The Checklist Manifesto – by Dr. Atul Gawande
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dr. Gawande, himself a general surgeon, uses checklists a lot. He is, unequivocally, an expert in his field. He “shouldn’t” need a checklist to tell him to do such things as “Check you have the correct patient”. But checklists are there as a safety net. And, famously, “safety regulations are written in blood”, after all.
And, who amongst us has never made such a “silly” error? From forgetting to turn the oven on, to forgetting to take the handbrake off, it takes only a momentary distraction to think we’ve done something we haven’t.
You may be wondering: why a whole book on this? Is it just many examples of the usefulness of checklists? Because I’m already sold on that, so, what else am I going to get out of it?
Dr. Gawande also explains in clear terms:
- How to optimize “all necessary steps” with “as few steps as possible”
- The important difference between read-do checklists and do-confirm checklists
- To what extent we should try to account for the unexpected
- How to improve compliance (i.e., making sure you actually use it, no matter how tempting it will be to go “yeah this is automatic for me now” and gloss over it)
- The role of checklists in teams, and in passing on knowledge
…and more.
Bottom line: if you’ve ever tried to make tea without putting the tea-leaves in the pot, this is the book that will help you avoid making more costly mistakes—whatever your area of activity or interest.
Click here to check out the Checklist Manifesto, and make fewer mistakes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Lies That Depression Tells Us
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this short (6:42) video, psychiatrist Dr. Tracey Marks talks about 8 commonly-believed lies that depression often tells us. They are:
- “I don’t measure up”
- “No one cares about me”
- “I’m better off alone”
- “No one understands”
- “It’s all my fault”
- “I have no reason to be depressed”
- “Nothing matters”
- “I’ll never get better”
Some of these can be reinforced by people around us; it’s easy to believe that “no one understands” if for example the few people we interact with the most don’t understand, or that “I have no reason to be depressed” if people try to cheer you up by pointing out your many good fortunes.
The reality, of course, is that depression is a large, complex, and many-headed beast, with firm roots in neurobiology.
There are things we can do that may ameliorate it… But they also may not, and sometimes life is just going to suck for a while. That doesn’t mean we should give up (that, too, is depression lying to us, per “I’ll never get better”), but it does mean that we should not be so hard on ourselves for not having “walked it off” the way one might “just walk off” a broken leg.
Oh, you can’t “just walk off” a broken leg? Well then, perhaps it’s not surprising if we don’t “just think off” a broken brain, either. The brain can rebuild itself, but that’s a slow process, so buckle in:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to know more?
You might like these previous articles of ours about depression (managing it, and overcoming it):
- The Mental Health First-Aid That You’ll Hopefully Never Need
- Behavioral Activation Against Depression & Anxiety
- The Easiest Way To Take Up Journaling
- Antidepressants: Personalization Is Key!
Take care!
Share This Post
-
Remember – by Dr. Lisa Genova
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Memory is often viewed as one thing—either you have a good memory, or you don’t. At best, a lot of people have a vague idea of selective memory. But, the reality is much more complex—and much more interesting.
Dr. Genova lays out clearly and simply the various different kinds of memory, how they work, and how they fail. Some of these kinds of memory operate on completely different principles than others, and/or in different parts of the brain. And, it’s not just “a memory for faces” or a “memory for names”, nor even “short term vs long term”. There’s working memory, explicit and implicit memory, semantic memory, episodic memory, muscle memory, and more.
However, this is not just an interesting book—it’s also a useful one. Dr. Genova also looks at how we can guard against failing memory in later years, and how we can expand and grow the kinds of memory that are most important to us.
The style of the book is very conversational, and not at all textbook-like. It’s certainly very accessible, and pleasant to read too.
Bottom line: memory is a weird and wonderful thing, and this book shines a clear light on many aspects of it—including how to improve the various different kinds of memory.
Click here to check out Remember (we recommend to do it now before you forget!
Share This Post
-
Brain Power – by Michael Gelb & Kelly Howell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s most important when it comes to brain health? Is it the right diet? Supplements? Brain-training? Attitude? Sleep? Physical exercise? Social connections? Something else?
This book covers a lot of bases, including all of the above and more. The authors are not scientists by training and this is not a book of science, so much as a book of aggregated science-based advice from other sources. The authors did consult with many scientists, and their input is shown throughout.
In the category of criticism, nothing here goes very deeply into the science, and there’s also nothing you wouldn’t find we’ve previously written about in a 10almonds article somewhere. But all the same, it’s good to have a wide variety of brain-healthy advices all in one place.
Bottom line: if you’re looking for a one-stop-shop “look after your brain as you age” guide, then this is a good one.
Click here to check out Brain Power, and improve your mind as you age!
Share This Post
Related Posts
-
Get Better Sleep: Beyond The Basics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First though, for the sake of being methodical, let’s quickly note the basics:
- Aim for 7–9 hours per night
- Set a regular bedtime and (equally important!) regular getting-up time
- Have a 2-hour wind-down period before bed, to decompress from any stresses of the day
- Minimal device/screen usage before bed
- Abstain from stimulants for as long before bed as reasonably possible (caffeine elimination halflife is 4–8 hours depending on your genes, call it 6 hours average to eliminate half (not the whole lot), and you’ll see it’s probably best to put a cap on it earlier rather than later).
- Abstain from alcohol, ideally entirely, but allow at least 1hr/unit before bed. So for example, 1hr for a 1oz single shot of spirits, or 2–3 hours for a glass of wine (depending on size), or 3–4 hours for a martini (depending on recipe). Not that that is not the elimination time, nor even the elimination halflife of alcohol, it’s just a “give your body a chance at least” calculation. If you like to have a drink to relax before bed, then well, only you can decide what you like more: that or actually getting restorative sleep.
- Consider a warm bath/shower before bed, if that suits your schedule.
- Wash and change your bedsheets more often than seems necessary. Or if that’s too onerous, at least change the pillowcases more often, which makes quite a difference already.
- Lower the temperature of your bedroom shortly before bedtime; this will help cue the body to produce melatonin
- Make your bedroom as dark as reasonably possible. Invest in blackout blinds/curtains, and remove any pesky electronics, or at least cover their little LEDs if it’s something that reasonably needs to remain on.
Ok, now, onwards…
Those 7–9 hours? Yes, it goes for you too.
A lot of people mistake getting 6 hours sleep per night for only needing 6 hours sleep per night. Sure, you may still be alive after regularly getting 6 hours, but (unless you have a rare mutation of the ADRB1 gene) it will be causing harm, and yes, that includes later in life; we don’t stop needing so much sleep, even stop getting it:
Why You Probably Need More Sleep
With this in mind, it becomes important to…
Prioritize your sleep—which means planning for it!
When does your bedtime routine start? According to sleep scientist Dr. Lisa Matricciani, it starts before breakfast. This is because the things we do earlier in the day can greatly affect the amount (and quality) of sleep we get later. For example, a morning moderate-to-intense exercise session greatly improves sleep at night:
Planning Ahead For Better Sleep
As for quality, that is as important as quantity, and it’s not just about “soundness” of sleep:
The 6 Dimensions Of Sleep (And Why They Matter)
“What gets measured, gets done” goes for sleep too
Sleep-deprived people usually underestimate how sleep-deprived they are. This is for the same reason as why drunk people usually underestimate how drunk they are—to put it in words that go for both situations: a cognitively impaired person lacks the cognitive function to realize how cognitively impaired they are.
Here’s the science on that, by the way:
How Sleep-Deprived Are You, Really?
For that reason, we recommend using sleep-tracking software (there are many apps for that) on your phone or, ideally, a wearable device (such as a smartwatch or similar).
A benefit of doing so is that we don’t think “well, I slept from 10pm to 6am, so that’s 8 hours”, if our device tells us we slept between 10:43pm and 5:56 am with 74% sleep efficiency because we woke up many times.
As an aside, sleep efficiency should be about 85%, by the way. Why not 100%, you ask? It’s because if your body is truly out like a light for the entire night, something is wrong (either you were very sleep-deprived, or you have been drugged, that kind of thing). See also:
An unbroken night’s sleep is a myth. Here’s what good sleep looks like.
So waking up during the night is normal, and nothing to worry about per se. If you do find trouble getting back to sleep, though:
How to Fall Back Asleep After Waking Up in the Middle of the Night
Be careful about how you try to supplement sleep
This goes both for taking substances of various kinds, and napping. Some sleep aids can help, but many are harmful and/or do not really work as such; here’s a rundown of examples of those:
Safe Effective Sleep Aids For Seniors?
And when it comes to napping, timing is everything:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
Want to know a lot more?
This is the book on sleep:
Why We Sleep – by Dr. Matthew Walker
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Bird flu has been detected in a pig in the US. Why does that matter?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The United States Department of Agriculture last week reported that a pig on a backyard farm in Oregon was infected with bird flu.
As the bird flu situation has evolved, we’ve heard about the A/H5N1 strain of the virus infecting a range of animals, including a variety of birds, wild animals and dairy cattle.
Fortunately, we haven’t seen any sustained spread between humans at this stage. But the detection of the virus in a pig marks a worrying development in the trajectory of this virus.
David MG/Shutterstock How did we get here?
The most concerning type of bird flu currently circulating is clade 2.3.4.4b of A/H5N1, a strain of influenza A.
Since 2020, A/H5N1 2.3.4.4b has spread to a vast range of birds, wild animals and farm animals that have never been infected with bird flu before.
While Europe is a hotspot for A/H5N1, attention is currently focused on the US. Dairy cattle were infected for the first time in 2024, with more than 400 herds affected across at least 14 US states.
Bird flu has enormous impacts on farming and commercial food production, because infected poultry flocks have to be culled, and infected cows can result in contaminated diary products. That said, pasteurisation should make milk safe to drink.
While farmers have suffered major losses due to H5N1 bird flu, it also has the potential to mutate to cause a human pandemic.
Birds and humans have different types of receptors in their respiratory tract that flu viruses attach to, like a lock (receptors) and key (virus). The attachment of the virus allows it to invade a cell and the body and cause illness. Avian flu viruses are adapted to birds, and spread easily among birds, but not in humans.
So far, human cases have mainly occurred in people who have been in close contact with infected farm animals or birds. In the US, most have been farm workers.
The concern is that the virus will mutate and adapt to humans. One of the key steps for this to happen would be a shift in the virus’ affinity from the bird receptors to those found in the human respiratory tract. In other words, if the virus’ “key” mutated to better fit with the human “lock”.
A recent study of a sample of A/H5N1 2.3.4.4b from an infected human had worrying findings, identifying mutations in the virus with the potential to increase transmission between human hosts.
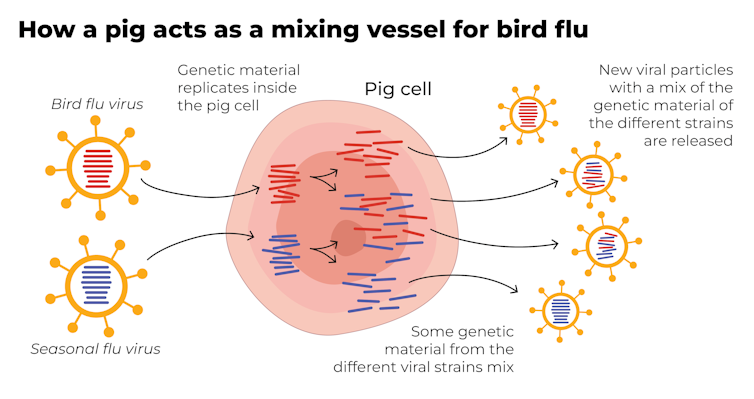
Why are pigs a problem?
A human pandemic strain of influenza can arise in several ways. One involves close contact between humans and animals infected with their own specific flu viruses, creating opportunities for genetic mixing between avian and human viruses.
Pigs are the ideal genetic mixing vessel to generate a human pandemic influenza strain, because they have receptors in their respiratory tracts which both avian and human flu viruses can bind to.
This means pigs can be infected with a bird flu virus and a human flu virus at the same time. These viruses can exchange genetic material to mutate and become easily transmissible in humans.
The Conversation, CC BY-SA Interestingly, in the past pigs were less susceptible to A/H5N1 viruses. However, the virus has recently mutated to infect pigs more readily.
In the recent case in Oregon, A/H5N1 was detected in a pig on a non-commercial farm after an outbreak occurred among the poultry housed on the same farm. This strain of A/H5N1 was from wild birds, not the one that is widespread in US dairy cows.
The infection of a pig is a warning. If the virus enters commercial piggeries, it would create a far greater level of risk of a pandemic, especially as the US goes into winter, when human seasonal flu starts to rise.
How can we mitigate the risk?
Surveillance is key to early detection of a possible pandemic. This includes comprehensive testing and reporting of infections in birds and animals, alongside financial compensation and support measures for farmers to encourage timely reporting.
Strengthening global influenza surveillance is crucial, as unusual spikes in pneumonia and severe respiratory illnesses could signal a human pandemic. Our EPIWATCH system looks for early warnings of such activity, which can speed up vaccine development.
If a cluster of human cases occurs, and influenza A is detected, further testing (called subtyping) is essential to ascertain whether it’s a seasonal strain, an avian strain from a spillover event, or a novel pandemic strain.
Early identification can prevent a pandemic. Any delay in identifying an emerging pandemic strain enables the virus to spread widely across international borders.
Australia’s first human case of A/H5N1 occurred in a child who acquired the infection while travelling in India, and was hospitalised with illness in March 2024. At the time, testing revealed Influenza A (which could be seasonal flu or avian flu), but subtyping to identify A/H5N1 was delayed.
This kind of delay can be costly if a human-transmissible A/H5N1 arises and is assumed to be seasonal flu because the test is positive for influenza A. Only about 5% of tests positive for influenza A are subtyped further in Australia and most countries.
In light of the current situation, there should be a low threshold for subtyping influenza A strains in humans. Rapid tests which can distinguish between seasonal and H5 influenza A are emerging, and should form part of governments’ pandemic preparedness.
A higher risk than ever before
The US Centers for Disease Control and Prevention states that the current risk posed by H5N1 to the general public remains low.
But with H5N1 now able to infect pigs, and showing worrying mutations for human adaptation, the level of risk has increased. Given the virus is so widespread in animals and birds, the statistical probability of a pandemic arising is higher than ever before.
The good news is, we are better prepared for an influenza pandemic than other pandemics, because vaccines can be made in the same way as seasonal flu vaccines. As soon as the genome of a pandemic influenza virus is known, the vaccines can be updated to match it.
Partially matched vaccines are already available, and some countries such as Finland are vaccinating high-risk farm workers.
C Raina MacIntyre, Professor of Global Biosecurity, NHMRC L3 Research Fellow, Head, Biosecurity Program, Kirby Institute, UNSW Sydney and Haley Stone, Research Associate, Biosecurity Program, Kirby Institute & CRUISE lab, Computer Science and Engineering, UNSW Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Strawberries vs Cherries – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing strawberries to cherries, we picked the cherries.
Why?
Both are great, and an argument could be made for either! But here’s our rationale:
In terms of macros, as with most fruits they are both mostly water, and have similar carbs and fiber. Nominally, cherries have the lower glycemic index, so we could call this category nominally a win for cherries, but honestly, they’re both low-GI foods and nobody is getting metabolic disease from eating strawberries, so it’s fairer to consider this category a tie.
Looking at the vitamins, strawberries have more of vitamins C, B9, E, and K, while cherries have more of vitamins A, B1, B2, B3, B5, and choline. Thus, a modest win for cherries here.
When it comes to minerals, strawberries see their day: strawberries have more iron, magnesium, manganese, and phosphorus, while cherries have more calcium, copper, and potassium. By the numbers, a win for strawberries.
So far, so tied!
What swings it into cherries’ favor is cherries’ slew of specific phytochemical benefits, including cherry-specific anti-inflammatory properties, sleep-improving abilities, and post-exercise recovery boosts, as well as anti-diabetic benefits above and beyond the normal “this is a fruit” level.
In short, both are very respectable fruits, but cherries have some extra qualities that are just special.
Of course, as ever, enjoy either or both; diversity is good!
Want to learn more?
You might like to read:
Cherries’ Health Benefits Simply Pop
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: