dandelion Greens vs Collard Greens – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dandelion greens to collard greens, we picked the dandelion greens.
Why?
Collard greens are great—they even beat kale in one of our previous “This or That” articles!—but dandelion greens simply pack more of a nutritional punch:
In terms of macros, dandelions have slightly more carbs (+3g/100g) for the same protein and fiber, and/but the glycemic index is equal (zero), so those carbs aren’t anything to worry about. Nobody is getting metabolic disease by getting their carbs from dandelion leaves. In short, we’re calling it a tie on macros, though it could nominally swing either way if you have an opinion (one way or the other) about the extra 3g of carbs.
In the category of vitamins, things are more exciting: dandelion greens have more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K, while collard greens have more vitamin B5. An easy and clear win for dandelions.
Looking at the minerals tells a similar story; dandelion greens have much more calcium, copper, iron, magnesium, phosphorus, potassium, and zinc, while collard greens have slightly more manganese. Another overwhelming win for dandelions.
One more category, polyphenols. We’d be here until next week if we listed all the polyphenols that dandelion greens have, but suffice it to say, dandelion greens have a total of 385.55mg/100g polyphenols, while collard greens have a total of 0.08mg/100g polyphenols. Grabbing a calculator, we see that this means dandelions have more than 4819x the polyphenol content that collard greens do.
So, “eat leafy greens” is great advice, but they are definitely not all created equal!
Let us take this moment to exhort: if you have any space at home where you can grow dandelions, grow them!
Not only are they great for pollinators, but also they beat the collard greens that beat kale. And you can have as much as you want, for free, right there.
Want to learn more?
You might like to read:
Collard Greens vs Kale – Which is Healthier?
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: