Stretching & Mobility – by James Atkinson
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“I will stretch for just 10 minutes per day”, we think, and do our best. Then there are a plethora of videos saying “Stretching mistakes that you are making!” and it turns out we haven’t been doing them in a way that actually helps.
This book fixes that. Unlike some books of the genre, it’s not full of jargon and you won’t need an anatomy and physiology degree to understand it. It is, however, dense in terms of the information it gives—it’s not padded out at all; it contains a lot of value.
The stretches are all well-explained and well-illustrated; the cover art will give you an idea of the anatomical illustration style contained with in.
Atkinson also gives workout plans, so that we know we’re not over- or under-training or trying to do too much or missing important things out.
Bottom line: if you’re looking to start a New Year routine to develop better suppleness, this book is a great primer for that.
Click here to check out Stretching and Mobility, and improve yours!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Superfood Broccoli Pesto
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cruciferous vegetables have many health benefits of their own (especially: a lot of anticancer benefits). But, it can be hard to include them in every day’s menu, so this is just one more way that’ll broaden your options! It’s delicious mixed into pasta, or served as a dip, or even on toast.
You will need
- 4 cups small broccoli florets
- 1 cup fresh basil leaves
- ½ cup pine nuts
- ¼ bulb garlic
- 3 tbsp extra virgin olive oil
- 2 tbsp nutritional yeast
- 1 tbsp lemon juice
- 2 tsp black pepper, coarse ground
- 1 tsp red pepper flakes
- ½ tsp MSG or 1 tsp low-sodium salt
Method
(we suggest you read everything at least once before doing anything)
1) Steam the broccoli for 3–5 minutes. Allow to cool.
2) Blend the pine nuts, garlic, lemon juice, and nutritional yeast.
3) Add the broccoli, basil, olive oil, black pepper, red pepper, and MSG or salt, and blend in the food processor again until well-combined.
4) Serve:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Broccoli vs Cauliflower – Which is Healthier?
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Herbs for (Evidence-Based) Health & Healing ← Basil features here! It’s easy to think that medicinal herbs have to be some kind of arcane obscurity, but it’s often not so.
- Our Top 5 Spices: How Much Is Enough For Benefits? ← Black pepper, red pepper, and garlic all feature here
- All About Olive Oil: Is “Extra Virgin” Worth It?
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
-
Digital Minimalism – by Dr. Cal Newport
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are a lot of books that advise “Unplug once in a while, and go outside”. But it doesn’t really take a book to convey that, does it? And it just leaves all the digital catching-up once we get back. Surely there must be a better way?
Rather than relying on a “digital detox”, Dr. Newport offers principles to apply to our digital lives, that allow us to reap the benefits of modern information technology without being obeisant to it.
The book’s greatest strength lies in that; having clear guidelines that can be applied to cut out the extra weight of digital media that has simply snuck in because of The Almighty Algorithm—and even tips on how to engage more mindfully with that if we still want to, for example using social media only in a web browser rather than on our phones, so that we can ringfence the time for it rather than having it spill into every spare moment.
In the category of criticism, the book sometimes lacks a little awareness when it comes to assumptions about the reader and the reader’s social circles; that (for example) nobody has any disabilities and everyone lives in the same town. But for most people most of the time, the advices will stand, and the exceptions can be managed by the reader neatly enough.
Stylistically, the book is not very minimalist, but this is not inconsistent with the advice of the book, if you’re curling up in the armchair with a physical copy, or a single-purpose ereader device.
Bottom line: if you’d like to streamline your use of digital media, but don’t want to lose out on the value it brings you, this book provides an excellent template
Click here to check out Digital Minimalism, and choose focused life in a noisy world!
Share This Post
-
Genetic Risk Factors For Long COVID
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people, after getting COVID, go on to have Long COVID. There are various contributing factors to this, including:
- Lifestyle factors that impact general disease-proneness
- Immune-specific factors such as being immunocompromised already
- Genetic factors
We looked at some modifiable factors to improve one’s disease-resistance, yesterday:
And we’ve taken a more big-picture look previously:
Beyond Supplements: The Real Immune-Boosters!
Along with some more systemic issues:
Why Some People Get Sick More (And How To Not Be One Of Them)
But, for when the “don’t get COVID” ship has sailed, one of the big remaining deciding factors with regard to whether one gets Long COVID or not, is genetic
The Long COVID Genes
For those with their 23andMe genetic data to hand…
❝Study findings revealed that three specific genetic loci, HLA-DQA1–HLA-DQB1, ABO, and BPTF–KPAN2–C17orf58, and three phenotypes were at significantly heightened risk, highlighting high-priority populations for interventions against this poorly understood disease.❞
For those who don’t, then first: you might consider getting that! Here’s why:
Genetic Testing: Health Benefits & Methods
But also, all is not lost meanwhile:
The same study also found that individuals with genetic predispositions to chronic fatigue, depression, and fibromyalgia, as well as other phenotypes such as autoimmune conditions and cardiometabolic conditions, are at significantly higher risk of long-COVID than individuals without these conditions.
Good news, bad news
Another finding was that women and non-smokers were more likely to get Long COVID, than men and smokers, respectively.
Does that mean that those things are protective against Long COVID, which would be very counterintuitive in the case of smoking?
Well, yes and no; it depends on whether you count “less likely to get Long COVID because of being more likely to just die” as protective against Long COVID.
(Incidentally, estrogen is moderately immune-enhancing, while testosterone is moderately immune-suppressing, so the sex thing was not too surprising. It’s also at least contributory to why women get more autoimmune disorders, while men get more respiratory infections such as colds and the like)
Want to know more?
You can read the paper itself, here:
*GWAS = Genome-Wide Association Study
Take care!
Share This Post
Related Posts
-
The Whys and Hows of Cutting Meats Out Of Your Diet
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it’s time to tell the meat to beat it…
Meat in general, and red meat and processed meat in particular, have been associated with so many health risks, that it’s very reasonable to want to reduce, if not outright eliminate, our meat consumption.
First, in case anyone’s wondering “what health risks?”
The aforementioned culprits tend to turn out to be a villain in the story of every second health-related thing we write about here. To name just a few:
- Processed Meat Consumption and the Risk of Cancer: A Critical Evaluation of the Constraints of Current Evidence from Epidemiological Studies
- Red Meat Consumption (Heme Iron Intake) and Risk for Diabetes and Comorbidities?
- Health Risks Associated with Meat Consumption: A Review of Epidemiological Studies
- Associations of Processed Meat, Unprocessed Red Meat, Poultry, or Fish Intake With Incident Cardiovascular Disease and All-Cause Mortality
- Meat consumption: Which are the current global risks? A review of recent (2010-2020) evidences
Seasoned subscribers will know that we rarely go more than a few days without recommending the very science-based Mediterranean Diet which studies find beneficial for almost everything we write about. The Mediterranean Diet isn’t vegetarian per se—by default it consists of mostly plants but does include some fish and a very small amount of meat from land animals. But even that can be improved upon:
- A Pesco-Mediterranean Diet With Intermittent Fasting
- Mediterranean, vegetarian and vegan diets as practical outtakes of EAS and ACC/AHA recommendations for lowering lipid profile
- A Mediterranean Low-Fat Vegan Diet to Improve Body Weight and Cardiometabolic Risk Factors: A Randomized, Cross-over Trial
So that’s the “why”; now for the “how”…
It’s said that with a big enough “why” you can always find a “how”, but let’s make things easy!
Meatless Mondays
One of the biggest barriers to many people skipping the meat is “what will we even eat?”
The idea of “Meatless Mondays” means that this question need only be answered once a week, and in doing that a few Mondays in a row, you’ll soon find you’re gradually building your repertoire of meatless meals, and finding it’s not so difficult after all.
Then you might want to expand to “meat only on the weekends”, for example.
Flexitarian
This can be met with derision, “Yes and I’m teetotal, apart from wine”, but there is a practical aspect here:
The idea is “I will choose vegetarian options, unless it’s really inconvenient for me to do so”, which wipes out any difficulty involved.
After doing this for a while, you might find that as you get more used to vegetarian stuff, it’s almost never inconvenient to eat vegetarian.
Then you might want to expand it to “I will choose vegan options, unless it’s really inconvenient for me to do so”
Like-for-like substitutions
Pretty much anything that can come from an animal, one can get a plant-based version of it nowadays. The healthiness (and cost!) of these substitutions can vary, but let’s face it, meat is neither the healthiest nor the cheapest thing out there these days either.
If you have the money and don’t fancy leaping to lentils and beans, this can be a very quick and easy zero-effort change-over. Then once you’re up and running, maybe you can—at your leisure—see what all the fuss is about when it comes to tasty recipes with lentils and beans!
That’s all we have time for today, but…
We’re thinking of doing a piece making your favorite recipes plant-based (how to pick the right substitutions so the meal still tastes and “feels” the same), so let us know if you’d like that? Feel free to mention your favorite foods/meals too, as that’ll help us know what there’s a market for!
You can do that by hitting reply to any of our emails, or using the handy feedback widget at the bottom!
Curious to know more while you wait?
Check out: The Vegan Diet: A Complete Guide for Beginners ← this is a well-sourced article from Healthline, who—just like us—like to tackle important health stuff in an easy-to-read, well-sourced format
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What happens in my brain when I get a migraine? And what medications can I use to treat it?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Migraine is many things, but one thing it’s not is “just a headache”.
“Migraine” comes from the Greek word “hemicrania”, referring to the common experience of migraine being predominantly one-sided.
Some people experience an “aura” preceding the headache phase – usually a visual or sensory experience that evolves over five to 60 minutes. Auras can also involve other domains such as language, smell and limb function.
Migraine is a disease with a huge personal and societal impact. Most people cannot function at their usual level during a migraine, and anticipation of the next attack can affect productivity, relationships and a person’s mental health.
Francisco Gonzelez/Unsplash What’s happening in my brain?
The biological basis of migraine is complex, and varies according to the phase of the migraine. Put simply:
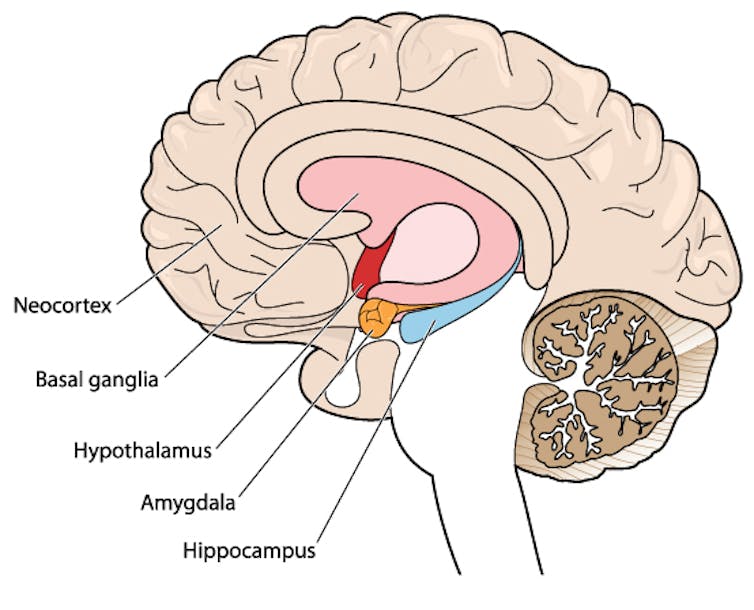
The earliest phase is called the prodrome. This is associated with activation of a part of the brain called the hypothalamus which is thought to contribute to many symptoms such as nausea, changes in appetite and blurred vision.
The hypothalamus is shown here in red. Blamb/Shutterstock Next is the aura phase, when a wave of neurochemical changes occur across the surface of the brain (the cortex) at a rate of 3–4 millimetres per minute. This explains how usually a person’s aura progresses over time. People often experience sensory disturbances such as flashes of light or tingling in their face or hands.
In the headache phase, the trigeminal nerve system is activated. This gives sensation to one side of the face, head and upper neck, leading to release of proteins such as CGRP (calcitonin gene-related peptide). This causes inflammation and dilation of blood vessels, which is the basis for the severe throbbing pain associated with the headache.
Finally, the postdromal phase occurs after the headache resolves and commonly involves changes in mood and energy.
What can you do about the acute attack?
A useful way to conceive of migraine treatment is to compare putting out campfires with bushfires. Medications are much more successful when applied at the earliest opportunity (the campfire). When the attack is fully evolved (into a bushfire), medications have a much more modest effect.
Aspirin
For people with mild migraine, non-specific anti-inflammatory medications such as high-dose aspirin, or standard dose non-steroidal medications (NSAIDS) can be very helpful. Their effectiveness is often enhanced with the use of an anti-nausea medication.
Triptans
For moderate to severe attacks, the mainstay of treatment is a class of medications called “triptans”. These act by reducing blood vessel dilation and reducing the release of inflammatory chemicals.
Triptans vary by their route of administration (tablets, wafers, injections, nasal sprays) and by their time to onset and duration of action.
The choice of a triptan depends on many factors including whether nausea and vomiting is prominent (consider a dissolving wafer or an injection) or patient tolerability (consider choosing one with a slower onset and offset of action).
As triptans constrict blood vessels, they should be used with caution (or not used) in patients with known heart disease or previous stroke.
Triptans should be used cautiously in patients with heart disease. CDC/Unsplash Gepants
Some medications that block or modulate the release of CGRP, which are used for migraine prevention (which we’ll discuss in more detail below), also have evidence of benefit in treating the acute attack. This class of medication is known as the “gepants”.
Gepants come in the form of injectable proteins (monoclonal antibodies, used for migraine prevention) or as oral medication (for example, rimegepant) for the acute attack when a person has not responded adequately to previous trials of several triptans or is intolerant of them.
They do not cause blood vessel constriction and can be used in patients with heart disease or previous stroke.
Ditans
Another class of medication, the “ditans” (for example, lasmiditan) have been approved overseas for the acute treatment of migraine. Ditans work through changing a form of serotonin receptor involved in the brain chemical changes associated with the acute attack.
However, neither the gepants nor the ditans are available through the Pharmaceutical Benefits Scheme (PBS) for the acute attack, so users must pay out-of-pocket, at a cost of approximately A$300 for eight wafers.
What about preventing migraines?
The first step is to see if lifestyle changes can reduce migraine frequency. This can include improving sleep habits, routine meal schedules, regular exercise, limiting caffeine intake and avoiding triggers such as stress or alcohol.
Despite these efforts, many people continue to have frequent migraines that can’t be managed by acute therapies alone. The choice of when to start preventive treatment varies for each person and how inclined they are to taking regular medication. Those who suffer disabling symptoms or experience more than a few migraines a month benefit the most from starting preventives.
Some people will take medicines to prevent migraines. Tbel Abuseridze/Unsplash Almost all migraine preventives have existing roles in treating other medical conditions, and the physician would commonly recommend drugs that can also help manage any pre-existing conditions. First-line preventives include:
- tablets that lower blood pressure (candesartan, metoprolol, propranolol)
- antidepressants (amitriptyline, venlafaxine)
- anticonvulsants (sodium valproate, topiramate).
Some people have none of these other conditions and can safely start medications for migraine prophylaxis alone.
For all migraine preventives, a key principle is starting at a low dose and increasing gradually. This approach makes them more tolerable and it’s often several weeks or months until an effective dose (usually 2- to 3-times the starting dose) is reached.
It is rare for noticeable benefits to be seen immediately, but with time these drugs typically reduce migraine frequency by 50% or more.
‘Nothing works for me!’
In people who didn’t see any effect of (or couldn’t tolerate) first-line preventives, new medications have been available on the PBS since 2020. These medications block the action of CGRP.
The most common PBS-listed anti-CGRP medications are injectable proteins called monoclonal antibodies (for example, galcanezumab and fremanezumab), and are self-administered by monthly injections.
These drugs have quickly become a game-changer for those with intractable migraines. The convenience of these injectables contrast with botulinum toxin injections (also effective and PBS-listed for chronic migraine) which must be administered by a trained specialist.
Up to half of adolescents and one-third of young adults are needle-phobic. If this includes you, tablet-form CGRP antagonists for migraine prevention are hopefully not far away.
Data over the past five years suggest anti-CGRP medications are safe, effective and at least as well tolerated as traditional preventives.
Nonetheless, these are used only after a number of cheaper and more readily available first-line treatments (all which have decades of safety data) have failed, and this also a criterion for their use under the PBS.
Mark Slee, Associate Professor, Clinical Academic Neurologist, Flinders University and Anthony Khoo, Lecturer, Flinders University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Is chocolate milk a good recovery drink after a workout? A dietitian reviews the evidence
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Whether you enjoy chocolate milk regularly, as a weekend treat, or as an occasional dose of childhood nostalgia, it probably wouldn’t be the first option you think of for post-workout recovery.
Unless you’re on TikTok, perhaps. According to many people on the social media platform, chocolate milk is not only delicious, but it offers benefits comparable to sports drinks after a workout.
So is there any evidence to support this? Let’s take a look.
eldar nurkovic/Shutterstock Rehydrating after a workout is important
Water accounts for somewhere between 50% and 60% of our body weight. Water has many important functions in the body, including helping to keep our body at the right temperature through sweating.
We lose water naturally from our bodies when we sweat, as well as through our breathing and when we go to the toilet. So it’s important to stay hydrated to replenish the water we lose.
When we don’t, we become dehydrated, which can put a strain on our bodies. Signs and symptoms of dehydration can range from thirst and dizziness to low blood pressure and confusion.
Athletes, because of their higher levels of exertion, lose more water through sweating and from respiration (when their breathing rate gets faster). If they’re training or competing in hot or humid environments they will sweat even more.
Dehydration impacts athletes’ performance and like for all of us, can affect their health.
So finding ways to ensure athletes rehydrate quickly during and after they train or compete is important. Fortunately, sports scientists and dietitians have done research looking at the composition of different fluids to understand which ones rehydrate athletes most effectively.
The beverage hydration index
The best hydrating drinks are those the body retains the most of once they’ve been consumed. By doing studies where they give people different drinks in standardised conditions, scientists have been able to determine how various options stack up.
To this end, they’ve developed something called the beverage hydration index, which measures to what degree different fluids hydrate a person compared to still water.
According to this index beverages with similar fluid retention to still water include sparkling water, sports drinks, cola, diet cola, tea, coffee, and beer below 4% alcohol. That said, alcohol is probably best avoided when recovering from exercise.
Beverages with superior fluid retention to still water include milk (both full-fat and skim), soy milk, orange juice and oral rehydration solutions.
This body of research indicates that when it comes to rehydration after exercise, unflavoured milk (full fat, skim or soy) is better than sports drinks.
But what about chocolate milk?
A small study looked at the effects of chocolate milk compared to plain milk on rehydration and exercise performance in futsal players (futsal is similar to soccer but played on a court indoors). The researchers found no difference in rehydration between the two. There’s no other published research to my knowledge looking at how chocolate milk compares to regular milk for rehydration during or after exercise.
But rehydration isn’t the only thing athletes look for in sports drinks. In the same study, drinking chocolate milk after play (referred to as the recovery period) increased the time it took for the futsal players to become exhausted in further exercise (a shuttle run test) four hours later.
This was also shown in a review of several clinical trials. The analysis found that, compared to different placebos (such as water) or other drinks containing fat, protein and carbohydrates, chocolate milk lengthened the time to exhaustion during exercise.
What’s in chocolate milk?
Milk contains protein, carbohydrates and electrolytes, each of which can affect hydration, performance, or both.
Protein is important for building muscle, which is beneficial for performance. The electrolytes in milk (including sodium and potassium) help to replace electrolytes lost through sweating, so can also be good for performance, and aid hydration.
Compared to regular milk, chocolate milk contains added sugar. This provides extra carbohydrates, which are likewise beneficial for performance. Carbohydrates provide an immediate source of energy for athletes’ working muscles, where they’re stored as glycogen. This might contribute to the edge chocolate milk appears to have over plain milk in terms of athletic endurance.
The added sugar in chocolate milk provides extra carbohydrates. Brent Hofacker/Shutterstock Coffee-flavoured milk has an additional advantage. It contains caffeine, which can improve athletic performance by reducing the perceived effort that goes into exercise.
One study showed that a frappe-type drink prepared with filtered coffee, skim milk and sugar led to better muscle glycogen levels after exercise compared to plain milk with an equivalent amount of sugar added.
So what’s the verdict?
Evidence shows chocolate milk can rehydrate better than water or sports drinks after exercise. But there isn’t evidence to suggest it can rehydrate better than plain milk. Chocolate milk does appear to improve athletic endurance compared to plain milk though.
Ultimately, the best drink for athletes to consume to rehydrate is the one they’re most likely to drink.
While many TikTok trends are not based on evidence, it seems chocolate milk could actually be a good option for recovery from exercise. And it will be cheaper than specialised sports nutrition products. You can buy different brands from the supermarket or make your own at home with a drinking chocolate powder.
This doesn’t mean everyone should look to chocolate milk when they’re feeling thirsty. Chocolate milk does have more calories than plain milk and many other drinks because of the added sugar. For most of us, chocolate milk may be best enjoyed as an occasional treat.
Evangeline Mantzioris, Program Director of Nutrition and Food Sciences, Accredited Practising Dietitian, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: