Terminal lucidity: why do loved ones with dementia sometimes ‘come back’ before death?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is often described as “the long goodbye”. Although the person is still alive, dementia slowly and irreversibly chips away at their memories and the qualities that make someone “them”.
Dementia eventually takes away the person’s ability to communicate, eat and drink on their own, understand where they are, and recognise family members.
Since as early as the 19th century, stories from loved ones, caregivers and health-care workers have described some people with dementia suddenly becoming lucid. They have described the person engaging in meaningful conversation, sharing memories that were assumed to have been lost, making jokes, and even requesting meals.
It is estimated 43% of people who experience this brief lucidity die within 24 hours, and 84% within a week.
Why does this happen?
Terminal lucidity or paradoxical lucidity?
In 2009, researchers Michael Nahm and Bruce Greyson coined the term “terminal lucidity”, since these lucid episodes often occurred shortly before death.
But not all lucid episodes indicate death is imminent. One study found many people with advanced dementia will show brief glimmers of their old selves more than six months before death.
Lucidity has also been reported in other conditions that affect the brain or thinking skills, such as meningitis, schizophrenia, and in people with brain tumours or who have sustained a brain injury.
Moments of lucidity that do not necessarily indicate death are sometimes called paradoxical lucidity. It is considered paradoxical as it defies the expected course of neurodegenerative diseases such as dementia.
But it’s important to note these episodes of lucidity are temporary and sadly do not represent a reversal of neurodegenerative disease.

Why does terminal lucidity happen?
Scientists have struggled to explain why terminal lucidity happens. Some episodes of lucidity have been reported to occur in the presence of loved ones. Others have reported that music can sometimes improve lucidity. But many episodes of lucidity do not have a distinct trigger.
A research team from New York University speculated that changes in brain activity before death may cause terminal lucidity. But this doesn’t fully explain why people suddenly recover abilities that were assumed to be lost.
Paradoxical and terminal lucidity are also very difficult to study. Not everyone with advanced dementia will experience episodes of lucidity before death. Lucid episodes are also unpredictable and typically occur without a particular trigger.
And as terminal lucidity can be a joyous time for those who witness the episode, it would be unethical for scientists to use that time to conduct their research. At the time of death, it’s also difficult for scientists to interview caregivers about any lucid moments that may have occurred.
Explanations for terminal lucidity extend beyond science. These moments of mental clarity may be a way for the dying person to say final goodbyes, gain closure before death, and reconnect with family and friends. Some believe episodes of terminal lucidity are representative of the person connecting with an afterlife.
Why is it important to know about terminal lucidity?
People can have a variety of reactions to seeing terminal lucidity in a person with advanced dementia. While some will experience it as being peaceful and bittersweet, others may find it deeply confusing and upsetting. There may also be an urge to modify care plans and request lifesaving measures for the dying person.
Being aware of terminal lucidity can help loved ones understand it is part of the dying process, acknowledge the person with dementia will not recover, and allow them to make the most of the time they have with the lucid person.
For those who witness it, terminal lucidity can be a final, precious opportunity to reconnect with the person that existed before dementia took hold and the “long goodbye” began.
Yen Ying Lim, Associate Professor, Turner Institute for Brain and Mental Health, Monash University and Diny Thomson, PhD (Clinical Neuropsychology) Candidate and Provisional Psychologist, Monash University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oral retinoids can harm unborn babies. But many women taking them for acne may not be using contraception
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Oral retinoids are a type of medicine used to treat severe acne. They’re sold under the brand name Roaccutane, among others.
While oral retinoids are very effective, they can have harmful effects if taken during pregnancy. These medicines can cause miscarriages and major congenital abnormalities (harm to unborn babies) including in the brain, heart and face. At least 30% of children exposed to oral retinoids in pregnancy have severe congenital abnormalities.
Neurodevelopmental problems (in learning, reading, social skills, memory and attention) are also common.
Because of these risks, the Australasian College of Dermatologists advises oral retinoids should not be prescribed a month before or during pregnancy under any circumstances. Dermatologists are instructed to make sure a woman isn’t pregnant before starting this treatment, and discuss the risks with women of childbearing age.
But despite this, and warnings on the medicines’ packaging, pregnancies exposed to oral retinoids continue to be reported in Australia and around the world.
In a study published this month, we wanted to find out what proportion of Australian women of reproductive age were taking oral retinoids, and how many of these women were using contraception.
Our results suggest a high proportion of women are not using effective contraception while on these drugs, indicating Australia needs a strategy to reduce the risk oral retinoids pose to unborn babies.
Contraception options
Using birth control to avoid pregnancy during oral retinoid treatment is essential for women who are sexually active. Some contraception methods, however, are more reliable than others.
Long-acting-reversible contraceptives include intrauterine devices (IUDs) inserted into the womb (such as Mirena, Kyleena, or copper devices) and implants under the skin (such as Implanon). These “set and forget” methods are more than 99% effective.
Oral retinoids taken during pregnancy can cause complications in babies. Gorodenkoff/Shutterstock The effectiveness of oral contraceptive pills among “perfect” users (following the directions, with no missed or late pills) is similarly more than 99%. But in typical users, this can fall as low as 91%.
Condoms, when used as the sole method of contraception, have higher failure rates. Their effectiveness can be as low as 82% in typical users.
Oral retinoid use over time
For our study, we analysed medicine dispensing data among women aged 15–44 from Australia’s Pharmaceutical Benefit Scheme (PBS) between 2013 and 2021.
We found the dispensing rate for oral retinoids doubled from one in every 71 women in 2013, to one in every 36 in 2021. The increase occurred across all ages but was most notable in young women.
Most women were not dispensed contraception at the same time they were using the oral retinoids. To be sure we weren’t missing any contraception that was supplied before the oral retinoids, we looked back in the data. For example, for an IUD that lasts five years, we looked back five years before the oral retinoid prescription.
Our analysis showed only one in four women provided oral retinoids were dispensed contraception simultaneously. This was even lower for 15- to 19-year-olds, where only about one in eight women who filled a prescription for oral retinoids were dispensed contraception.
A recent study found 43% of Australian year 10 and 69% of year 12 students are sexually active, so we can’t assume this younger age group largely had no need for contraception.
One limitation of our study is that it may underestimate contraception coverage, because not all contraceptive options are listed on the PBS. Those options not listed include male and female sterilisation, contraceptive rings, condoms, copper IUDs, and certain oral contraceptive pills.
But even if we presume some of the women in our study were using forms of contraception not listed on the PBS, we’re still left with a significant portion without evidence of contraception.
What are the solutions?
Other countries such as the United States and countries in Europe have pregnancy prevention programs for women taking oral retinoids. These programs include contraception requirements, risk acknowledgement forms and regular pregnancy tests. Despite these programs, unintended pregnancies among women using oral retinoids still occur in these countries.
But Australia has no official strategy for preventing pregnancies exposed to oral retinoids. Currently oral retinoids are prescribed by dermatologists, and most contraception is prescribed by GPs. Women therefore need to see two different doctors, which adds costs and burden.
Preventing pregnancy during oral retinoid treatment is essential. Krakenimages.com/Shutterstock Rather than a single fix, there are likely to be multiple solutions to this problem. Some dermatologists may not feel confident discussing sex or contraception with patients, so educating dermatologists about contraception is important. Education for women is equally important.
A clinical pathway is needed for reproductive-aged women to obtain both oral retinoids and effective contraception. Options may include GPs prescribing both medications, or dermatologists only prescribing oral retinoids when there’s a contraception plan already in place.
Some women may initially not be sexually active, but change their sexual behaviour while taking oral retinoids, so constant reminders and education are likely to be required.
Further, contraception access needs to be improved in Australia. Teenagers and young women in particular face barriers to accessing contraception, including costs, stigma and lack of knowledge.
Many doctors and women are doing the right thing. But every woman should have an effective contraception plan in place well before starting oral retinoids. Only if this happens can we reduce unintended pregnancies among women taking these medicines, and thereby reduce the risk of harm to unborn babies.
Dr Laura Gerhardy from NSW Health contributed to this article.
Antonia Shand, Research Fellow, Obstetrician, University of Sydney and Natasha Nassar, Professor of Paediatric and Perinatal Epidemiology and Chair in Translational Childhood Medicine, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
-
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Share This Post
-
Our Top 5 Spices: How Much Is Enough For Benefits?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A spoonful of pepper makes the… Hang on, no, that’s not right…
We know that spices are the spice of life, and many have great health-giving qualities. But…
- How much is the right amount?
- What’s the minimum to get health benefits?
- What’s the maximum to avoid toxicity?
That last one always seems like a scary question, but please bear in mind: everything is toxic at a certain dose. Oxygen, water, you-name-it.
On the other hand, many things have a toxicity so low that one could not physically consume it sufficiently faster than the body eliminates it, to get a toxic build-up.
Consider, for example, the €50 banknote that was nearly withdrawn from circulation because one of the dyes used in it was found to be toxic. However, the note remained in circulation after scientists patiently explained that a person would have to eat many thousands of them to get a lethal dose.
So, let’s address these questions in reverse order:
What’s the maximum to avoid toxicity?
In the case of the spices we’ll look at today, the human body generally* has high tolerance for them if eaten at levels that we find comfortable eating.
*IMPORTANT NOTE: If you have (or may have) a medical condition that may be triggered by spices, go easier on them (or if appropriate, abstain completely) after you learn about that.
Check with your own physician if unsure, because not only are we not doctors, we’re specifically not your doctors, and cannot offer personalized health advice.
We’re going to be talking in averages and generalizations here. Caveat consumator.
For most people, unless you are taking the spice in such quantities that you are folding space and seeing the future, or eating them as the main constituents of your meal rather than an embellishment, you should be fine. Please don’t enter a chilli-eating contest and sue us.
What is the minimum to get health benefits and how much should we eat?
The science of physiology generally involves continuous rather than discrete data, so there’s not so much a hard threshold, as a point at which the benefits become significant. The usefulness of most nutrients we consume, be they macro- or micro-, will tend to have a bell curve.
In other words, a tiny amount won’t do much, the right amount will have a good result, and usefulness will tail off after that point. To that end, we’re going to look at the “sweet spot” of peaking on the graph.
Also note: the clinical dose is the dose of the compound, not the amount of the food that one will need to eat to get that dose. For example, food x containing compound y will not usually contain that compound at 100% rate and nothing else. We mention this so that you’re not surprised when we say “the recommended dose is 5mg of compound, so take a teaspoon of this spice”, for example.
Further note: we only have so much room here, so we’re going to list only the top benefits, and not delve into the science of them. You can see the related main features for more details, though!
The “big 5” health-giving spices, with their relevant active compound:
- Black pepper (piperine)
- Hot pepper* (capsaicin)
- Garlic (allicin)
- Ginger (gingerol)
- Turmeric (curcumin**)
*Cayenne pepper is very high in capsaicin; chilli peppers are also great
**not the same thing as cumin, which is a completely different plant. Cumin does have some health benefits of its own, but not in the same league as the spices above, and there’s only so much we have room to cover today.
Black pepper
- Benefits: antioxidant, anti-cancer, boosts bioavailability of other nutrients, aids digestion
- Dosage: 5–20mg for benefits
- Suggestion: ½ teaspoon of black pepper is sufficient for benefits. However, this writer’s kitchen dictum in this case is “if you can’t see the black pepper in/on the food, add more”—but that’s more about taste!
- Related main feature: Black Pepper’s Anti-Cancer Arsenal (And More)
Hot Pepper
- Benefits: anti-inflammatory, metabolism accelerator
- Dosage: 6mg gives benefits, 500mg is a common dose in capsules
- Suggestion: if not making a spicy dish, consider using a teaspoon of cayenne as part of the seasoning for rice or potatoes
- Related main feature: Capsaicin For Weight Loss And Against Inflammation
Garlic
- Benefits: heart health, blood sugar balancing, anti-cancer
- Dosage: 4–8µg for benefits
- Suggestion: 1–2 cloves daily is generally good. However, cooking reduces allicin content (and so does oxidation after cutting/crushing), so you may want to adjust accordingly if doing those things.
- Related main feature: The Many Health Benefits Of Garlic
Ginger
- Benefits: anti-inflammatory, antioxidant, anti-nausea
- Dosage: 3–4g for benefits
- Suggestion: 1 teaspoon grated raw ginger or ½ a teaspoon powdered ginger, can be used in baking or as part of the seasoning for a stir-fry
- Related main feature: Ginger Does A Lot More Than You Think
Turmeric
- Benefits: anti-inflammatory, anti-cancer
- Dosage: 500–2000mg for benefits
- Suggestion: ¼ teaspoon per day is sufficient for benefits; ½ teaspoon dropped into the water when cooking rice will infuse the rice with turmeric (which is very water-soluble), turn the rice a pretty golden color, and not affect the flavor. Throw in some black pepper as it increases the bioavailability of curcumin up to 2000%
- Related main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Closing notes
The above five spices are very healthful for most people. Personal physiology can and will vary, so if in doubt, a) check with your doctor b) start at lowest doses and establish your tolerance (or lack thereof).
Enjoy, and stay well!
Share This Post
Related Posts
-
Why You Probably Need More Sleep
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sleep: yes, you really do still need it!
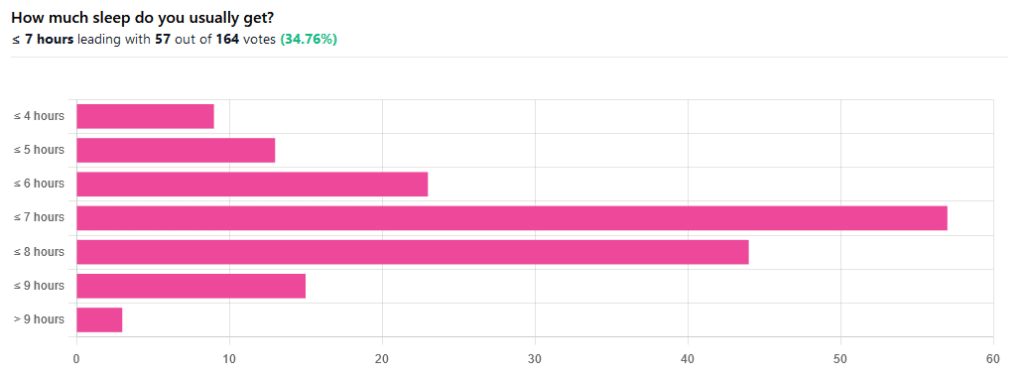
We asked you how much sleep you usually get, and got the above-pictured, below-described set of responses:
- A little of a third of all respondents selected the option “< 7 hours”
- However, because respondents also selected options such as < 6 hours, < 5 hours, and < 4 hours, so if we include those in the tally, the actual total percentage of respondents who reported getting under 7 hours, is actually more like 62%, or just under two thirds of all respondents.
- Nine respondents, which was about 5% of the total, reported usually getting under 4 hours sleep
- A little over quarter of respondents reported usually getting between 7 and 8 hours sleep
- Fifteen respondents, which was a little under 10% of the total, reported usually getting between 8 and 9 hours of sleep
- Three respondents, which was a little under 2% of the total, reported getting over 9 hours of sleep
- In terms of the classic “you should get 7–9 hours sleep”, approximately a third of respondents reported getting this amount.
You need to get 7–9 hours sleep: True or False?
True! Unless you have a (rare!) mutated ADRB1 gene, which reduces that.
The way to know whether you have this, without genomic testing to know for sure, is: do you regularly get under 6.5 hours sleep, and yet continue to go through life bright-eyed and bushy-tailed? If so, you probably have that gene. If you experience daytime fatigue, brain fog, and restlessness, you probably don’t.
About that mutated ADRB1 gene:
NIH | Gene identified in people who need little sleep
Quality of sleep matters as much as duration, and a lot of studies use the “RU-Sated” framework, which assesses six key dimensions of sleep that have been consistently associated with better health outcomes. These are:
- regularity / usual hours
- satisfaction with sleep
- alertness during waking hours
- timing of sleep
- efficiency of sleep
- duration of sleep
But, that doesn’t mean that you can skimp on the last one if the others are in order. In fact, getting a good 7 hours sleep can reduce your risk of getting a cold by three or four times (compared with six or fewer hours):
Behaviorally Assessed Sleep and Susceptibility to the Common Cold
^This study was about the common cold, but you may be aware there are more serious respiratory viruses freely available, and you don’t want those, either.
Napping is good for the health: True or False?
True or False, depending on how you’re doing it!
If you’re trying to do it to sleep less in total (per polyphasic sleep scheduling), then no, this will not work in any sustainable fashion and will be ruinous to the health. We did a Mythbusting Friday special on specifically this, a while back:
Could Just Two Hours Sleep Per Day Be Enough?
PS: you might remember Betteridge’s Law of Headlines
If you’re doing it as a energy-boosting supplement to a reasonable night’s sleep, napping can indeed be beneficial to the health, and can give benefits such as:
- Increased alertness
- Helps with learning
- Improved memory
- Boost to immunity
- Enhance athletic performance
However! There is still a right and a wrong way to go about it, and we wrote about this previously, for a Saturday Life Hacks edition of 10almonds:
How To Nap Like A Pro (No More “Sleep Hangovers”!)
As we get older, we need less sleep: True or False
False, with one small caveat.
The small caveat: children and adolescents need 9–12 hours sleep because, uncredited as it goes, they are doing some seriously impressive bodybuilding, and that is exhausting to the body. So, an adult (with a normal lifestyle, who is not a bodybuilder) will tend to need less sleep than a child/adolescent.
But, the statement “As we get older, we need less sleep” is generally taken to mean “People in the 65+ age bracket need less sleep than younger adults”, and this popular myth is based on anecdotal observational evidence: older people tend to sleep less (as our survey above shows! For any who aren’t aware, our readership is heavily weighted towards the 60+ demographic), and still continue functioning, after all.
Just because we survive something with a degree of resilience doesn’t mean it’s good for us.
In fact, there can be serious health risks from not getting enough sleep in later years, for example:
Sleep deficiency promotes Alzheimer’s disease development and progression
Want to get better sleep?
What gets measured, gets done. Sleep tracking apps can be a really good tool for getting one’s sleep on a healthier track. We compared and contrasted some popular ones:
The Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
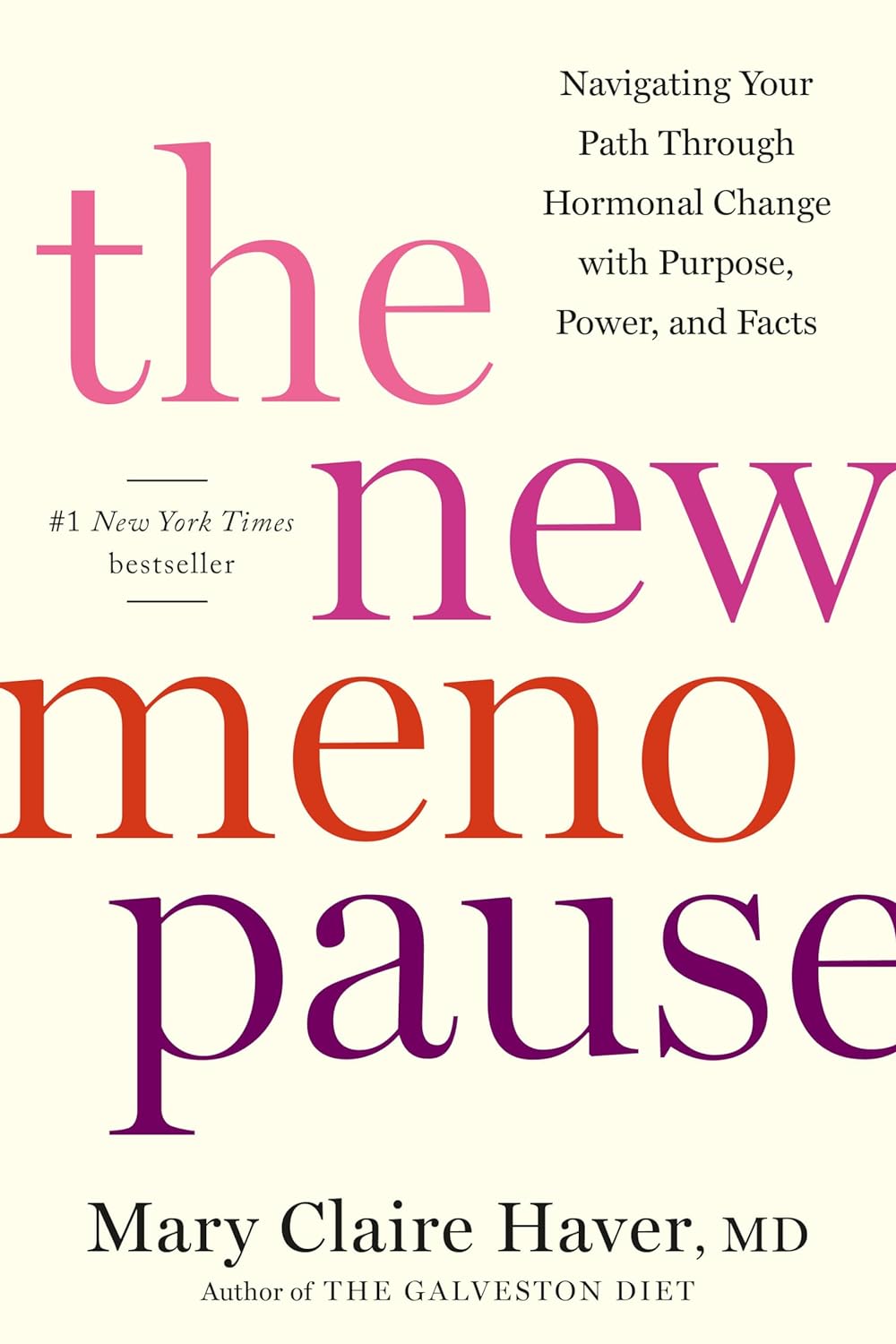
The New Menopause – by Dr. Mary Claire Haver
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author is most famous for “The Galveston Diet”, which book is astonishingly similar in its content, chapters, format, etc to Nikki Williams’ “It’s Not You, It’s Your Hormones” which came out a few years previously but didn’t get the same marketing.
Nonetheless, this time Dr. Haver has something new to add, and we think it’s worth a read.
The general theme of this book is a comprehensive overview of the menopause, experientially (subjective to the person going through it) and empirically (by science), from start to finish and beyond. This book’s more about human physiology, and less about diet than the previous.
Dr. Haver also discusses in-depth how estrogen is thought of as a sex hormone (and it is), to the point that people consider it perhaps expendable, and forget (or are simply unaware) that we have estrogen receptors throughout our bodies and estrogen is vital for maintaining many other bodily functions, including your heart, cognitive function, bone integrity, blood sugar balance, and more.
(in case you’re wondering “why don’t men fall to bits, then?”, don’t worry, their testosterone does these things for them. Testosterone is orders of magnitude less potent than estrogen, mg for mg, so they need a lot more of it, but under good conditions they produce plenty so it’s fine)
But, the amount of testosterone available to peri/postmenopausal women is simply not enough to do that job (and it’d also result in a transition of secondary sex characteristics, which for most people would be very unwanted), so, something else needs to be done.
Dr. Haver also discusses in detail the benefits and risks of HRT and how to get/manage them, respectively, with the latest up-to-date research (at time of going to print; the book was published in April 2024).
Bottom line: if you want to know what’s going on with your peri- or post-menopausal body and how it could be better (or if you want to know what’s going on with someone else approaching/experiencing menopause), then this is a top-tier book.
Click here to check out The New Menopause, and know what’s going on and what to do about it!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Modern Friendship – by Anna Goldfarb
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s a topic we’ve covered before at 10almonds: Human Connection In An All-Too-Busy World.
Here, however, Goldfarb has an entire book to cover what we had one article to cover, so of course it’s a lot more in-depth.
Importantly, if also covers: what if you seem to be doing everything right, and it’s still not working out? What if you’re already reaching out, suggesting things, doing your part?
Piece by piece, she uncovers what the very many problems are, ranging from availability issues and priorities, to health concerns and financial difficulties, to challenges as diverse as trust issues and exhaustion, and much more.
After all the hard truths about modern friendship, she gets onto equally cheery topics such as why friendships fail, but fear not, solutions are forthcoming too—and indeed, that’s what most of the book is about.
Covering such topics as desire, diligence, and delight, we learn how to not only practise wholehearted friendship, but also, how to matter to others, too. She finishes up with a “14-day friendship cleanse”, which sounds a lot more alarming than it actually is.
The style is interesting, being personal and, well, friendly throughout—but still with scholarly citations as we go along, and actual social science rather than mere conjecture.
Bottom line: if you find that your friendships are facing challenges, this book can help you to get to the bottom of any problems and move forwards (likely doing so together).
Click here to check out Modern Friendship, and learn how to truly nurture and grow your connections!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: