The Lost Art of Silence – by Sarah Anderson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From “A Room Of One’s Own” to “Silent Mondays”, from spiritual retreats to noise-cancelling headphones, this book covers the many benefits of silence—and a couple of downsides too.
In an age where most things are available at the touch of a button, a little peaceful solitude can come at quite a premium, but what it offers can effect all manner of physical changes, from reduced stress responses to increased neurogenesis (growing new brain cells).
The tone throughout is a combination of personal and pop-science, and it’s very motivating to find a little more space-between-the-things in life.
The book is best enjoyed in a quiet room.
Bottom line: if you get the feeling sometimes that you could rest and recover fully and properly if you could just find the downtime, this book will help you find exactly that.
Click here to check out the Lost Art of Silence, and find peace and strength in it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Anti-Viral Gut – by Dr. Robynne Chutkan
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people get a virus and feel terrible for a few days; other people get the same virus and die. Then there are some who never even get it at all despite being in close proximity with the other two. So, what’s the difference?
Dr. Robynne Chutkan outlines the case for the difference not being in the virus, but in the people. And nor is it a matter of mysterious fate, but rather, a matter of the different levels of defenses (or lack thereof) that we each have.
The key, she explains, is in our microbiome, and the specific steps to make sure that ours is optimized and ready to protect us. The book goes beyond “eat prebiotics and probiotics”, though, and goes through other modifiable factors, based on data from this pandemic and the last one a hundred years ago. We also learn about the many different kinds of bacteria that live in our various body parts (internal and external), because as it turns out, our gut microbiome (however important; hence the title) isn’t the only relevant microbiome when it comes to whether or not a given disease will take hold or be eaten alive on the way in.
The style is very polished—Dr. Chutkan is an excellent educator who makes her points clearly and comprehensibly without skimping on scientific detail.
Bottom line: if you’d like your chances of surviving any given virus season to not be left to chance, then this is a must-read book.
Click here to check out The Anti-Viral Gut, and make your body a fortress!
Share This Post
-
Heavy Metal Detox In A Pill?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previous discussed assorted approaches to “detoxing”:
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
Today we’re going to be looking at one we didn’t cover there, which is zeolite.
What is zeolite?
Zeolite is a mineral that occurs naturally and can also be synthesized, and it’s famous for absorbing other stuff from around it. Because of this property, it’s used in many things, including:
- Petrochemical catalysis
- Water treatment
- Nuclear waste reprocessing
- Cat litter
- Supplements (for detox purposes)
That’s, uh… An interesting list, isn’t it? So, we were curious as to whether this mineral that’s also used in fish tank filters is, in fact, overpriced gravel being sold to the gullible as a health supplement.
We had to do some digging on this one
Our journey didn’t start well, with this very dubious-looking paper being cited by a company selling zeolite supplements:
This immediately prompted two questions:
- Who is eating graphene?!* That stuff does not occur in nature (or at least; it hasn’t ever been found; the universe is a big place so it might exist elsewhere), has only relatively recently been synthesized, is very difficult to produce, is two-dimensional while being hard as diamonds, and exists only in truly tiny lab-made quantities worldwide. It would be orders of magnitude easier to find and eat uranium.
- Is this a reputable journal? Which question was easier to answer than the former one, and the answer is “no”; we hadn’t heard of this journal (ACTA Scientific), and neither it seems had most of the Internet, but we did find it on a list of predatory journals, here.
*The citation given in the above paper should by rights answer the question of who is eating graphene, since by rights they must have demonstrated it somehow, but it just doesn’t. Instead, it links to what it claims is a paper titled “Oxygenated Zeolite (Clinoptilite) Efficiently Removes Aluminum & Graphene Oxide”, but is in reality just someone’s blog post with a screenshot of an actual paper entitled “Novel, oxygenated clinoptilolite material efficiently removes aluminium from aluminium chloride-intoxicated rats in vivo”). Looking up this real paper in its real journal, it does not mention graphene.
All this to say: sometimes, unscrupulous people will just plain lie to you, which is why peer review is important, as is sourcing data from reputable journals. Which is what we do for you so that you don’t have to 🙂
It does, actually, work though (for heavy metal detox)
Notwithstanding the aforementioned bunk, we found this from a more reputable publisher:
❝In this study, we have presented clinical evidence supporting the use of an activated clinoptilolite (zeolite) suspension to safely and effectively increase the urinary excretion of potentially toxic heavy metals in healthy volunteers without negatively impacting the electrolyte profiles of the participants.
Significant increases in the urinary excretion of aluminum, antimony, arsenic, bismuth, cadmium, lead, mercury, nickel and tin were observed in the subjects participating in the two study groups as compared to placebo controls.❞
Also good for the gut and against inflammation
Specifically, it’s good for gut barrier integrity, i.e., against “leaky gut syndrome”:
❝Twelve weeks of zeolite supplementation exerted beneficial effects on intestinal wall integrity as indicated via decreased concentrations of the tight junction modulator zonulin.
This was accompanied by mild anti-inflammatory effects in this cohort of aerobically trained subjects.❞
May also be good against neurodegenerative diseases
If it is (which is plausible), it’ll probably because of removing heavy metals and improving gut barrier integrity—in other words, the things we just looked at in the two reputable peer-reviewed studies we examined above.
But the science is young for this one; here’s the current state of things:
Zeolite and Neurodegenerative Diseases
Is it safe?
Safety reviews have found it to be safe, for example:
Critical Review on Zeolite Clinoptilolite Safety and Medical Applications in vivo
However, if you are taking regular medications, we recommend checking with your pharmacist or doctor to ensure that zeolite will not also remove those medications from your system!
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
-
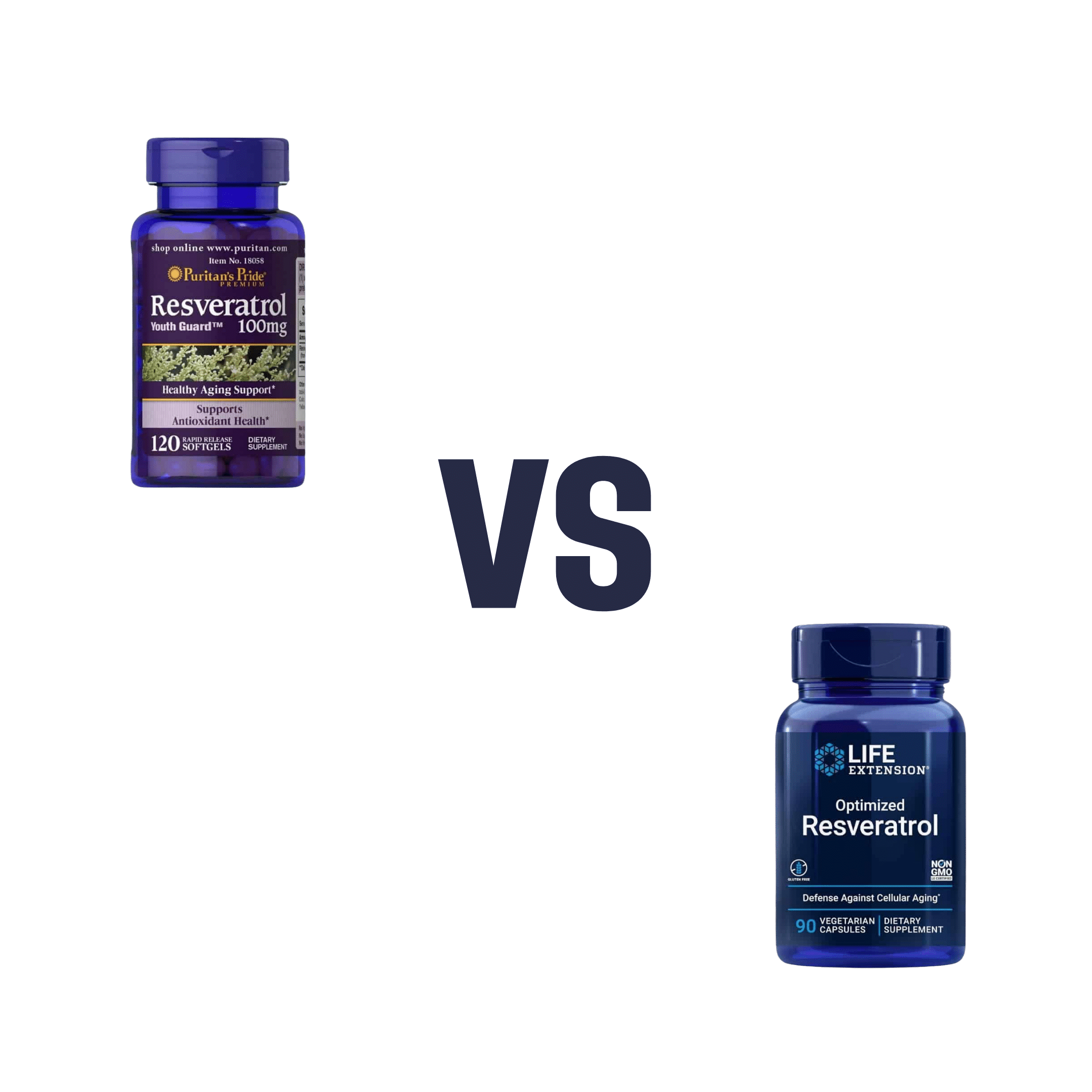
Puritans Pride Resveratrol vs Life Extension Resveratrol – Which is Healthier
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing Puritan’s Pride Resveratrol to Life Extension Resveratrol, we picked the Life Extension Resveratrol.
Why?
It contains not only more resveratrol per serving (250mg compared to Puritan’s Pride’s 100mg), but also contains other goodies too. Specifically, each capsule also contains:
- Quercetin (150mg)
- Grape & berry blend (85mg)
- Fisetin (10mg)
Whereas the Puritan’s Pride softgels? The other top ingredients are soybean oil and gelatin.
Want to check out the products for yourself? Here they are:
Puritan’s Pride Resveratrol | Life Extension Resveratrol
Want to know more about these supplements? Check out:
Resveratrol & Healthy Aging
Fight Inflammation & Protect Your Brain, With Quercetin
Berries & Other Polyphenol-rich Foods
Fisetin: The Anti-Aging AssassinEnjoy!
Share This Post
Related Posts
-
Trout vs Haddock – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing trout to haddock, we picked the trout.
Why?
It wasn’t close.
In terms of macros, trout has more protein and more fat, although the fat is mostly healthy (some saturated though, and trout does have more cholesterol). This category could be a win for either, depending on your priorities. But…
When it comes to vitamins, trout has a lot more of vitamins A, B1, B2, B3, B5, B6, B12, C, D, and E, while haddock is not higher in any vitamins.
In the category of minerals, trout has more calcium, copper, iron, magnesium, potassium, and zinc, while haddock has slightly more selenium. Given that a 10oz portion of trout already contains 153% of the RDA of selenium, however, the same size portion of haddock having 173% of the RDA isn’t really a plus for haddock (especially as selenium can cause problems if we get too much). Oh, and haddock is also higher in sodium, but in industrialized countries, most people most of the time need less of that, not more.
On balance, the overwhelming nutritional density of trout wins the day.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: It Makes Quite A Difference!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What Macronutrient Balance Is Right For You?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝I want to learn more about macros. Can you cover that topic?❞
That’s a little broader than we usually go for, given the amount of space we have, but let’s give it a go!
Macronutrients, or “macros”, are the nutrients that we typically measure in grams rather than milligrams or micrograms, and are:
- Carbohydrates
- …and what kinds, of which usually the focus is on how much is sugars as opposed to more complex carbs that take longer to break down. See also: Should You Go Light Or Heavy On Carbs?
- …and of the sugars, the interested may further categorize them into sucrose, fructose, etc. See also: Which Sugars Are Healthier, And Which Are Just The Same?
- Proteins
- …of which, the amino acid make-up is generally considered a matter of micronutrients. See also: Protein: How Much Do We Need, Really?
- Fats
- …and what kinds, i.e. monounsaturated vs polyunsaturated vs saturated. See also: Saturated Fat: What’s The Truth?
- …and then the interested may further categorize them for their fatty acids / triglycerides profile, etc. See also: What Omega-3 Fatty Acids Really Do For Us
- Fiber
- …which often gets ignored by people counting macros, as “stuff that doesn’t do anything”, despite it in fact being very important for health. See also: Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Water
- …which again tends to get disregarded but is very arguably a critical macronutrient. See also: Busting The Myth of “Eight Glasses Of Water A Day”
In terms of how much we need of each, you can read more in the above-linked articles, but:
- General scientific consensus is we need plenty of fiber (30 or 40g per day is good) and water (highly dependent on climate and activity), and there’s a clear minimum requisite for protein (usually put at around 1g of protein per day per 1kg of body weight).
- There is vigorous debate in the general health community about what the best ratio of carbs to fat is.
The reality is that humans are quite an adaptable species, and while we absolutely do need at least some of both (carbohydrates and fats), we can play around with the ratios quite a bit, provided we don’t get too extreme about it.
While some influence is social and often centered around weight loss (see for example keto which seeks to minimize carbs, and volumetrics, which seeks maximise volume-to-calorie ratio, which de facto tends to minimize fats), some of what drives us to lean one way or the other will be genetics, too—dependent on what our ancestors ate more or less of.
Writer’s example: my ancestors could not grow much grain (or crops in general) where they were, so they got more energy from such foods as whale and seal fat (with protein coming more from reindeer). Now, biology is not destiny, and I personally enjoy a vegan diet, but my genes are probably why I am driven to get most of my daily calories from fat (of which, a lot of fatty nuts (don’t tell almonds, but I prefer walnuts and cashews) and healthy oils such as olive oil, avocado oil, and coconut oil).
However! About that adaptability. Provided we make changes slowly, we can usually adjust our diet to whatever we want it to be, including whether we get our energy more from carbs or fats. The reason we need to make changes slowly is because our gut needs time to adjust. For example, if your vegan writer here were to eat her ancestrally-favored foods now, I’d be very ill, because my gut microbiome has no idea what to do with animal products anymore, no matter what genes I have. In contrast, if an enthusiastic enjoyer of a meat-heavy diet were to switch to my fiber-rich diet overnight, they’d be very ill.
So: follow your natural inclinations, make any desired changes slowly, and if in doubt, it’s hard to go wrong with enjoying carbs and fats in moderation.
Learn more: Intuitive Eating Might Not Be What You Think
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
- Carbohydrates
-
Vision for Life, Revised Edition – by Dr. Meir Schneider
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The “ten steps” would be better called “ten exercises”, as they’re ten things that one can (and should) continue to do on an ongoing basis, rather than steps to progress through and then forget about.
We can’t claim to have tested the ten exercises for improvement (this reviewer has excellent eyesight and merely hopes to maintain such as she gets older) but the rationale is compelling, and the public testimonials abundant.
Dr. Schneider also talks about improving and correcting errors of refraction—in other words, doing the job of any corrective lenses you may currently be using. While he doesn’t claim miracles, it turns out there is a lot that can be done for common issues such as near-sightedness and far-sightedness, amongst others.
There’s a large section on managing more chronic pathological eye conditions than this reviewer previously knew existed; in some cases it’s a matter of making sure things don’t get worse, but in many others, there’s a recurring of theme of “and here’s an exercise for correcting that”.
The writing style is a little more “narrative prose” than we’d have liked, but the quality of the content more than makes up for any style preference issues.
Bottom line: the human body is a highly adaptive organism, and sometimes it just needs a little help to correct itself. This book can help with that.
Click here to check out Vision for Life, and take good care of yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: