The 4 Bad Habits That Cause The Most Falls While Walking
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The risk of falling becomes greater (both in probability and in severity of consequences) as we get older. But, many people who do fall do so for the same reasons, some of which are avoidable. Dr. Doug Weiss has advice based on extensive second-hand experience:
Best foot forward!
If any of these prompt a “surely nobody does that” response, then, good for you to not have that habit, but Dr. Weiss has seen many patients who thusly erred. And if any of these do describe how you walk, then well, you’re not alone—time to fix it, though!
- Walking with Stiff Legs: walking with a hyperextended (straight) knee instead of a slight bend (5-15°) makes it harder to adjust balance, increasing the risk of falls. This can also put extra pressure on the joints, potentially leading to osteoarthritis.
- Crossing Legs While Turning: turning by crossing one leg over the other is a common cause of falls, particularly in the elderly. To avoid this, when turning step first with the foot that is on the side you are going to go. If you have the bad habit, this may feel strange at first, but you will soon adapt.
- Looking Down While Walking: focusing only on the ground directly in front of you can cause you to miss obstacles ahead, leading to falls. Instead, practice “scanning”, alternating between looking down at the ground and looking up to maintain awareness of your surroundings.
- Shuffling Instead of Tandem Walking: shuffling with feet far apart, rather than walking with one foot in front of the other, reduces balance and increases the risk of tripping. Tandem walking, where one foot is placed directly in front of the other, is the safer and more balanced way to walk.
It also helps disguise your numbers.
For more details on all of these, plus visual demonstrations, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special (How To Not Fall, And How To Minimize Injury If You Do) ← this never seems like an urgent thing to learn, but trust us, it’s more fun to read it now, than from your hospital bed later
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Do You Have A Personalized Health Plan? (Here’s How)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Good health” is quite a broad umbrella, and while we all have a general idea of what “healthy” looks like, it’s easy to focus on some areas and overlook others.
Of course, how much one does this will still depend on one’s level of interest in health, which can change over the course of life, and (barring serious midlife health-related curveballs such as a cancer diagnosis or something) often looks like an inverse bell curve:
- As small kids, we probably barely thought about health
- As teenagers, we probably had a narrow view of health (often related to whatever is considered sexually attractive at the time)
- In our 20s, may have a bit of a health kick in which we learn and apply a lot… Which often then gets to later take a bit of a back seat to work responsibilities and so forth
- This is commonly followed by a few decades of just trying to make it to Friday by any means necessary (definite risk factor for substance abuse of various kinds), double if we have kids, triple if we have work, kids, and are also solely responsible for managing the household.
- Then just as suddenly as it is predictably, we are ambushed when approaching retirement age by a cluster of age-related increased health risks that we now get to do our best to mitigate—the focus here is “not dying early”. A lot of health education occurs at this time.
- Finally, upon retirement, we actually get the time to truly focus on our health again, and now it’s easier to learn about all aspects of health, even if now there’s a need to juggle many health issues all at once, most of which affect the others.
See also: How Likely Are You To Live To 100? ← in which we can also see a graph of 10almonds subscribers’ ages, consistent with the above
So, let’s recap, and personalize our health plan
There are often things we wish we could have focused on sooner, so now’s the time to figure out what future-you in your next decade (or later!) is going to thank you for having done now.
So, while 20-year-old us might have been focusing on fat levels or athletic performance, how much does that really help us now? (With apologies to any readers in their 20s, but also, with the bonus for you: now’s the perfect time to plan ahead!)
At 10almonds, while we cover very many health topics, we often especially focus on:
- Brain health
- Heart health
- Gut health
…because they affect everything else so much. We’ve listed them there in the order they appear in the body, but in fact it can be useful to view them upside down, because:
- Gut health is critical for good metabolic health (a happy efficient gut allows us to process nutrients, including energy, efficiently)
- Metabolic health is critical for good heart health (a nicely ticking metabolism will not strain our heart)
- Heart health is critical for good brain health (a strong heart will nourish the brain with well-oxygenated blood and the nutrients it also carries)
So, this isn’t a catch-22 at all! There is a clear starting point:
“How do I do the other bits, though?”
We have you covered here: Your Health Audit, From Head To Toe
“Wait, where’s the personalization?”
This comes once you’ve got those above things in order.
Hopefully you know what particular health risks you have—as in, particular to you.
First, you will have any current diagnoses, and a plan for treating those. Many chronic illnesses can be reversed or at least lessened with lifestyle changes, in particular, if we reduce chronic inflammation, which is implicated in countless chronic illnesses, and exacerbates most of the rest.
So: How to Prevent (or Reduce) Inflammation
The same goes for any heightened risks you have as a result of those current diagnoses.
Next, you will have any genetic health risks—so here’s where genetic testing is a good one-shot tool, to get a lot of information all in one go.
Learn more: The Real Benefit Of Genetic Testing
…and then, of course, take appropriate steps to avoid suffering the things of which you are at increased genetic risk.
Finally, you will have any personal concerns or goals—in other words, what do you want to still be able to do, later in life? It’s easy to say “everything”, but what’s most important?
This writer’s example: I want to remain mobile, free from pain, and sharp of mind.
That doesn’t mean I’ll neglect the rest of my health, but it does mean that I will regularly weigh my choices against whether they are consistent with those three things.
As for how to plan for that?
Check out: Train For The Event Of Your Life! ← this one is mostly about the mobility aspect; staying free from pain is in large part a matter of avoiding inflammation which we already discussed, and staying sharp of mind relies on the gut-heart-brain pipeline we also covered.
You can also, of course, personalize your diet per which areas of health are the most important for you:
Four Ways To Upgrade The Mediterranean (most anti-inflammatory, gut-healthiest, heart-healthiest, brain-healthiest)
Take care!
Share This Post
-
Sunflower Corn Burger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Burgers are rarely a health food, but in this case, everything in the patty is healthy, and it’s packed with protein, fiber, and healthy fats.
You will need
- 1 can chickpeas
- ¾ cup frozen corn
- ½ cup chopped fresh parsley
- ⅓ cup sunflower seeds
- ⅓ cup cornichon pickles
- ⅓ cup wholegrain bread crumbs (gluten-free, if desired/required)
- ¼ bulb garlic (or more if you want a stronger flavor)
- 1 tbsp extra virgin olive oil, plus more for frying
- 1 tbsp nutritional yeast (or 1 tsp yeast extract)
- 2 tsp ground cumin
- 2 tsp red pepper flakes
- 2 tsp black pepper, coarse ground
- 1 tsp Dijon mustard
- To serve: 4 burger buns; these are not usually healthy, so making your own is best, but if you don’t have the means/time, then getting similarly shaped wholegrain bread buns works just fine.
- Optional: your preferred burger toppings, e.g. greenery, red onion, tomato slices, avocado, jalapeños, whatever does it for you
Note: there is no need to add salt; there is enough already in the pickles.
Method
(we suggest you read everything at least once before doing anything)
1) Combine all the ingredients except the buns (and any optional toppings) in a food processor, pulsing a few times for a coarse texture (not a purée).
2) Shape the mixture into 4 burger patties, and let them chill in the fridge for at least 30 minutes.
3) Heat a skillet over a medium-high heat with some olive oil, and fry the burgers on both sides until they develop a nice golden crust; this will probably take about 4 minutes per side.
4) Assemble in the buns with any toppings you want, and serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Sunflower Seeds vs Pumpkin Seeds – Which is Healthier? ← pumpkin seeds have more micronutrients; sunflower seeds have more healthy fats; feel free to use either or both in this recipe
- What Omega-3 Fatty Acids Really Do For Us
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Making Friends With Your Gut (You Can Thank Us Later)
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
Taking A Trip Through The Evidence On Psychedelics
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
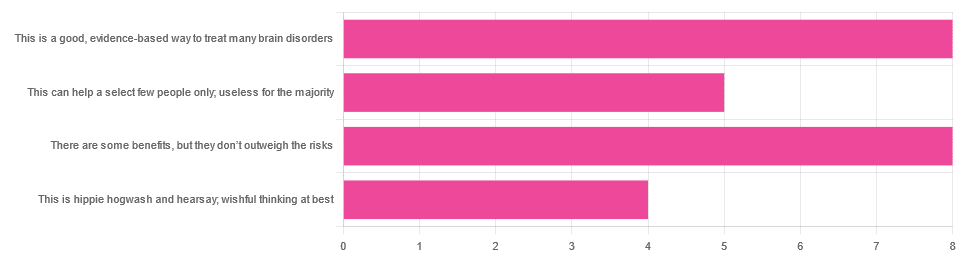
In Tuesday’s newsletter, we asked you for your opinions on the medicinal use of psychedelics, and got the above-depicted, below-described, set of responses:
- 32% said “This is a good, evidence-based way to treat many brain disorders”
- 32% said “There are some benefits, but they don’t outweigh the risks”
- 20% said “This can help a select few people only; useless for the majority”
- 16% said “This is hippie hogwash and hearsay; wishful thinking at best”
Quite a spread of answers, so what does the science say?
This is hippie hogwash and hearsay; wishful thinking at best! True or False?
False! We’re tackling this one first, because it’s easiest to answer:
There are some moderately-well established [usually moderate] clinical benefits from some psychedelics for some people.
If that sounds like a very guarded statement, it is. Part of this is because “psychedelics” is an umbrella term; perhaps we should have conducted separate polls for psilocybin, MDMA, ayahuasca, LSD, ibogaine, etc, etc.
In fact: maybe we will do separate main features for some of these, as there is a lot to say about each of them separately.
Nevertheless, looking at the spread of research as it stands for psychedelics as a category, the answers are often similar across the board, even when the benefits/risks may differ from drug to drug.
To speak in broad terms, if we were to make a research summary for each drug it would look approximately like this in each case:
- there has been research into this, but not nearly enough, as “the war on drugs” may well have manifestly been lost (the winner of the war being: drugs; still around and more plentiful than ever), but it did really cramp science for a few decades.
- the studies are often small, heterogenous (often using moderately wealthy white student-age population samples), and with a low standard of evidence (i.e. the methodology often has some holes that leave room for reasonable doubt).
- the benefits recorded are often small and transient.
- in their favor, though, the risks are also generally recorded as being quite low, assuming proper safe administration*.
*Illustrative example:
Person A takes MDMA in a club, dances their cares away, has had only alcohol to drink, sweats buckets but they don’t care because they love everyone and they see how we’re all one really and it all makes sense to them and then they pass out from heat exhaustion and dehydration and suffer kidney damage (not to mention a head injury when falling) and are hospitalized and could die;
Person B takes MDMA in a lab, is overwhelmed with a sense of joy and the clarity of how their participation in the study is helping humanity; they want to hug the researcher and express their gratitude; the researcher reminds them to drink some water.
Which is not to say that a lab is the only safe manner of administration; there are many possible setups for supervised usage sites. But it does mean that the risks are often as much environmental as they are risks inherent to the drug itself.
Others are more inherent to the drug itself, such as adverse cardiac events for some drugs (ibogaine is one that definitely needs medical supervision, for example).
For those who’d like to see numbers and clinical examples of the bullet points we gave above, here you go; this is a great (and very readable) overview:
NIH | Evidence Brief: Psychedelic Medications for Mental Health and Substance Use Disorders
Notwithstanding the word “brief” (intended in the sense of: briefing), this is not especially brief and is rather an entire book (available for free, right there!), but we do recommend reading it if you have time.
This can help a select few people only; useless for the majority: True or False?
True, technically, insofar as the evidence points to these drugs being useful for such things as depression, anxiety, PTSD, addiction, etc, and estimates of people who struggle with mental health issues in general is often cited as being 1 in 4, or 1 in 5. Of course, many people may just have moderate anxiety, or a transient period of depression, etc; many, meanwhile, have it worth.
In short: there is a very large minority of people who suffer from mental health issues that, for each issue, there may be one or more psychedelic that could help.
This is a good, evidence-based way to treat many brain disorders: True or False?
True if and only if we’re willing to accept the so far weak evidence that we discussed above. False otherwise, while the jury remains out.
One thing in its favor though is that while the evidence is weak, it’s not contradictory, insofar as the large preponderance of evidence says such therapies probably do work (there aren’t many studies that returned negative results); the evidence is just weak.
When a thousand scientists say “we’re not completely sure, but this looks like it helps; we need to do more research”, then it’s good to believe them on all counts—the positivity and the uncertainty.
This is a very different picture than we saw when looking at, say, ear candling or homeopathy (things that the evidence says simply do not work).
We haven’t been linking individual studies so far, because that book we linked above has many, and the number of studies we’d have to list would be:
n = number of kinds of psychedelic drugs x number of conditions to be treated
e.g. how does psilocybin fare for depression, eating disorders, anxiety, addiction, PTSD, this, that, the other; now how does ayahuasca fare for each of those, and so on for each drug and condition; at least 25 or 30 as a baseline number, and we don’t have that room.
But here are a few samples to finish up:
- Psilocybin as a New Approach to Treat Depression and Anxiety in the Context of Life-Threatening Diseases—A Systematic Review and Meta-Analysis of Clinical Trials
- Therapeutic Use of LSD in Psychiatry: A Systematic Review of Randomized-Controlled Clinical Trials
- Efficacy of Psychoactive Drugs for the Treatment of Posttraumatic Stress Disorder: A Systematic Review of MDMA, Ketamine, LSD and Psilocybin
- Changes in self-rumination and self-compassion mediate the effect of psychedelic experiences on decreases in depression, anxiety, and stress.
- Psychedelic Treatments for Psychiatric Disorders: A Systematic Review and Thematic Synthesis of Patient Experiences in Qualitative Studies
- Repeated lysergic acid diethylamide (LSD) reverses stress-induced anxiety-like behavior, cortical synaptogenesis deficits and serotonergic neurotransmission decline
In closing…
The general scientific consensus is presently “many of those drugs may ameliorate many of those conditions, but we need a lot more research before we can say for sure”.
On a practical level, an important take-away from this is twofold:
- drugs, even those popularly considered recreational, aren’t ontologically evil, generally do have putative merits, and have been subject to a lot of dramatization/sensationalization, especially by the US government in its famous war on drugs.
- drugs, even those popularly considered beneficial and potentially lifechangingly good, are still capable of doing great harm if mismanaged, so if putting aside “don’t do drugs” as a propaganda of the past, then please do still hold onto “don’t do drugs alone”; trained professional supervision is a must for safety.
Take care!
Share This Post
Related Posts
-
Anti-Inflammatory Piña Colada Baked Oats
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
If you like piña coladas and getting songs stuck in your head, then enjoy this very anti-inflammatory, gut-healthy, blood-sugar-balancing, and frankly delicious dish:
You will need
- 9 oz pineapple, diced
- 7 oz rolled oats
- 3 oz desiccated coconut
- 14 fl oz coconut milk (full fat, the kind from a can)
- 14 fl oz milk (your choice what kind, but we recommend coconut, the kind for drinking)
- Optional: some kind of drizzling sugar such as honey or maple syrup
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Mix all the ingredients (except the drizzling sugar, if using) well, and put them in an ovenproof dish, compacting the mixture down gently so that the surface is flat.
3) Drizzle the drizzling sugar, if drizzling.
4) Bake in the oven for 30–40 minutes, until lightly golden-brown.
5) Serve hot or cold:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Bromelain vs Inflammation & Much More ← as found (uniquely!) in pineapple
- Can Saturated Fats Be Healthy? ← coconut certainly can!
- The Best Kind Of Fiber For Overall Health? ← it’s β-glucan, as found in abundance in oats
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Longevity for the Lazy – by Dr. Richard Malish
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some people who devote all their resources to longevity, which can become a full-time occupation, not to mention a very expensive endeavor. This book’s for those who want to get the best possible “bang for buck” by doing the things that have the most favorable cost:worth ratio.
Dr. Malish covers what can be done easily for personal longevity, as well as what technological advances can be enjoyed that those before us didn’t have as options. He also discusses the diseases that are most likely to kill us, and how to avoid those.
He preaches a proactive approach, but one that is simple and consistent and based in good science, and good statistics. Indeed, while he’s served 20 years as an army doctor and a cardiologist, he now works as a healthcare policy consultant, so he is well-placed to advise.
The style of the book is halfway between regular pop-science and a textbook; you can either read it cover-to-cover, or skim first though the key points, highlight boxes, summaries, and the like. He also provides a time-phased task list, for those who like things to be laid out like that.
Bottom line: this is a very good, methodical guide to living longer without making it a full-time occupation.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
‘I keep away from people’ – combined vision and hearing loss is isolating more and more older Australians
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our ageing population brings a growing crisis: people over 65 are at greater risk of dual sensory impairment (also known as “deafblindness” or combined vision and hearing loss).
Some 66% of people over 60 have hearing loss and 33% of older Australians have low vision. Estimates suggest more than a quarter of Australians over 80 are living with dual sensory impairment.
Combined vision and hearing loss describes any degree of sight and hearing loss, so neither sense can compensate for the other. Dual sensory impairment can occur at any point in life but is increasingly common as people get older.
The experience can make older people feel isolated and unable to participate in important conversations, including about their health.
bricolage/Shutterstock Causes and conditions
Conditions related to hearing and vision impairment often increase as we age – but many of these changes are subtle.
Hearing loss can start as early as our 50s and often accompany other age-related visual changes, such as age-related macular degeneration.
Other age-related conditions are frequently prioritised by patients, doctors or carers, such as diabetes or heart disease. Vision and hearing changes can be easy to overlook or accept as a normal aspect of ageing. As an older person we interviewed for our research told us
I don’t see too good or hear too well. It’s just part of old age.
An invisible disability
Dual sensory impairment has a significant and negative impact in all aspects of a person’s life. It reduces access to information, mobility and orientation, impacts social activities and communication, making it difficult for older adults to manage.
It is underdiagnosed, underrecognised and sometimes misattributed (for example, to cognitive impairment or decline). However, there is also growing evidence of links between dementia and dual sensory loss. If left untreated or without appropriate support, dual sensory impairment diminishes the capacity of older people to live independently, feel happy and be safe.
A dearth of specific resources to educate and support older Australians with their dual sensory impairment means when older people do raise the issue, their GP or health professional may not understand its significance or where to refer them. One older person told us:
There’s another thing too about the GP, the sort of mentality ‘well what do you expect? You’re 95.’ Hearing and vision loss in old age is not seen as a disability, it’s seen as something else.
Isolated yet more dependent on others
Global trends show a worrying conundrum. Older people with dual sensory impairment become more socially isolated, which impacts their mental health and wellbeing. At the same time they can become increasingly dependent on other people to help them navigate and manage day-to-day activities with limited sight and hearing.
One aspect of this is how effectively they can comprehend and communicate in a health-care setting. Recent research shows doctors and nurses in hospitals aren’t making themselves understood to most of their patients with dual sensory impairment. Good communication in the health context is about more than just “knowing what is going on”, researchers note. It facilitates:
- shorter hospital stays
- fewer re-admissions
- reduced emergency room visits
- better treatment adherence and medical follow up
- less unnecessary diagnostic testing
- improved health-care outcomes.
‘Too hard’
Globally, there is a better understanding of how important it is to maintain active social lives as people age. But this is difficult for older adults with dual sensory loss. One person told us
I don’t particularly want to mix with people. Too hard, because they can’t understand. I can no longer now walk into that room, see nothing, find my seat and not recognise [or hear] people.
Again, these experiences increase reliance on family. But caring in this context is tough and largely hidden. Family members describe being the “eyes and ears” for their loved one. It’s a 24/7 role which can bring frustration, social isolation and depression for carers too. One spouse told us:
He doesn’t talk anymore much, because he doesn’t know whether [people are] talking to him, unless they use his name, he’s unaware they’re speaking to him, so he might ignore people and so on. And in the end, I noticed people weren’t even bothering him to talk, so now I refuse to go. Because I don’t think it’s fair.
Dual sensory loss can be isolating for older people and carers. Synthex/Shutterstock So, what can we do?
Dual sensory impairment is a growing problem with potentially devastating impacts.
It should be considered a unique and distinct disability in all relevant protections and policies. This includes the right to dedicated diagnosis and support, accessibility provisions and specialised skill development for health and social professionals and carers.
We need to develop resources to help people with dual sensory impairment and their families and carers understand the condition, what it means and how everyone can be supported. This could include communication adaptation, such as social haptics (communicating using touch) and specialised support for older adults to navigate health care.
Increasing awareness and understanding of dual sensory impairment will also help those impacted with everyday engagement with the world around them – rather than the isolation many feel now.
Moira Dunsmore, Senior Lecturer, Sydney Nursing School, Faculty of Medicine and Health, University of Sydney, University of Sydney; Annmaree Watharow, Lived Experience Research Fellow, Centre for Disability Research and Policy, University of Sydney, and Emily Kecman, Postdoctoral research fellow, Department of Linguistics, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: