Stuck in fight-or-flight mode? 5 ways to complete the ‘stress cycle’ and avoid burnout or depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can you remember a time when you felt stressed leading up to a big life event and then afterwards felt like a weight had been lifted? This process – the ramping up of the stress response and then feeling this settle back down – shows completion of the “stress cycle”.
Some stress in daily life is unavoidable. But remaining stressed is unhealthy. Chronic stress increases chronic health conditions, including heart disease and stroke and diabetes. It can also lead to burnout or depression.
Exercise, cognitive, creative, social and self-soothing activities help us process stress in healthier ways and complete the stress cycle.
What does the stress cycle look like?
Scientists and researchers refer to the “stress response”, often with a focus on the fight-or-flight reactions. The phrase the “stress cycle” has been made popular by self-help experts but it does have a scientific basis.
The stress cycle is our body’s response to a stressful event, whether real or perceived, physical or psychological. It could be being chased by a vicious dog, an upcoming exam or a difficult conversation.
The stress cycle has three stages:
- stage 1 is perceiving the threat
- stage 2 is the fight-or-flight response, driven by our stress hormones: adrenaline and cortisol
- stage 3 is relief, including physiological and psychological relief. This completes the stress cycle.
Different people will respond to stress differently based on their life experiences and genetics.
Unfortunately, many people experience multiple and ongoing stressors out of their control, including the cost-of-living crisis, extreme weather events and domestic violence.
Remaining in stage 2 (the flight-or-flight response), can lead to chronic stress. Chronic stress and high cortisol can increase inflammation, which damages our brain and other organs.
When you are stuck in chronic fight-or-flight mode, you don’t think clearly and are more easily distracted. Activities that provide temporary pleasure, such as eating junk food or drinking alcohol are unhelpful strategies that do not reduce the stress effects on our brain and body. Scrolling through social media is also not an effective way to complete the stress cycle. In fact, this is associated with an increased stress response.
Stress and the brain
In the brain, chronic high cortisol can shrink the hippocampus. This can impair a person’s memory and their capacity to think and concentrate.
Chronic high cortisol also reduces activity in the prefrontal cortex but increases activity in the amygdala.
The prefrontal cortex is responsible for higher-order control of our thoughts, behaviours and emotions, and is goal-directed and rational. The amygdala is involved in reflexive and emotional responses. Higher amygdala activity and lower prefrontal cortex activity explains why we are less rational and more emotional and reactive when we are stressed.
There are five types of activities that can help our brains complete the stress cycle. https://www.youtube.com/embed/eD1wliuHxHI?wmode=transparent&start=0 It can help to understand how the brain encounters stress.
1. Exercise – its own complete stress cycle
When we exercise we get a short-term spike in cortisol, followed by a healthy reduction in cortisol and adrenaline.
Exercise also increases endorphins and serotonin, which improve mood. Endorphins cause an elated feeling often called “runner’s high” and have anti-inflammatory effects.
When you exercise, there is more blood flow to the brain and higher activity in the prefrontal cortex. This is why you can often think more clearly after a walk or run. Exercise can be a helpful way to relieve feelings of stress.
Exercise can also increase the volume of the hippocampus. This is linked to better short-term and long-term memory processing, as well as reduced stress, depression and anxiety.
2. Cognitive activities – reduce negative thinking
Overly negative thinking can trigger or extend the stress response. In our 2019 research, we found the relationship between stress and cortisol was stronger in people with more negative thinking.
Higher amygdala activity and less rational thinking when you are stressed can lead to distorted thinking such as focusing on negatives and rigid “black-and-white” thinking.
Activities to reduce negative thinking and promote a more realistic view can reduce the stress response. In clinical settings this is usually called cognitive behaviour therapy.
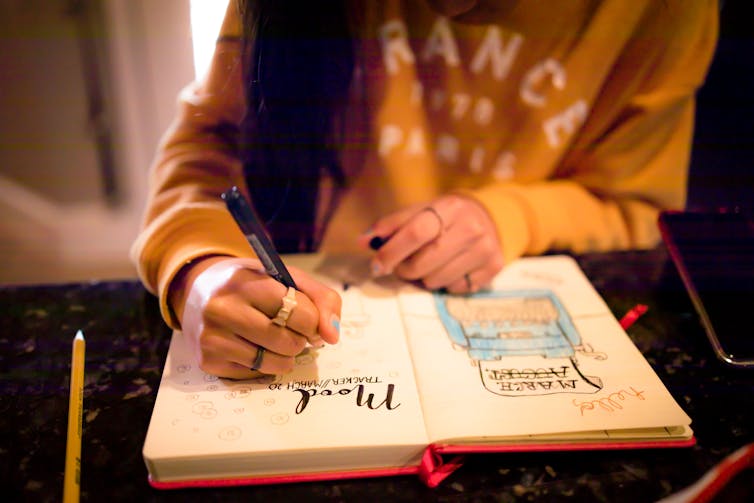
At home, this could be journalling or writing down worries. This engages the logical and rational parts of our brain and helps us think more realistically. Finding evidence to challenge negative thoughts (“I’ve prepared well for the exam, so I can do my best”) can help to complete the stress cycle.
3. Getting creative – a pathway out of ‘flight or fight’
Creative activities can be art, craft, gardening, cooking or other activities such as doing a puzzle, juggling, music, theatre, dancing or simply being absorbed in enjoyable work.
Such pursuits increase prefrontal cortex activity and promote flow and focus.
Flow is a state of full engagement in an activity you enjoy. It lowers high-stress levels of noradrenaline, the brain’s adrenaline. When you are focussed like this, the brain only processes information relevant to the task and ignores non-relevant information, including stresses.
4. Getting social and releasing feel-good hormones
Talking with someone else, physical affection with a person or pet and laughing can all increase oxytocin. This is a chemical messenger in the brain that increases social bonding and makes us feel connected and safe.
Laughing is also a social activity that activates parts of the limbic system – the part of the brain involved in emotional and behavioural responses. This increases endorphins and serotonin and improves our mood.
5. Self-soothing
Breathing exercises and meditation stimulate the parasympathetic nervous system (which calms down our stress responses so we can “reset”) via the vagus nerves, and reduce cortisol.
A good cry can help too by releasing stress energy and increasing oxytocin and endorphins.
Emotional tears also remove cortisol and the hormone prolactin from the body. Our prior research showed cortisol and prolactin were associated with depression, anxiety and hostility.

Action beats distraction
Whether it’s watching a funny or sad movie, exercising, journalling, gardening or doing a puzzle, there is science behind why you should complete the stress cycle.
Doing at least one positive activity every day can also reduce our baseline stress level and is beneficial for good mental health and wellbeing.
Importantly, chronic stress and burnout can also indicate the need for change, such as in our workplaces. However, not all stressful circumstances can be easily changed. Remember help is always available.
If you have concerns about your stress or health, please talk to a doctor.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14 or Kids Helpline on 1800 55 1800.
Theresa Larkin, Associate professor of Medical Sciences, University of Wollongong and Susan J. Thomas, Associate professor in Mental Health and Behavioural Science, University of Wollongong
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Astaxanthin: Super-Antioxidant & Neuroprotectant
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Think Pink For Brain Health!
Astaxanthin is a carotenoid that’s found in:
- certain marine microalgae
- tiny crustaceans that eat the algae
- fish (and flamingos!) that eat the crustaceans
Yes, it’s the one that makes things pink.
But it does a lot more than that…
Super-antioxidant
Move over, green tea! Astaxanthin has higher antioxidant activity than most carotenoids. For example, it is 2–5 times more effective than alpha-carotene, lutein, beta-carotene, and lycopene:
Antioxidant activities of astaxanthin and related carotenoids
We can’t claim credit for naming it a super-antioxidant though, because:
Astaxanthin: A super antioxidant from microalgae and its therapeutic potential
Grow new brain cells
Axtaxanthin is a neuroprotectant, but that’s to be expected from something with such a powerful antioxidant ability.
What’s more special to astaxanthin is that it assists continued adult neurogenesis (creation of new brain cells):
❝The unique chemical structure of astaxanthin enables it to cross the blood-brain barrier and easily reach the brain, where it may positively influence adult neurogenesis.
Furthermore, astaxanthin appears to modulate neuroinflammation by suppressing the NF-κB pathway, reducing the production of pro-inflammatory cytokines, and limiting neuroinflammation associated with aging and chronic microglial activation.
By modulating these pathways, along with its potent antioxidant properties, astaxanthin may contribute to the restoration of a healthy neurogenic microenvironment, thereby preserving the activity of neurogenic niches during both normal and pathological aging. ❞
That first part is very important, by the way! There are so many things that our brain needs, and we can eat, but the molecules are unable to pass the blood-brain barrier, meaning they either get wasted, or used elsewhere, or dismantled for their constituent parts. In this case, it zips straight into the brain instead.
See also:
How To Grow New Brain Cells (At Any Age)
(Probably) good for the joints, too
First, astaxanthin got a glowing report in a study we knew not to trust blindly:
…and breathe. What a title that was! But, did you catch why it’s not to be trusted blindly? It was down at the bottom…
❝Conflict of interest statement
NOVAREX Co., Ltd. funded the study. Valensa International provided the FlexPro MD® ingredients, and NOVAREX Co., Ltd. encapsulated the test products (e.g., both FlexPro MD® and placebo)❞
Studies where a supplement company funded the study are not necessarily corrupt, but they can certainly sway publication bias, i.e. the company funds a bunch of studies and then pulls funding from the ones that aren’t going the way it wants.
So instead let’s look at:
Astaxanthin attenuates joint inflammation induced by monosodium urate crystals
and
Astaxanthin ameliorates cartilage damage in experimental osteoarthritis
…which had no such conflicts of interest.
They agree that astaxanthin indeed does the things (attenuates joint inflammation & ameliorates cartilage damage).
However, they are animal studies (rats), so we’d like to see studies with humans to be able to say for sure how much it helps these things.
Summary of benefits
Based on the available research, astaxanthin…
- is indeed a super-antioxidant
- is a neuroprotective agent
- also assists adult neurogenesis
- is probablygood for joints too
How much do I take, and is it safe?
A 2019 safety review concluded:
❝Recommended or approved doses varied in different countries and ranged between 2 and 24 mg.
We reviewed 87 human studies, none of which found safety concerns with natural astaxanthin supplementation, 35 with doses ≥12 mg/day.❞
Source: Astaxanthin: How much is too much? A safety review
In short: for most people, it’s very safe and well-tolerated. If you consume it to an extreme, you will likely turn pink, much as you would turn orange if you did the same thing with carrots. But aside from that, the risks appear to be minimal.
However! If you have a seafood allergy, please take care to get a supplement that’s made from microalgae, not one that’s made from krill or other crustaceans, or from other creatures that eat those.
Where can I get it?
We don’t sell it, but here’s an example product on Amazon, for your convenience
Enjoy!
Share This Post
-
Collard Greens vs Watercress – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
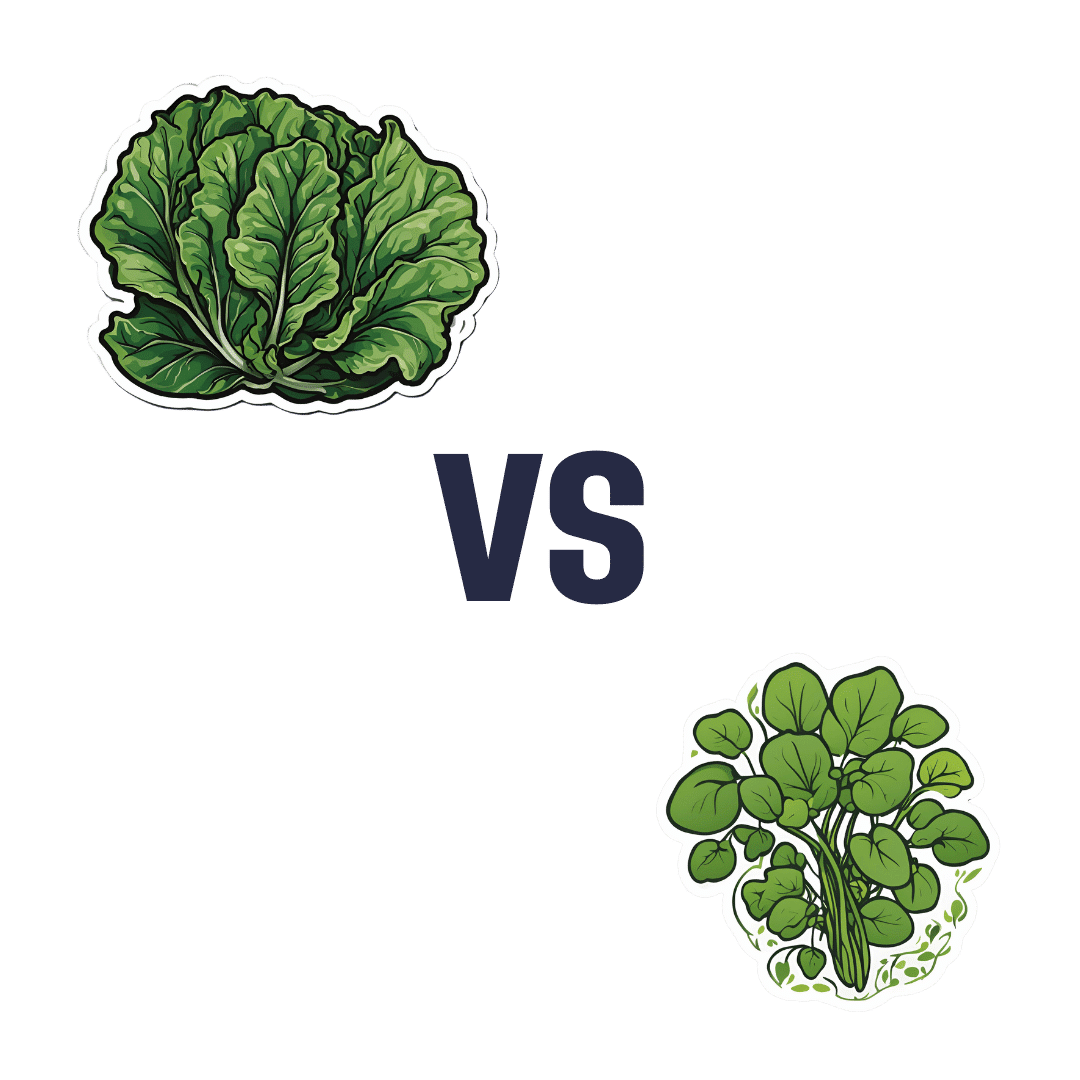
When comparing collard greens to watercress, we picked the collard greens.
Why?
It was close! But…
In terms of macros, collard greens have 8x the fiber, 4x the carbs, and slightly more protein. The fiber-to-carbs ratio also gives collard greens the lower glycemic index, although honestly, nobody is getting metabolic disease from eating watercress. Still, by the numbers it’s a clear win for collard greens, and especially 8x the fiber is not to be undervalued!
When it comes to vitamins, things were much more even; collard greens have more of vitamins A, B3, B9, K, and choline, while watercress has more of vitamins B1, B2, B5, C, and E. They’re tied on vitamin B6, so that makes a 5.5:5.5 tie overall. Looking for a tiebreaker, collard greens’ margins of difference are greater, so we could call this a tie or the narrowest of wins for collard greens ion this category.
In the category of minerals, collard greens have more calcium, copper, iron, manganese, and zinc, while watercress has more copper, phosphorus, potassium, and selenium. They’re tied on magnesium. This time the margins of difference are also comparable, so there’s really no tiebreaker available for this one. Thus, an absolute tie on minerals.
Looking at polyphenols, watercress has slightly more, with the main contender being 4mg/100g quercetin.
Adding up the sections results in either a tie or a slight for collard greens based on the tiebreaker in the vitamins category.
We can also put the two clear wins (one for collard greens and one for watercress), and say that in our opinion, collard greens’ 4g/100g fiber beats watercress’s 4mg/100g quercetin.
Quercetin is great and all, but:
- if you buy a quercetin supplement like this one on Amazon it’s 1000mg capsules, so how critical is watercress’s 4mg, really? Yes, getting it from food is better, but it’s not 25,000% better.
- no doctor that we know of is saying “you need more quercetin or you’re going to die”, but they do say “you need more fiber or you’re going to die”
- indeed, the WHO passionately proclaims that 95% of people in the US especially desperately need to eat more fiber, whereas there is no similar giant public health campaign begging people to have 4mg more of quercetin
…so we’ll say that’s another tiebreaker in favor of collard greens.
In short: collard greens scrape a win based on several tiebreakers, but watercress was a very close contender indeed!
Of course, by all means enjoy either or (ideally!) both; diversity is good.
Want to learn more?
You might like:
What’s Your Plant Diversity Score?
Enjoy!
Share This Post
-
The Other Alzheimer’s Risk Factor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The usually-listed 7 known risk factors of dementia (in general, not just Alzheimer’s) do not include today’s item. For a recap, those were:
The 7 Known Risk Factors For Dementia
The bonus risk factor
This idea is not completely novel; it’s been known for a while that traumatic brain injury (TBI) can increase the risk of dementia, but it has generally been chalked up to “if you damage an organ, then that organ does not function so well afterwards”.
However, in the case of Alzheimer’s, it seems there’s something deeper at play. Specifically, a study that found…
❝…traumatic brain injury alters the small vessels in the brain, resulting in an accumulation of amyloid beta—a hallmark of Alzheimer’s disease.
The findings suggest that vascular dysfunction could be an early driver in neurodegenerative disorders rather than being caused by neuronal damage.❞
This association held true even in quite young patients!
The study from Sweden looked at brain tissue from TBI patients (who had had to have brain tissue removed for medical reasons due to bleeding and swelling), and found that the (traumatic) changes to the vascular smooth muscle cells were associated with increased aggregation of amyloid-β.
In terms of establishing cause and effect: since it could be safely concluded the amyloid-β had not caused the TBI (which all had external explanations such as “car crash” or such), it can be deduced that almost* certainly the TBI caused the amyloid-β aggregation.
*because little to nothing in science is every truly certain. As in life in general, really; the difference is that scientists admit it!
You may be wondering: what was the control? It would be a very generous group of citizens indeed who would volunteer bits of their brains that hadn’t needed removing. However, the answer is that the control brain bits came from a biobank, and were from uninjured patients with no history of TBI or neurodegenerative disorders, and who had died from systemic, unrelated causes. Having been dead for a matter of hours, and the fixation time for the brain bits from the living people taking long enough that everybody’s brain bits had been out of their respective living bodies for a similar length of time, this was deemed an acceptable, if imperfect, control.
You can read the study in its entirety here; it is fascinating:
The practical take-away
The practical take-away, of course, is: look after your brain
Not just in the sense of eat fiber, get healthy fats, move more, get good sleep, stay intellectually stimulated, etc*, but also in the sense of “keep your brain physically safe”.
Now, you may think that you already try not to get into car crashes, and perhaps you do not compete in contact sports, but do be aware that one of the leading causes of TBI in older people is, ignominiously, falling down.
And if you think “that only happens to older/other people”, then be aware: there’s a first time for everything and you are not immune. With that in mind, do check out:
Fall Special! ← the seasonal title notwithstanding, this is about not falling down in the first place, and being less injurable if you do fall down
*This was a modest and vague list for brevity’s sake, so for much more detail, enjoy:
How To Reduce Your Alzheimer’s Risk ← this is rather more comprehensive
Want to know more?
Here you can read about the largest study of its kind into lifestyle factors and Alzheimer’s disease:
Alzheimer’s Causative Factors To Avoid ← the methods and conclusions of Dr. David Snowdon’s famous “Nun Study”
Take care!
Share This Post
Related Posts
-
Eggcellent News Against Dementia?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s that time of the week again… We hope all our readers have had a great and healthy week! Here are some selections from health news from around the world:
Moderation remains key
Eggs have come under the spotlight for their protective potential against dementia, largely due to their content of omega-3 fatty acids, choline, and other nutrients.
Nevertheless, the study had some limitations (including not measuring the quantity of eggs consumed, just the frequency), and while eating eggs daily showed the lowest rates of dementia, not eating them at all did not significantly alter the risk.
Eating more than 2 eggs per day is still not recommended, however, for reasons of increasing the risk of other health issues, such as heart disease.
Read in full: Could eating eggs prevent dementia?
Related: Eggs: Nutritional Powerhouse or Heart-Health Timebomb?
More than suitable
It’s common for a lot of things to come with the warning “not suitable for those who are pregnant or nursing”, with such frequency that it can be hard to know what one can safely do/take while pregnant or nursing.
In the case of COVID vaccines, though, nearly 90% of babies who had to be hospitalized with COVID-19 had mothers who didn’t get the vaccine while they were pregnant.
And as for how common that is: babies too young to be vaccinated (so, under 6 months) had the highest covid hospitalization rate of any age group except people over 75.
Read in full: Here’s why getting a covid shot during pregnancy is important
Related: The Truth About Vaccines
Positive dieting
Adding things into one’s diet is a lot more fun than taking things out, is generally easier to sustain, and (as a general rule of thumb; there are exceptions of course) give the greatest differences in health outcomes.
This is perhaps most true of beans and pulses, which add many valuable vitamins, minerals, protein, and perhaps most importantly of all (single biggest factor in reducing heart disease risk), fiber.
Read in full: Adding beans and pulses can lead to improved shortfall nutrient intakes and a higher diet quality in American adults
Related: Intuitive Eating Might Not Be What You Think
Clearing out disordered thinking
Hoarding is largely driven by fear of loss, and this radical therapy tackles that at the root, by such means as rehearsing alternative outcomes of discarding through imagery rescripting, and examining the barriers to throwing things away—to break down those barriers one at a time.
Read in full: Hoarding disorder: sensory CBT treatment strategy shows promise
Related: When You Know What You “Should” Do (But Knowing Isn’t The Problem)
Superfluous
Fluoridated water may not be as helpful for the teeth as it used to be prior to about 1975. Not because it became any less effective per se, but because of the modern prevalence of fluoride-containing toothpastes, mouthwashes, etc rendering it redundant in more recent decades.
Read in full: Dental health benefits of fluoride in water may have declined, study finds
Related: Water Fluoridation, Atheroma, & More
Off-label?
With rising costs of living including rising healthcare costs, and increasing barriers to accessing in-person healthcare, it’s little wonder that many are turning to the gray market online to get their medications.
These websites typically use legal loopholes to sell prescription drugs to the public, by employing morally flexible doctors who are content to expediently rubber-stamp prescriptions upon request, on the basis of the patient having filled out a web form and checked boxes for their symptoms (and of course also having waived all rights of complaint or legal recourse).
However, some less scrupulous sorts are exploiting this market, to sell outright fake medications, using a setup that looks like a “legitimate” gray market website. Caveat emptor indeed.
Read in full: CDC warns of fake drug dangers from online pharmacies
Related: Are You Taking PIMs? Getting Off The Overmedication Train
A rising threat
In 2021 (we promise the paper was published only a few days ago!), the leading causes of death were:
- COVID-19
- Heart disease
- Stroke
…which latter represented a rising threat, likely in part due to the increase in the aging population.
Read in full: Stroke remains a leading cause of death globally, with increased risk linked to lifestyle factors
Related: 6 Signs Of Stroke (One Month In Advance)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
14 Powerful Strategies To Prevent Dementia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia risk starts climbing very steeply after the age of 65, but it’s not entirely predetermined. Dr. Brad Stanfield, a primary care physician, has insights:
The strategies
We’ll not keep them a mystery; they are:
- Cognitive stimulation: which means genuinely challenging mental activities using a variety of mental faculties. This will usually mean that anything that is just “same old, same old” all the time will stop giving benefits after a short while once it becomes rote, and you’ll need something harder and/or different.
- Hearing health: being unable to participate in conversations increases dementia risk; hearing aids can help.
- Eyesight health: similar to the above; regular eye tests are good, and the use of glasses where appropriate.
- Depression management: midlife depression is linked to later life dementia, likely in large part due to social isolation and a lack of stimulation, but either way, treating depression earlier reduces later dementia risk.
- Exercising regularly: what’s good for the heart is good for the brain; the brain is a hungry organ and the blood is what feeds it (and removes things that shouldn’t be there)
- Head injury avoidance: even mild head injuries can cause problems down the road. Protecting one’s head in sports, and even while casually cycling, is important.
- Smoking cessation: just don’t smoke; if you smoke, make it a top priority to quit unless you are given direct strong medical advice to the contrary (there are cases, few and far between, whereby quitting smoking genuinely needs to be deferred until after something else is dealt with first, but they are a lot rarer than a lot of people who are simply afraid of quitting would like to believe)
- Cholesterol management: again, healthy blood means a healthy brain, and that goes for triglycerides too.
- Weight management: obesity, especially waist to hip ratio (indicating visceral abdominal fat specifically) is associated with many woes, including dementia.
- Diabetes management: once again, healthy blood means a healthy brain, and that goes for blood sugar management too.
- Blood pressure management: guess what, healthy blood still means a healthy brain, and that goes for blood pressure too.
- Alcohol reduction/cessation: alcohol is bad for pretty much everything, and for most people who drink, quitting is probably the top thing to do after quitting smoking.
- Social engagement: while we all may have our different preferences on a scale of introversion to extroversion, we are fundamentally a social species and thrive best with social contact, even if it’s just a few people.
- Air pollution reduction: avoiding pollutants, and filtering the air we breathe where pollutants are otherwise unavoidable, makes a measurable difference to brain health outcomes.
For more information on all of these (except the last two, which really he only mentions in passing), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Reduce Your Alzheimer’s Risk ← our own main feature on the topic
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
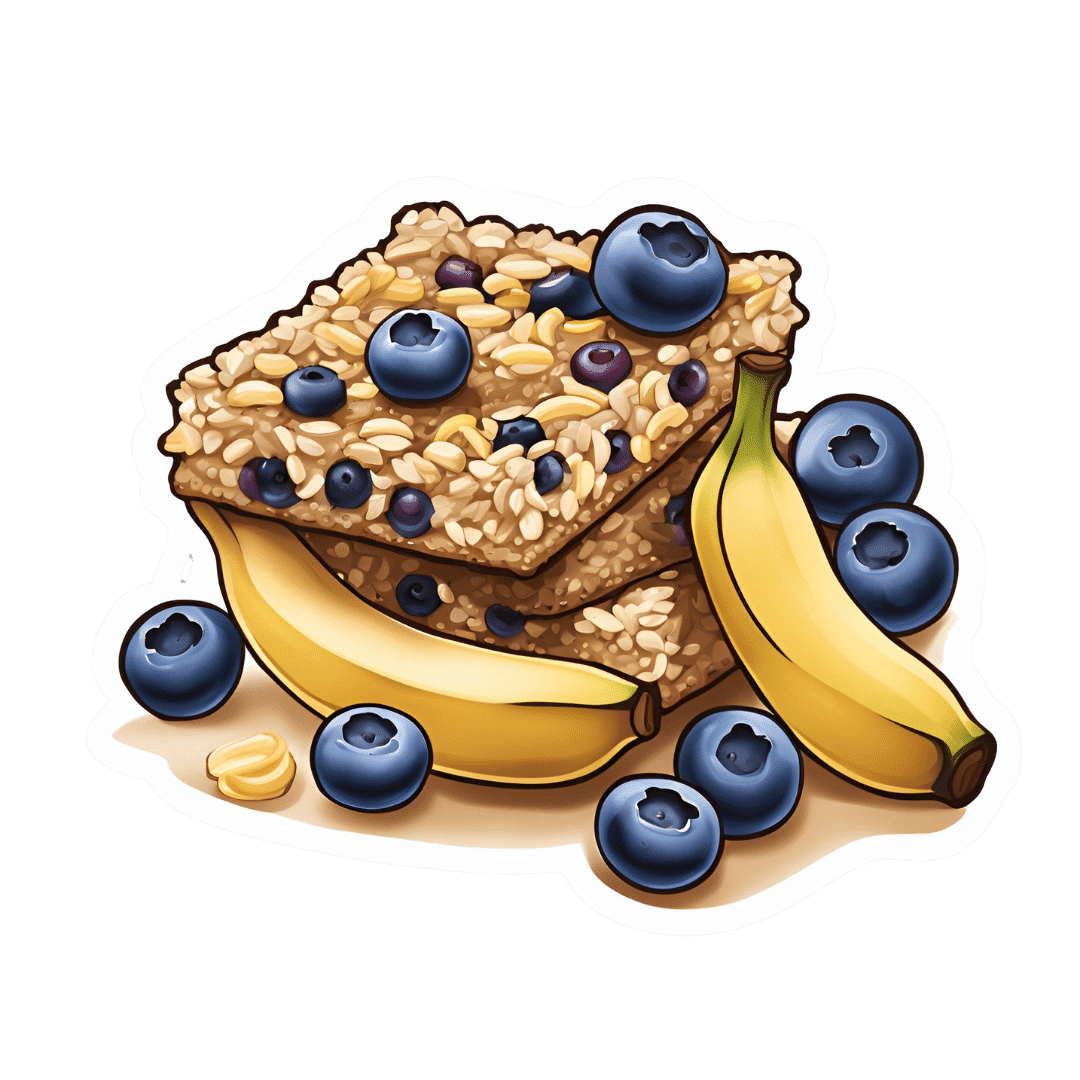
Blueberry & Banana Collagen Baked Oats
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Good news for vegans/vegetarians! While we include an optional tablespoon of collagen powder in this recipe, the whole recipe is already geared around collagen synthesis, so it’s very collagen-boosting even with just the plants, providing collagen’s building blocks of protein, zinc, and vitamins C and D (your miraculous body will use these to assemble the collagen inside you).
You will need
- 2 cups oats, whence the protein and zinc
- 1 cup milk (your preference what kind; we recommend almond for flavor; whether you choose plant or animal though, it should be fortified with vitamin D)
- 2 bananas, peeled and mashed
- 4 oz blueberries, whence the vitamin C (frozen is fine) (chopped dried apricots are also a fine substitute if that’s more convenient)
- 1 oz flaked almonds, whence the protein and zinc
- 1 tbsp pumpkin seeds, whence the protein and zinc
- 1 tbsp flax seeds, whence the protein and zinc
- Optional: 1 tbsp maple syrup
- Optional: 1 tbsp collagen powder, dissolved in 1 oz hot water
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Mix the oats with 2 cups boiling water; allow to stand for 10–15 minutes, and then drain any excess water.
3) Mix the mashed bananas with the remaining ingredients except the milk and blueberries, stirring thoroughly.
4) Add the softened oats, and stir those in thoroughly too.
5) Add the milk and blueberries, in that order, stirring gently if using fresh blueberries, lest they get crushed.
6) Pour the mixture into an 8″ square cake tin that you have lined with baking paper, and smooth the top.
7) Bake for about 40 minutes or until firm and golden brown. Allow to cool; it will firm up more while it does.
8) Cut into squares or bars, and serve or store for later.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
We Are Such Stuff As Fish Are Made Of ← our main feature about collagen
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: