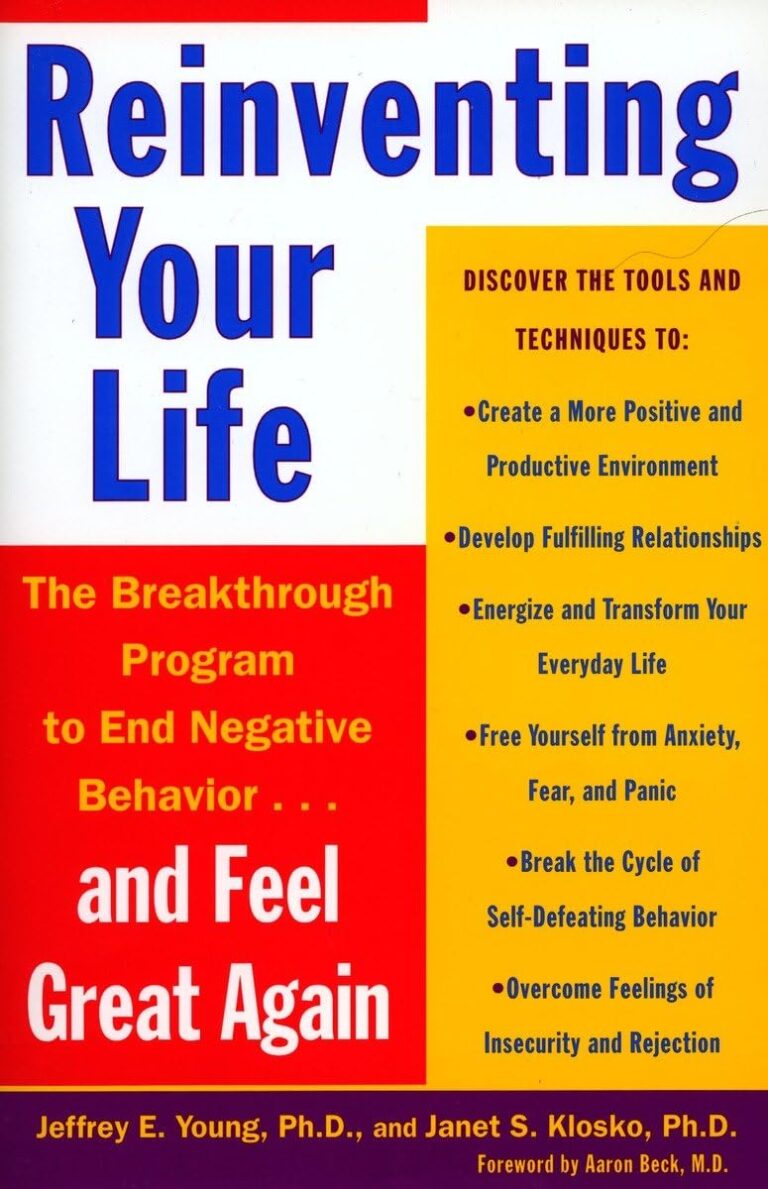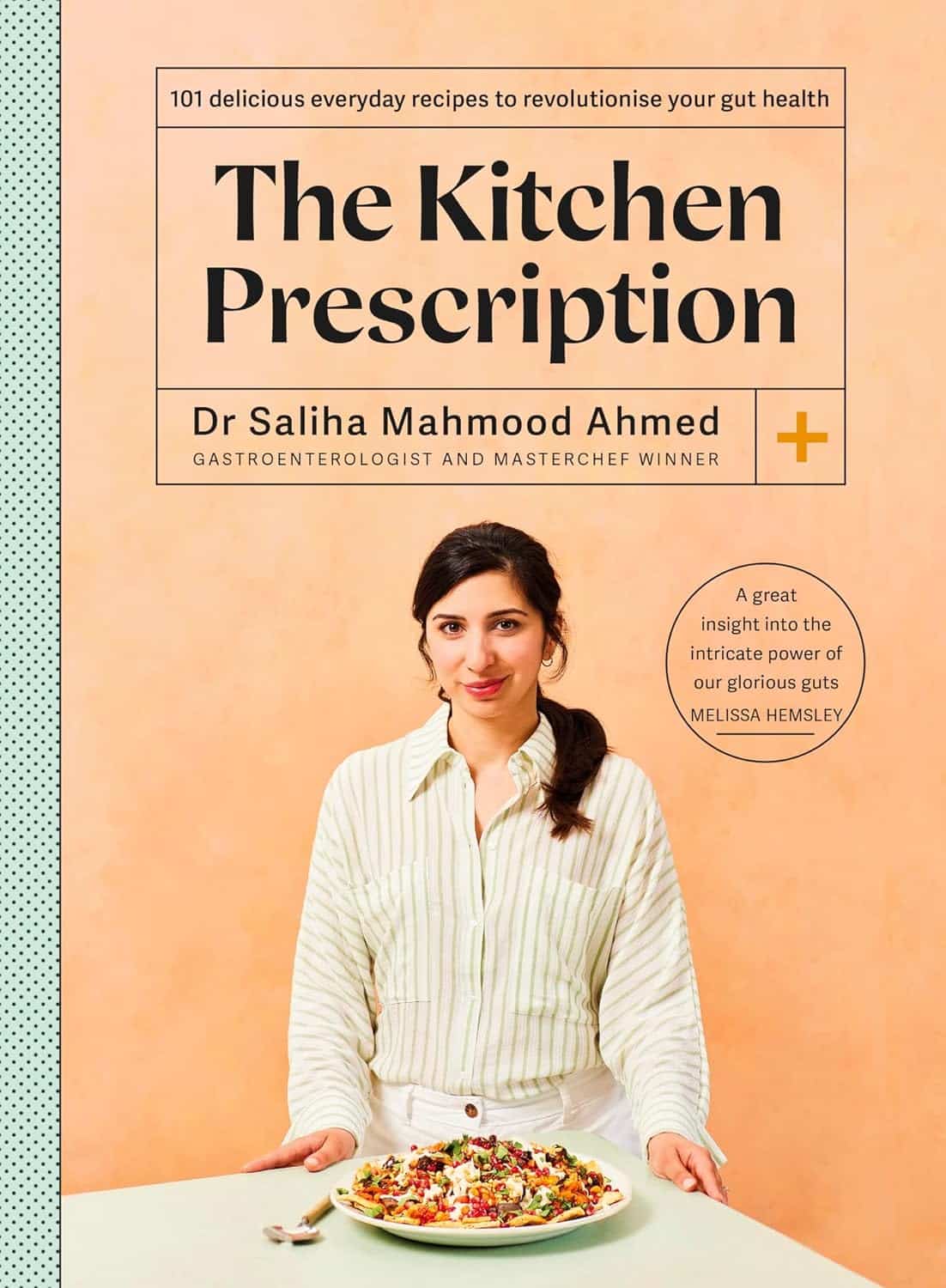
The Kitchen Prescription – by Saliha Mahmood Ahmed
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the biggest challenges facing anyone learning to cook more healthily, is keeping it tasty. What to cook when your biggest comfort foods all contain things you “should” avoid?
Happily for us, Dr. Ahmed is here with a focus on comfort food that’s good for your gut health. It’s incidentally equally good for the heart and good against diabetes… but Dr. Ahmed is a gastroenterologist, so that’s where she’s coming from with these.
There’s a wide range of 101 recipes here, including many tagged vegetarian, vegan, and/or gluten-free, as appropriate.
While this is not a vegetarian cookbook, Dr. Ahmed does consider the key components of a good diet to be, in order of quantity that should be consumed:
- Fruits and vegetables
- Whole grains
- Legumes
- Pulses
- Nuts and seeds
…and as such, the recipes are mostly plant-based.
The recipes are from all around the world, and/but the ingredients are mostly things that are almost universal. In the event that something might be hard-to-get, she suggests an appropriate substitution.
The recipes are straightforward and clear, as well as being beautifully illustrated.
All in all, a fine addition to anyone’s kitchen!
Get your copy of The Kitchen Prescription from Amazon today!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
No, your aches and pains don’t get worse in the cold. So why do we think they do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s cold and wet outside. As you get out of bed, you can feel it in your bones. Your right knee is flaring up again. That’ll make it harder for you to walk the dog or go to the gym. You think it must be because of the weather.
It’s a common idea, but a myth.
When we looked at the evidence, we found no direct link between most common aches and pains and the weather. In the first study of its kind, we found no direct link between the temperature or humidity with most joint or muscle aches and pains.
So why are so many of us convinced the weather’s to blame? Here’s what we think is really going on.
fongbeerredhot/Shutterstock Weather can be linked to your health
The weather is often associated with the risk of new and ongoing health conditions. For example, cold temperatures may worsen asthma symptoms. Hot temperatures increase the risk of heart problems, such as arrhythmia (irregular heartbeat), cardiac arrest and coronary heart disease.
Many people are also convinced the weather is linked to their aches and pains. For example, two in every three people with knee, hip or hand osteoarthritis say cold temperatures trigger their symptoms.
Musculoskeletal conditions affect more than seven million Australians. So we set out to find out whether weather is really the culprit behind winter flare-ups.
What we did
Very few studies have been specifically and appropriately designed to look for any direct link between weather changes and joint or muscle pain. And ours is the first to evaluate data from these particular studies.
We looked at data from more than 15,000 people from around the world. Together, these people reported more than 28,000 episodes of pain, mostly back pain, knee or hip osteoarthritis. People with rheumatoid arthritis and gout were also included.
We then compared the frequency of those pain reports between different types of weather: hot or cold, humid or dry, rainy, windy, as well as some combinations (for example, hot and humid versus cold and dry).
Bad back on a cold day? We wanted to know if the weather was really to blame. Pearl PhotoPix/Shutterstock What we found
We found changes in air temperature, humidity, air pressure and rainfall do not increase the risk of knee, hip or lower back pain symptoms and are not associated with people seeking care for a new episode of arthritis.
The results of this study suggest we do not experience joint or muscle pain flare-ups as a result of changes in the weather, and a cold day will not increase our risk of having knee or back pain.
In order words, there is no direct link between the weather and back, knee or hip pain, nor will it give you arthritis.
It is important to note, though, that very cold air temperatures (under 10°C) were rarely studied so we cannot make conclusions about worsening symptoms in more extreme changes in the weather.
The only exception to our findings was for gout, an inflammatory type of arthritis that can come and go. Here, pain increased in warmer, dry conditions.
Gout has a very different underlying biological mechanism to back pain or knee and hip osteoarthritis, which may explain our results. The combination of warm and dry weather may lead to increased dehydration and consequently increased concentration of uric acid in the blood, and deposition of uric acid crystals in the joint in people with gout, resulting in a flare-up.
Why do people blame the weather?
The weather can influence other factors and behaviours that consequently shape how we perceive and manage pain.
For example, some people may change their physical activity routine during winter, choosing the couch over the gym. And we know prolonged sitting, for instance, is directly linked to worse back pain. Others may change their sleep routine or sleep less well when it is either too cold or too warm. Once again, a bad night’s sleep can trigger your back and knee pain.
Likewise, changes in mood, often experienced in cold weather, trigger increases in both back and knee pain.
So these changes in behaviour over winter may contribute to more aches and pains, and not the weather itself.
Believing our pain will feel worse in winter (even if this is not the case) may also make us feel worse in winter. This is known as the nocebo effect.
When it’s cold outside, we may be less active. Anna Nass/Shutterstock What to do about winter aches and pains?
It’s best to focus on risk factors for pain you can control and modify, rather than ones you can’t (such as the weather).
You can:
- become more physically active. This winter, and throughout the year, aim to walk more, or talk to your health-care provider about gentle exercises you can safely do at home, with a physiotherapist, personal trainer or at the pool
- lose weight if obese or overweight, as this is linked to lower levels of joint pain and better physical function
- keep your body warm in winter if you feel some muscle tension in uncomfortably cold conditions. Also ensure your bedroom is nice and warm as we tend to sleep less well in cold rooms
- maintain a healthy diet and avoid smoking or drinking high levels of alcohol. These are among key lifestyle recommendations to better manage many types of arthritis and musculoskeletal conditions. For people with back pain, for example, a healthy lifestyle is linked with higher levels of physical function.
Manuela Ferreira, Professor of Musculoskeletal Health, Head of Musculoskeletal Program, George Institute for Global Health and Leticia Deveza, Rheumatologist and Research Fellow, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Does Music Really Benefit The Brain?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Is it actually beneficial for the brain to listen to music, or is it just in line with any relaxing activity? And what kind of music is most beneficial❞
The short answer, first of all, is that it is indeed beneficial.
One reason for this without having to get very deep into it, is that a very important thing for general brain health is using it, and that means lighting up all areas of your brain.
Now, we all lead different lives and thus different parts of our brains will get relatively more resources than others depending on what we do with them, and that’s ok.
For example, if you were to scan this writer’s polyglot brain, you’d surely find overdevelopment in areas associated with language use and verbal memory, but if you were to scan a taxi-driver’s brain, then it’d be spatial reasoning and spatial memory that’s overpowered, and for a visual artist, it may be visual processing and creativity that’s enhanced. A musician’s brain? Fine motor skills, auditory processing, auditory memory.
Now, for those of us who aren’t musicians, how then can we light up areas associated with music? By listening to music, of course. It won’t give us the fine motor skills of a concert violinist, but the other areas we mentioned will get a boost.
See also: How To Engage Your Whole Brain ← this covers music too, but it’s about (as the title suggests) the whole brain, so check it out and see if there are any areas you’ve been neglecting!
There are other benefits too, though, including engaging our parasympathetic nervous system, which is good for our heart, gut, brain, and general health—especially if we sing or hum along to the music:
The Science Of Sounds ← this also covers the science (yes, science) of mantra meditation vs music
As for “and what kind of music is most beneficial”, we’d hypothesize that a variety is best, just like with food!
However, there are some considerations to bear in mind, with science to support them. For example…
About tempo:
❝EEG analysis revealed significant changes in brainwave signals across different frequency bands under different tempi.
For instance, slow tempo induced higher Theta and Alpha power in the frontal region, while fast tempo increased Beta and Gamma band power.
Moreover, fast tempo enhanced the average connectivity strength in the frontal, temporal, and occipital regions, and increased phase synchrony value (PLV) between the frontal and parietal regions.❞
Read in full: Music tempo modulates emotional states as revealed through EEG insights
And if you’re wondering about those different brainwave bands, check out:
- How to get many benefits of sleep, while awake! Non-Sleep Deep Rest: A Neurobiologist’s Take ← although it’s not in the title, this does also cover the different brain wave bands
- Alpha, beta, theta: what are brain states and brain waves? And can we control them?
Additionally, if you just want science-backed relaxation, the following 8-minute soundscape was developed by sound technicians working with a team of psychologists and neurologists.
It’s been clinically tested, and found to have a much more relaxing effect (in objective measures of lowering heart rate and lowering cortisol levels, as well as in subjective self-reports) than merely “relaxing music”.
Try it and see for yourself:
Click Here If The Embedded Video Doesn’t Load Automatically!
For much deeper dive into the effect of music on the brain, check out this book we reviewed a while back, by an accomplished musician and neuroscientist (that’s one person, who is both things):
This Is Your Brain on Music – by Dr. Daniel Levitin
Enjoy!
And now for a bonus item…
A s a bit of reader feedback prompted some interesting thoughts:
❝You erred on the which is better section. Read this carefully :Looking at minerals, grapes have more calcium, copper, iron, magnesium, phosphorus, selenium, and zinc, while grapes have more potassium and manganese. A clear win for strawberries here.❞
You’re quite right; thank you for pointing it out, and kindly pardon the typo, which has now been corrected!
The reason for the mistake was because when I (writer responsible for it here, hi) was writing this, I had the information for both fruits in front of me, but the information for grapes was on the right in my field of vision, so I errantly put it on the right on the page, too, while also accidentally crediting strawberries’ minerals to grapes, since strawberries’ data was on the left in my field a vision.
The reason for explaining this: it’s a quirky, very human way to err, in an era when a lot of web content is AI-generated with very different kinds of mistakes (usually because AI is very bad at checking sources, so will confidently state something as true despite the fact that the source was The Onion, or Clickhole, or someone’s facetiously joking answer on Quora, for example).
All in all, while we try to not make typos, we’d rather such human errors than doing like an AI and confidently telling you that Amanita phalloides mushrooms are a rich source of magnesium, and also delicious (they are, reportedly, but they are also the most deadly mushroom on the face of the Earth, also known as the Death Cap mushroom).
In any case, here’s the corrected version of the grapes vs strawberries showdown:
Grapes vs Strawberries – Which is Healthier?
Enjoy!
Share This Post
-
How can I stop overthinking everything? A clinical psychologist offers solutions
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As a clinical psychologist, I often have clients say they are having trouble with thoughts “on a loop” in their head, which they find difficult to manage.
While rumination and overthinking are often considered the same thing, they are slightly different (though linked). Rumination is having thoughts on repeat in our minds. This can lead to overthinking – analysing those thoughts without finding solutions or solving the problem.
It’s like a vinyl record playing the same part of the song over and over. With a record, this is usually because of a scratch. Why we overthink is a little more complicated.
We’re on the lookout for threats
Our brains are hardwired to look for threats, to make a plan to address those threats and keep us safe. Those perceived threats may be based on past experiences, or may be the “what ifs” we imagine could happen in the future.
Our “what ifs” are usually negative outcomes. These are what we call “hot thoughts” – they bring up a lot of emotion (particularly sadness, worry or anger), which means we can easily get stuck on those thoughts and keep going over them.
However, because they are about things that have either already happened or might happen in the future (but are not happening now), we cannot fix the problem, so we keep going over the same thoughts.
Who overthinks?
Most people find themselves in situations at one time or another when they overthink.
Some people are more likely to ruminate. People who have had prior challenges or experienced trauma may have come to expect threats and look for them more than people who have not had adversities.
Deep thinkers, people who are prone to anxiety or low mood, and those who are sensitive or feel emotions deeply are also more likely to ruminate and overthink.
We all overthink from time to time, but some people are more prone to rumination.
BĀBI/UnsplashAlso, when we are stressed, our emotions tend to be stronger and last longer, and our thoughts can be less accurate, which means we can get stuck on thoughts more than we would usually.
Being run down or physically unwell can also mean our thoughts are harder to tackle and manage.
Acknowledge your feelings
When thoughts go on repeat, it is helpful to use both emotion-focused and problem-focused strategies.
Being emotion-focused means figuring out how we feel about something and addressing those feelings. For example, we might feel regret, anger or sadness about something that has happened, or worry about something that might happen.
Acknowledging those emotions, using self-care techniques and accessing social support to talk about and manage your feelings will be helpful.
The second part is being problem-focused. Looking at what you would do differently (if the thoughts are about something from your past) and making a plan for dealing with future possibilities your thoughts are raising.
But it is difficult to plan for all eventualities, so this strategy has limited usefulness.
What is more helpful is to make a plan for one or two of the more likely possibilities and accept there may be things that happen you haven’t thought of.
Think about why these thoughts are showing up
Our feelings and experiences are information; it is important to ask what this information is telling you and why these thoughts are showing up now.
For example, university has just started again. Parents of high school leavers might be lying awake at night (which is when rumination and overthinking is common) worrying about their young person.
Think of what the information is telling you.
TheVisualsYouNeed/ShutterstockKnowing how you would respond to some more likely possibilities (such as they will need money, they might be lonely or homesick) might be helpful.
But overthinking is also a sign of a new stage in both your lives, and needing to accept less control over your child’s choices and lives, while wanting the best for them. Recognising this means you can also talk about those feelings with others.
Let the thoughts go
A useful way to manage rumination or overthinking is “change, accept, and let go”.
Challenge and change aspects of your thoughts where you can. For example, the chance that your young person will run out of money and have no food and starve (overthinking tends to lead to your brain coming up with catastrophic outcomes!) is not likely.
You could plan to check in with your child regularly about how they are coping financially and encourage them to access budgeting support from university services.
Your thoughts are just ideas. They are not necessarily true or accurate, but when we overthink and have them on repeat, they can start to feel true because they become familiar. Coming up with a more realistic thought can help stop the loop of the unhelpful thought.
Accepting your emotions and finding ways to manage those (good self-care, social support, communication with those close to you) will also be helpful. As will accepting that life inevitably involves a lack of complete control over outcomes and possibilities life may throw at us. What we do have control over is our reactions and behaviours.
Remember, you have a 100% success rate of getting through challenges up until this point. You might have wanted to do things differently (and can plan to do that) but nevertheless, you coped and got through.
So, the last part is letting go of the need to know exactly how things will turn out, and believing in your ability (and sometimes others’) to cope.
What else can you do?
A stressed out and tired brain will be more likely to overthink, leading to more stress and creating a cycle that can affect your wellbeing.
So it’s important to manage your stress levels by eating and sleeping well, moving your body, doing things you enjoy, seeing people you care about, and doing things that fuel your soul and spirit.
Find ways to manage your stress levels.
antoniodiaz/ShutterstockDistraction – with pleasurable activities and people who bring you joy – can also get your thoughts off repeat.
If you do find overthinking is affecting your life, and your levels of anxiety are rising or your mood is dropping (your sleep, appetite and enjoyment of life and people is being negatively affected), it might be time to talk to someone and get some strategies to manage.
When things become too difficult to manage yourself (or with the help of those close to you), a therapist can provide tools that have been proven to be helpful. Some helpful tools to manage worry and your thoughts can also be found here.
When you find yourself overthinking, think about why you are having “hot thoughts”, acknowledge your feelings and do some future-focused problem solving. But also accept life can be unpredictable and focus on having faith in your ability to cope.
Kirsty Ross, Associate Professor and Senior Clinical Psychologist, Massey University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
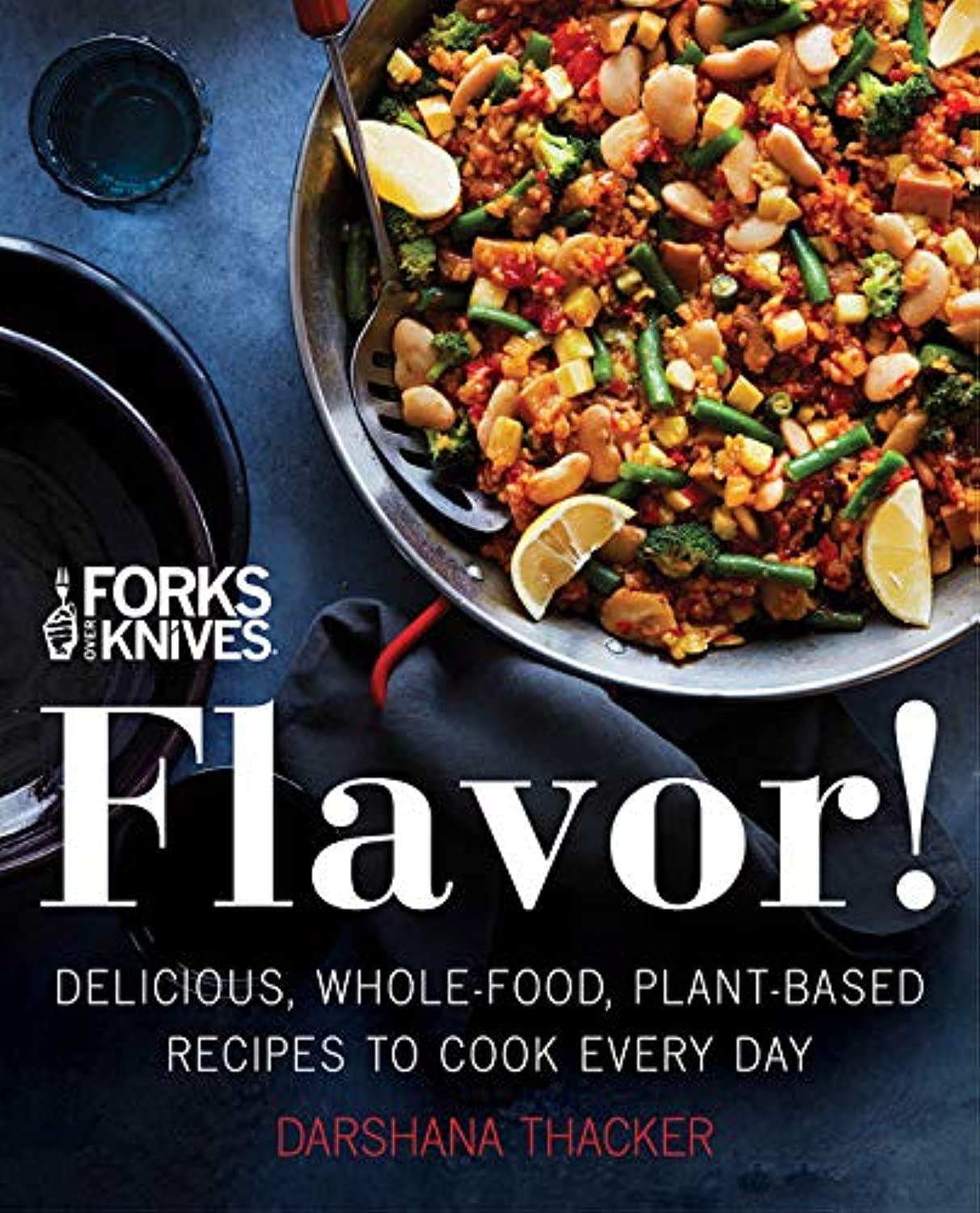
Forks Over Knives: Flavor! – by Darshana Thacker
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s important to not have to choose too much between health and flavor, because the outcome will never be a good one, either for your health or your happiness. And what’s bad for your happiness will ultimately not work out and thus will be bad for your general health, so, the question becomes: how to get both?
This book handles that nicely, delivering plant-based dishes that are also incidentally oil-free, and also either gluten-free or else there’s an obvious easy substitution to make it such. The flavor here comes from the ingredients as a whole, including the main ingredients as well as seasonings.
On the downside, occasionally those ingredients may be a little obscure if you don’t live in, say, San Francisco, and the ingredients weren’t necessarily chosen for cooking on a budget, either.
However, in most cases for most people it will, at worse, inspire you to try using an ingredient you don’t usually use—so that’s a good result.
The recipes are very clear and easy to follow, although not all are illustrated, and the “ready in…” times are about as accurate as they are for any cookbook, that is to say, it’s the time in which it conceivably can be done if (like the author, a head chef) you have a team of sous-chefs who have done a bunch of prep for you (e.g. sweet potato does not normally come in ½” dice; it comes in sweet potatoes) and laid everything out in little bowls mise-en-place style, and also you know the procedure well enough to not have to stop, hesitate, check anything, wash anything, wait for water to boil or anything else to heat up, or so forth. In other words, if you’re on your own in your home kitchen with normal domestic appliances, it’s going to take a little longer than for a professional in a professional kitchen with professional help.
But don’t let that detract from the honestly very good recipes.
Bottom line: if you’d like to level-up your plant-based cooking, this will definitely make your dishes that bit better!
Click here to check out Forks Over Knives: Flavor!, and dig in!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What is pathological demand avoidance – and how is it different to ‘acting out’?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Charlie” is an eight-year-old child with autism. Her parents are worried because she often responds to requests with insults, aggression and refusal. Simple demands, such as being asked to get dressed, can trigger an intense need to control the situation, fights and meltdowns.
Charlie’s parents find themselves in a constant cycle of conflict, trying to manage her and their own reactions, often unsuccessfully. Their attempts to provide structure and consequences are met with more resistance.
What’s going on? What makes Charlie’s behaviour – that some are calling “pathological demand avoidance” – different to the defiance most children show their parents or carers from time-to-time?
What is pathological demand avoidance?
British developmental psychologist Elizabeth Newson coined the term “pathological demand avoidance” (commonly shortened to PDA) in the 1980s after studying groups of children in her practice.
A 2021 systematic review noted features of PDA include resistance to everyday requests and strong emotional and behavioural reactions.
Children with PDA might show obsessive behaviour, struggle with persistence, and seek to control situations. They may struggle with attention and impulsivity, alongside motor and coordination difficulties, language delay and a tendency to retreat into role play or fantasy worlds.
PDA is also known as “extreme demand avoidance” and is often described as a subtype of autism. Some people prefer the term persistent drive for autonomy or pervasive drive for autonomy.
What does the evidence say?
Every clinician working with children and families recognises the behavioural profile described by PDA. The challenging question is why these behaviours emerge.
PDA is not currently listed in the two diagnostic manuals used in psychiatry and psychology to diagnose mental health and developmental conditions, the current Diagnostic and Statistical Manual of Mental Disorders (DSM-5) and the World Health Organization’s International Classification of Diseases (ICD-11).
Researchers have reported concerns about the science behind PDA. There are no clear theories or explanations of why or how the profile of symptoms develop, and little inclusion of children or adults with lived experience of PDA symptoms in the studies. Environmental, family or other contextual factors that may contribute to behaviour have not been systematically studied.
A major limitation of existing PDA research and case studies is a lack of consideration of overlapping symptoms with other conditions, such as autism, attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, anxiety disorder, selective mutism and other developmental disorders. Diagnostic labels can have positive and negative consequences and so need to be thoroughly investigated before they are used in practice.
Classifying a “new” condition requires consistency across seven clinical and research aspects: epidemiological data, long-term patient follow-up, family inheritance, laboratory findings, exclusion from other conditions, response to treatment, and distinct predictors of outcome. At this stage, these domains have not been established for PDA. It is not clear whether PDA is different from other formal diagnoses or developmental differences.
When a child is stressed, demands or requests might tip them into fight, flight or freeze mode. Shutterstock Finding the why
Debates over classification don’t relieve distress for a child or those close to them. If a child is “intentionally” engaged in antisocial behaviour, the question is then “why?”
Beneath the behaviour is almost always developmental difference, genuine distress and difficulty coping. A broad and deep understanding of developmental processes is required.
Interestingly, while girls are “under-represented” in autism research, they are equally represented in studies characterising PDA. But if a child’s behaviour is only understood through a “pathologising” or diagnostic lens, there is a risk their agency may be reduced. Underlying experiences of distress, sensory overload, social confusion and feelings of isolation may be missed.
So, what can be done to help?
There are no empirical studies to date regarding PDA treatment strategies or their effectiveness. Clinical advice and case studies suggest strategies that may help include:
- reducing demands
- giving multiple options
- minimising expectations to avoid triggering avoidance
- engaging with interests to support regulation.
Early intervention in the preschool and primary years benefits children with complex developmental differences. Clinical care that involves a range of medical and allied health clinicians and considers the whole person is needed to ensure children and families get the support they need.
It is important to recognise these children often feel as frustrated and helpless as their caregivers. Both find themselves stuck in a repetitive cycle of distress, frustration and lack of progress. A personalised approach can take into account the child’s unique social, sensory and cognitive sensitivities.
In the preschool and early primary years, children have limited ability to manage their impulses or learn techniques for managing their emotions, relationships or environments. Careful watching for potential triggers and then working on timetables and routines, sleep, environments, tasks, and relationships can help.
As children move into later primary school and adolescence, they are more likely to want to influence others and be able to have more self control. As their autonomy and ability to collaborate increases, the problematic behaviours tend to reduce.
Strategies that build self-determination are crucial. They include opportunities for developing confidence, communication and more options to choose from when facing challenges. This therapeutic work with children and families takes time and needs to be revisited at different developmental stages. Support to engage in school and community activities is also needed. Each small step brings more capacity and more effective ways for a child to understand and manage themselves and their worlds.
What about Charlie?
The current scope to explain and manage PDA is limited. Future research must include the voices and views of children and adults with PDA symptoms.
Such emotional and behavioural difficulties are distressing and difficult for children and families. They need compassion and practical help.
For a child like Charlie, this could look like a series of sessions where she and her parents meet with clinicians to explore Charlie’s perspective, experiences and triggers. The family might come to understand that, in addition to autism, Charlie has complex developmental strengths and challenges, anxiety, and some difficulties with adjustment related to stress at home and school. This means Charlie experiences a fight, flight, freeze response that looks like aggression, avoidance or shutting down.
With carefully planned supports at home and school, Charlie’s options can broaden and her distress and avoidance can soften. Outside the clinic room, Charlie and her family can be supported to join an inclusive local community sporting or creative activity. Gradually she can spend more time engaged at home, school and in the community.
Nicole Rinehart, Professor, Child and Adolescent Psychology, Director, Krongold Clinic (Research), Monash University; David Moseley, Senior Research Fellow, Deputy Director (Clinical), Monash Krongold Clinic, Monash University, and Michael Gordon, Associate Professor, Psychiatry, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Anti-Inflammatory Pineapple Fried Rice
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fried rice is not most people’s go-to when one thinks of health food, but this one is. It’s packed with plenty of nutrients, many of which are anti-inflammatory, but the real star is the pineapple (with its high bromelain content and thus particularly potent benefits).
You will need
- 2½ cups cooked wholegrain basmati rice (you can use our Tasty Versatile Rice recipe if you don’t already have leftovers to use)
- 1 cup pineapple chunks
- ½ red onion, diced
- 1 red bell pepper, diced
- ½ cup sweetcorn
- ½ peas
- 3 green onions, chopped
- 2 serrano peppers, chopped (omit if you don’t care for heat)
- 2 tbsp coconut oil
- 1 tbsp grated fresh ginger
- 1 tbsp black pepper, coarse ground
Method
(we suggest you read everything at least once before doing anything)
1) Fry the red onion, serrano peppers, and ginger in the coconut oil over a medium heat, stirring frequently, for about 3 minutes.
2) Add the pineapple, bell pepper, sweetcorn, peas, and black pepper, stirring frequently, for about another 3 minutes.
3) Add the rice, stirring gently but thoroughly, until fully reheated and mixed in.
4) Serve, garnishing with the green onions.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat To Beat Inflammation
- Ginger Does A Lot More Than You Think
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Bromelain vs Inflammation & Much More
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: