The Joy of Saying No – by Natalie Lue
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Superficially, this seems an odd topic for an entire book. “Just say no”, after all, surely! But it’s not so simple as that, is it?
Lue looks into what underpins people-pleasing, first. Then, she breaks it down into five distinct styles of people-pleasing that each come from slightly different motivations and ways of perceiving how we interact with those around us.
Lest this seem overly complicated, those five styles are what she calls: gooding, efforting, avoiding, saving, suffering.
She then looks out how to have a healthier relationship with our yes/no decisions; first by observing, then by creating healthy boundaries. “Healthy” is key here; this isn’t about being a jerk to everyone! Quite the contrary, it involves being honest about what we can and cannot reasonably take on.
The last section is about improving and troubleshooting this process, and constitutes a lot of the greatest value of the book, since this is where people tend to err the most.
Bottom line: this book is informative, clear, and helpful. And far from disappointing everyone with “no”, we can learn to really de-stress our relationships with others—and ourselves.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Early Bird Or Night Owl? Genes vs Environment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Sliding Slope?
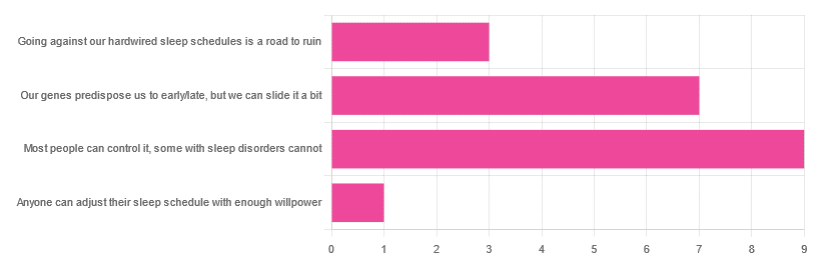
In Tuesday’s newsletter, we asked you how much control you believe we have over our sleep schedule, and got the above-depicted, below-described, set of responses:
- 45% said “most people can control it; some people with sleep disorders cannot
- 35% said “our genes predispose us to early/late, but we can slide it a bit
- 15% said: “going against our hardwired sleep schedules is a road to ruin”
- 5% said “anyone can adjust their sleep schedule with enough willpower”
You may be wondering: what’s with those single-digit numbers in the graph there? And the answer is: Tuesday’s email didn’t go out at the usual time due to a scheduling mistake (sorry!), which is probably what affected the number of responses (poll response levels vary, but are usually a lot higher than this).
Note: yes, this does mean most people who read our newsletter don’t vote. So, not to sound like a politician on the campaign trail, but… Your vote counts! We always love reading your comments when you add those, too—often they provide context that allow us to tailor what we focus on in our articles
However, those are the responses we got, so here we are!
What does the science say?
Anyone can adjust their sleep with enough willpower: True or False?
False, simply. It’s difficult for most people, but for many people with sleep disorders, it is outright impossible.
In a battle of narcolepsy vs willpower, for example, no amount of willpower will stop the brain from switching to sleep mode when it thinks it’s time to sleep:
❝Narcolepsy is the most common neurological cause of chronic sleepiness. The discovery about 20 years ago that narcolepsy is caused by selective loss of the neurons producing orexins sparked great advances in the field
[There is also] developing evidence that narcolepsy is an autoimmune disorder that may be caused by a T cell-mediated attack on the orexin neurons and explain how these new perspectives can inform better therapeutic approaches.❞
~ Dr. Carrie Mahoney et al. (lightly edited for brevity)
Source: The neurobiological basis of narcolepsy
For further reading, especially if this applies to you or a loved one:
Our genes predispose us to early/late, but we can slide it a bit: True or False?
True! First, about our genes predisposing us:
…and also:
Gene distinguishes early birds from night owls and helps predict time of death
Now, as for the “can slide it a bit”, this is really just a function of the general categories of “early bird” and “night owl” spanning periods of time that allow for a few hours’ wiggle-room at either side.
However, it is recommended to make any actual changes more gradually, with the Sleep Foundation going so far as to recommend 30 minutes, or even just 15 minutes, of change per day:
Sleep Foundation | How to Fix Your Sleep Schedule
Going against our hardwired sleep schedule is a road to ruin: True or False?
False, contextually. By this we mean: our “hardwired” sleep schedule is (for most of us), genetically predisposed but not predetermined.
Also, genetic predispositions are not necessarily always good for us; one would not argue, for example, for avoiding going against a genetic predisposition to addiction.
Some genetic predispositions are just plain bad for us, and genes can be a bit of a lottery.
That said, we do recommend getting some insider knowledge (literally), by getting personal genomics tests done, if that’s a viable option for you, so you know what’s really a genetic trait (and what to do with that information) and what’s probably caused by something else (and what to do with that information):
Genetic Testing: Health Benefits & Methods
Take care!
Share This Post
-
Eye Drops: Safety & Alternatives
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Before important business meetings my father used to use eye drops to add a “sparkle” to his eyes. I think that is a step too far, but what, short of eye drops, can we do to keep our eyes bright throughout the day?❞
Firstly, we’d indeed not recommend eye drops unless advised to do so by your doctor to treat a specific health condition:
- Infections from over-the-counter artificial tears
- Are my eye drops safe to use?
- More eye drops recalled due to infection danger
Those eye drops that “add sparkle” are often based on astringents such as witch hazel. This means that the capillaries in the eye undergo vasoconstriction, becoming much less visible and the eye thus appears much whiter and thus brighter.
There isn’t a way to do the same thing from the inside, as taking a vasoconstrictor will simply increase your general blood pressure, making the capillaries of your eyes more, rather than less, visible.
However, what you can do is…
- look after your general vasculature (cardiovascular health)
- in particular, reduce hypertension
- that includes limiting salt
- stay away from vasoconstrictors (including caffeine)
- reduce your resting cortisol levels
- that certainly also means reducing alcohol consumption
- maintain good hydration
Take care!
Share This Post
-
Ham Substitute in Bean Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
I am interested in what I can substitute for ham in bean soup?
Well, that depends on what the ham was like! You can certainly buy ready-made vegan lardons (i.e. small bacon/ham bits, often in tiny cubes or similar) in any reasonably-sized supermarket. Being processed, they’re not amazing for the health, but are still an improvement on pork.
Alternatively, you can make your own seitan! Again, seitan is really not a health food, but again, it’s still relatively less bad than pork (unless you are allergic to gluten, in which case, definitely skip this one).
Alternatively alternatively, in a soup that already contains beans (so the protein element is already covered), you could just skip the ham as an added ingredient, and instead bring the extra flavor by means of a little salt, a little yeast extract (if you don’t like yeast extract, don’t worry, it won’t taste like it if you just use a teaspoon in a big pot, or half a teaspoon in a smaller pot), and a little smoked paprika. If you want to go healthier, you can swap out the salt for MSG, which enhances flavor in a similar fashion while containing less sodium.
Wondering about the health aspects of MSG? Check out our main feature on this, from last month:
Share This Post
Related Posts
-
The Uses of Delusion – by Dr. Stuart Vyse
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Most of us try to live rational lives. We try to make the best decisions we can based on the information we have… And if we’re thoughtful, we even try to be aware of common logical fallacies, and overcome our personal biases too. But is self-delusion ever useful?
Dr. Stuart Vyse, psychologist and Fellow for the Committee for Skeptical Inquiry, argues that it can be.
From self-fulfilling prophecies of optimism and pessimism, to the role of delusion in love and loss, Dr. Vyse explores what separates useful delusion from dangerous irrationality.
We also read about such questions as (and proposed answers to):
- Why is placebo effect stronger if we attach a ritual to it?
- Why are negative superstitions harder to shake than positive ones?
- Why do we tend to hold to the notion of free will, despite so much evidence for determinism?
The style of the book is conversational, and captivating from the start; a highly compelling read.
Bottom line: if you’ve ever felt yourself wondering if you are deluding yourself and if so, whether that’s useful or counterproductive, this is the book for you!
Click here to check out The Uses of Delusion, and optimize yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
When And Why Do We Pick Up Our Phones?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The School of Life’s Alain de Botton makes the argument that—if we pay attention, if we keep track—there’s an understory to why we pick up our phones:
It’s not about information
Yes, our phones (or rather, the apps therein) are designed to addict us, to draw us back, to keep us scrolling and never let us go. We indeed seek out information like our ancestors once sought out berries; searching, encouraged by a small discovery, looking for more. The neurochemistry is similar.
But when we look at the “when” of picking up our phones, de Botton says, it tells a different story:
We pick them up not to find out what’s going on with the world, but rather specifically to not find out what’s going with ourselves. We pick them up to white out some anxiety we don’t want to examine, a line of thought we don’t want to go down, memories we don’t want to consider, futures we do not want to have to worry about.
And of course, phones do have a great educational potential, are an immensely powerful tool for accessing knowledge of many kinds—if only we can remain truly conscious while using them, and not take them as the new “opiate of the masses”.
De Botton bids us, when next we pick up our phone. ask a brave question:
“If I weren’t allowed to consult my phone right now, what might I need to think about?”
As for where from there? There’s more in the video:
Click Here If The Embedded Video Doesn’t Load Automatically!
Further reading
Making Social Media Work For Your Mental Health
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Why ’10almonds’? Newsletter Name Explained
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Each Thursday, we respond to subscriber questions and requests! If it’s something small, we’ll answer it directly; if it’s something bigger, we’ll do a main feature in a follow-up day instead!
So, no question/request to big or small; they’ll just get sorted accordingly
Remember, you can always hit reply to any of our emails, or use the handy feedback widget at the bottom. We always look forward to hearing from you!
Q: Why is your newsletter called 10almonds? Maybe I missed it in the intro email, but my curiosity wants to know the significance. Thanks!”
It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was online… So, calling ourselves 10almonds was a bit of a tongue-in-cheek reference to that story… but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: