Steps vs Cardio | Which is Best for Fat Loss, Health, & Performance?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
“Move more”, they say; but does it matter how quickly?
Use it or lose it
For general performance:
- More steps per day do offer slight aerobic benefits but do not significantly improve endurance.
- Higher-intensity cardio (ideally, HIIT) is essential for improving aerobic fitness.
- Training should match endurance goals (e.g. long-distance running vs team sports vs whatever it is that you care about for you).
For general health:
- Both cardio and step tracking reduce mortality risk and improve longevity.
- 2–3 hours of cardio per week provides most health benefits, with diminishing returns after 8 hours per week.
- 10,000+ steps/day is optimal, but 5,000+ steps/day still benefits health. And, not mentioned in this video, but really (per science) there seem to be diminishing returns after about 8,000 steps per day.
Fun fact: the reason it’s 10,000 steps per day that everyone talks about as the default goal, is just because the Japanese person who popularized it noted that the kanji for 10,000 looks a bit like a walking person: 万
For fat loss:
- Both step tracking and cardio do help.
- Step tracking better reflects total daily movement, while cardio burns calories in sessions—but if it’s not HIIT, there is likely to be a compensatory metabolic slump afterwards.
- High-intensity cardio increases fatigue, which may impact resistance training and diet adherence.
- Excessive endurance training can slightly inhibit muscle growth, but low-intensity steps have minimal interference.
So for fat loss, it’s best to get those steps in, and throw in a few HIIT sessions per week, with adequate recovery time between them.
For more on all of these things, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
How To Do HIIT (Without Wrecking Your Body)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Olive Oil vs Coconut Oil – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing extra virgin olive oil to cold-pressed coconut oil, we picked the olive oil.
Why?
While the cold-pressed coconut oil may offer some health benefits due to its lauric acid content, its 80–90% saturated fat content isn’t great for most people. It’s a great oil when applied topically for healthy skin and hair, though!
The extra virgin olive oil has a much more uncontroversially healthy blend of triglycerides, and (in moderation) is universally recognized as very heart-healthy.
Your local supermarket, most likely, has a good extra virgin olive oil, but if you’d like to get some online, here’s an example product on Amazon for your convenience.
Share This Post
-
Ear Candling: Is It Safe & Does It Work?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Does This Practice Really Hold A Candle To Evidence-Based Medicine?
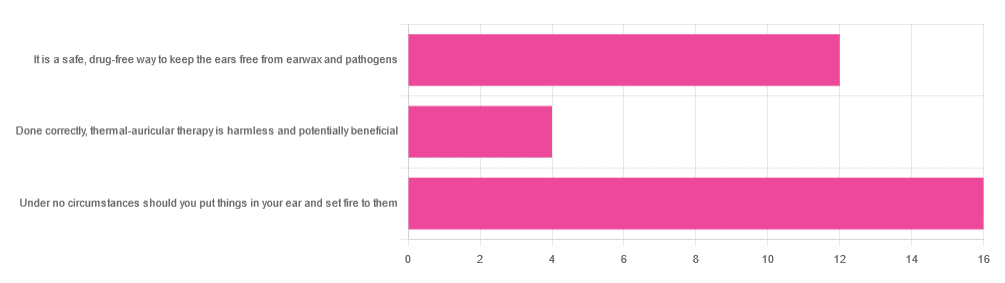
In Tuesday’s newsletter, we asked you your opinion of ear candling, and got the above-depicted, below-described set of responses:
- Exactly 50% said “Under no circumstances should you put things in your ear and set fire to them”
- About 38% said “It is a safe, drug-free way to keep the ears free from earwax and pathogens”
- About 13% said “Done correctly, thermal-auricular therapy is harmless and potentially beneficial”
This means that if we add the two positive-to-candling answers together, it’s a perfect 50:50 split between “do it” and “don’t do it”.
(Yes, 38%+13%=51%, but that’s because we round to the nearest integer in these reports, and more precisely it was 37.5% and 12.5%)
So, with the vote split, what does the science say?
First, a quick bit of background: nobody seems keen to admit to having invented this. One of the major manufacturers of ear candles refers to them as “Hopi” candles, which the actual Hopi tribe has spent a long time asking them not to do, as it is not and never has been used by the Hopi people. Other proposed origins offered by advocates of ear candling include Traditional Chinese Medicine (not used), Ancient Egypt (no evidence of such whatsoever), and Atlantis:
Quackwatch | Why Ear Candling Is Not A Good Idea
It is a safe, drug-free way to keep the ears free from earwax and pathogens: True or False?
False! In a lot of cases of alternative therapy claims, there’s an absence of evidence that doesn’t necessarily disprove the treatment. In this case, however, it’s not even an open matter; its claims have been actively disproven by experimentation:
- It doesn’t remove earwax; on the contrary, experimentation “showed no removal of cerumen from the external auditory canal. Candle wax was actually deposited in some“
- It doesn’t remove pathogens, and the proposed mechanism of action for removing pathogens, that of the “chimney effect”: the idea that the burning candle creates a vacuum that draws wax out of the ear along with debris and bacteria, simply does not work; on the contrary, “Tympanometric measurements in an ear canal model demonstrated that ear candles do not produce negative pressure”.
- It isn’t safe; on the contrary, “Ear candles have no benefit in the management of cerumen and may result in serious injury”
In a medium-sized survey (n=122), the following injuries were reported:
- 13 x burns
- 7 x occlusion of the ear canal
- 6 x temporary hearing loss
- 3 x otitis externa (this also called “swimmer’s ear”, and is an inflammation of the ear, accompanied by pain and swelling)
- 1 x tympanic membrane perforation
Indeed, authors of one paper concluded:
❝Ear candling appears to be popular and is heavily advertised with claims that could seem scientific to lay people. However, its claimed mechanism of action has not been verified, no positive clinical effect has been reliably recorded, and it is associated with considerable risk.
No evidence suggests that ear candling is an effective treatment for any condition. On this basis, we believe it can do more harm than good and we recommend that GPs discourage its use❞
Source: Canadian Family Physician | Ear Candling
Under no circumstances should you put things in your ear and set fire to them: True or False?
True! It’s generally considered good advice to not put objects in general in your ears.
Inserting flaming objects is a definite no-no. Please leave that for the Cirque du Soleil.
You may be thinking, “but I have done this and suffered no ill effects”, which seems reasonable, but is an example of survivorship bias in action—it doesn’t make the thing in question any safer, it just means you were one of the one of the ones who got away unscathed.
If you’re wondering what to do instead… Ear oils can help with the removal of earwax (if you don’t want to go get it sucked out at a clinic—the industry standard is to use a suction device, which actually does what ear candles claim to do). For information on safely getting rid of earwax, see our previous article:
Take care!
Share This Post
-
10 Mistakes To Sabotage Your Ozempic Progress
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Ozempic has a good reputation for getting reliable results, but there are ways to mess it up:
It’s not just inject-and-go
We’ll not keep the 10 ways a secret; they are:
- Increasing the dose too quickly: avoid cranking doses up too high too quickly, to prevent severe nausea, appetite suppression, and muscle loss. It’s worth being aware that high doses without proper management can lead to metabolic health disasters.
- Pushing through side effects: severe nausea or vomiting means you probably have an unhelpfully high dose; consult your prescribing doctor—it’s easy to feel “more is better; I don’t want to have less!”, but there really is a sweet spot, and if you’re not in it, then adjustments are needed in order to find it.
- Eating nutritionally scant food: reducing the quantity of unhealthy food isn’t enough—please prioritize nutrient-rich foods instead. Remember, “it’s not the calories in your food; it’s the food in your calories”.
- Consuming fried food and refined carbs: their general metabolic woes aside, fried foods and ultra-refined carbs can exacerbate nausea and other side effects, so it really is best to skip them. The good news is that Ozempic will help overcome those cravings more easily.
- Neglecting muscle protection: especially women, especially middle-aged or older, are at higher risk of osteoporosis and should maintain muscle mass (strong muscles and strong bones go together, by necessity). So, eat protein and do resistance training!
- Assuming it’s a monotherapy: GLP-1 drugs work best as part of a holistic protocol, including proper nutrition, strength training, and hormone therapy if appropriate.
- Not addressing metabolic health first: GLP-1 drugs are less effective in people with poor baseline metabolic health, so there’s a bit of a catch-22 here, but it’s important to be aware of. Fortunately, Ozempic and adopting a healthy lifestyle will each make the other work better.
- Neglecting comprehensive treatment plans: in other words, going through the motions of a holistic protocol and then expecting Ozempic to do all the work.
- Upping doses to overcome plateaus: plateaus often signal other issues (e.g. lack of protein, no strength training), so do address these before increasing dosage.
- Lack of collaboration with doctors: the human body is complex, and what’s going on metabolically is complex too, so there’s a lot a layperson can easily miss. For that matter, there’s a lot that doctors can easily miss too, but more heads are better than one.
For more on all of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like:
5 Ways To Naturally Boost The Ozempic Effect
Take care!
Share This Post
Related Posts
-
Rapid Rise in Syphilis Hits Native Americans Hardest
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
From her base in Gallup, New Mexico, Melissa Wyaco supervises about two dozen public health nurses who crisscross the sprawling Navajo Nation searching for patients who have tested positive for or been exposed to a disease once nearly eradicated in the U.S.: syphilis.
Infection rates in this region of the Southwest — the 27,000-square-mile reservation encompasses parts of Arizona, New Mexico, and Utah — are among the nation’s highest. And they’re far worse than anything Wyaco, who is from Zuni Pueblo (about 40 miles south of Gallup) and is the nurse consultant for the Navajo Area Indian Health Service, has seen in her 30-year nursing career.
Syphilis infections nationwide have climbed rapidly in recent years, reaching a 70-year high in 2022, according to the most recent data from the Centers for Disease Control and Prevention. That rise comes amid a shortage of penicillin, the most effective treatment. Simultaneously, congenital syphilis — syphilis passed from a pregnant person to a baby — has similarly spun out of control. Untreated, congenital syphilis can cause bone deformities, severe anemia, jaundice, meningitis, and even death. In 2022, the CDC recorded 231 stillbirths and 51 infant deaths caused by syphilis, out of 3,761 congenital syphilis cases reported that year.
And while infections have risen across the U.S., no demographic has been hit harder than Native Americans. The CDC data released in January shows that the rate of congenital syphilis among American Indians and Alaska Natives was triple the rate for African Americans and nearly 12 times the rate for white babies in 2022.
“This is a disease we thought we were going to eradicate not that long ago, because we have a treatment that works really well,” said Meghan Curry O’Connell, a member of the Cherokee Nation and chief public health officer at the Great Plains Tribal Leaders’ Health Board, who is based in South Dakota.
Instead, the rate of congenital syphilis infections among Native Americans (644.7 cases per 100,000 people in 2022) is now comparable to the rate for the entire U.S. population in 1941 (651.1) — before doctors began using penicillin to cure syphilis. (The rate fell to 6.6 nationally in 1983.)
O’Connell said that’s why the Great Plains Tribal Leaders’ Health Board and tribal leaders from North Dakota, South Dakota, Nebraska, and Iowa have asked federal Health and Human Services Secretary Xavier Becerra to declare a public health emergency in their states. A declaration would expand staffing, funding, and access to contact tracing data across their region.
“Syphilis is deadly to babies. It’s highly infectious, and it causes very severe outcomes,” O’Connell said. “We need to have people doing boots-on-the-ground work” right now.
In 2022, New Mexico reported the highest rate of congenital syphilis among states. Primary and secondary syphilis infections, which are not passed to infants, were highest in South Dakota, which had the second-highest rate of congenital syphilis in 2022. In 2021, the most recent year for which demographic data is available, South Dakota had the second-worst rate nationwide (after the District of Columbia) — and numbers were highest among the state’s large Native population.
In an October news release, the New Mexico Department of Health noted that the state had “reported a 660% increase in cases of congenital syphilis over the past five years.” A year earlier, in 2017, New Mexico reported only one case — but by 2020, that number had risen to 43, then to 76 in 2022.
Starting in 2020, the covid-19 pandemic made things worse. “Public health across the country got almost 95% diverted to doing covid care,” said Jonathan Iralu, the Indian Health Service chief clinical consultant for infectious diseases, who is based at the Gallup Indian Medical Center. “This was a really hard-hit area.”
At one point early in the pandemic, the Navajo Nation reported the highest covid rate in the U.S. Iralu suspects patients with syphilis symptoms may have avoided seeing a doctor for fear of catching covid. That said, he doesn’t think it’s fair to blame the pandemic for the high rates of syphilis, or the high rates of women passing infections to their babies during pregnancy, that continue four years later.
Native Americans are more likely to live in rural areas, far from hospital obstetric units, than any other racial or ethnic group. As a result, many do not receive prenatal care until later in pregnancy, if at all. That often means providers cannot test and treat patients for syphilis before delivery.
In New Mexico, 23% of patients did not receive prenatal care until the fifth month of pregnancy or later, or received fewer than half the appropriate number of visits for the infant’s gestational age in 2023 (the national average is less than 16%).
Inadequate prenatal care is especially risky for Native Americans, who have a greater chance than other ethnic groups of passing on a syphilis infection if they become pregnant. That’s because, among Native communities, syphilis infections are just as common in women as in men. In every other ethnic group, men are at least twice as likely to contract syphilis, largely because men who have sex with men are more susceptible to infection. O’Connell said it’s not clear why women in Native communities are disproportionately affected by syphilis.
“The Navajo Nation is a maternal health desert,” said Amanda Singer, a Diné (Navajo) doula and lactation counselor in Arizona who is also executive director of the Navajo Breastfeeding Coalition/Diné Doula Collective. On some parts of the reservation, patients have to drive more than 100 miles to reach obstetric services. “There’s a really high number of pregnant women who don’t get prenatal care throughout the whole pregnancy.”
She said that’s due not only to a lack of services but also to a mistrust of health care providers who don’t understand Native culture. Some also worry that providers might report patients who use illicit substances during their pregnancies to the police or child welfare. But it’s also because of a shrinking network of facilities: Two of the Navajo area’s labor and delivery wards have closed in the past decade. According to a recent report, more than half of U.S. rural hospitals no longer offer labor and delivery services.
Singer and the other doulas in her network believe New Mexico and Arizona could combat the syphilis epidemic by expanding access to prenatal care in rural Indigenous communities. Singer imagines a system in which midwives, doulas, and lactation counselors are able to travel to families and offer prenatal care “in their own home.”
O’Connell added that data-sharing arrangements between tribes and state, federal, and IHS offices vary widely across the country, but have posed an additional challenge to tackling the epidemic in some Native communities, including her own. Her Tribal Epidemiology Center is fighting to access South Dakota’s state data.
In the Navajo Nation and surrounding area, Iralu said, IHS infectious disease doctors meet with tribal officials every month, and he recommends that all IHS service areas have regular meetings of state, tribal, and IHS providers and public health nurses to ensure every pregnant person in those areas has been tested and treated.
IHS now recommends all patients be tested for syphilis yearly, and tests pregnant patients three times. It also expanded rapid and express testing and started offering DoxyPEP, an antibiotic that transgender women and men who have sex with men can take up to 72 hours after sex and that has been shown to reduce syphilis transmission by 87%. But perhaps the most significant change IHS has made is offering testing and treatment in the field.
Today, the public health nurses Wyaco supervises can test and treat patients for syphilis at home — something she couldn’t do when she was one of them just three years ago.
“Why not bring the penicillin to the patient instead of trying to drag the patient in to the penicillin?” said Iralu.
It’s not a tactic IHS uses for every patient, but it’s been effective in treating those who might pass an infection on to a partner or baby.
Iralu expects to see an expansion in street medicine in urban areas and van outreach in rural areas, in coming years, bringing more testing to communities — as well as an effort to put tests in patients’ hands through vending machines and the mail.
“This is a radical departure from our past,” he said. “But I think that’s the wave of the future.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
California Becomes Latest State To Try Capping Health Care Spending
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
California’s Office of Health Care Affordability faces a herculean task in its plan to slow runaway health care spending.
The goal of the agency, established in 2022, is to make care more affordable and accessible while improving health outcomes, especially for the most disadvantaged state residents. That will require a sustained wrestling match with a sprawling, often dysfunctional health system and powerful industry players who have lots of experience fighting one another and the state.
Can the new agency get insurers, hospitals, and medical groups to collaborate on containing costs even as they jockey for position in the state’s $405 billion health care economy? Can the system be transformed so that financial rewards are tied more to providing quality care than to charging, often exorbitantly, for a seemingly limitless number of services and procedures?
The jury is out, and it could be for many years.
California is the ninth state — after Connecticut, Delaware, Massachusetts, Nevada, New Jersey, Oregon, Rhode Island, and Washington — to set annual health spending targets.
Massachusetts, which started annual spending targets in 2013, was the first state to do so. It’s the only one old enough to have a substantial pre-pandemic track record, and its results are mixed: The annual health spending increases were below the target in three of the first five years and dropped beneath the national average. But more recently, health spending has greatly increased.
In 2022, growth in health care expenditures exceeded Massachusetts’ target by a wide margin. The Health Policy Commission, the state agency established to oversee the spending control efforts, warned that “there are many alarming trends which, if unaddressed, will result in a health care system that is unaffordable.”
Neighboring Rhode Island, despite a preexisting policy of limiting hospital price increases, exceeded its overall health care spending growth target in 2019, the year it took effect. In 2020 and 2021, spending was largely skewed by the pandemic. In 2022, the spending increase came in at half the state’s target rate. Connecticut and Delaware, by contrast, both overshot their 2022 targets.
It’s all a work in progress, and California’s agency will, to some extent, be playing it by ear in the face of state policies and demographic realities that require more spending on health care.
And it will inevitably face pushback from the industry as it confronts unreasonably high prices, unnecessary medical treatments, overuse of high-cost care, administrative waste, and the inflationary concentration of a growing number of hospitals in a small number of hands.
“If you’re telling an industry we need to slow down spending growth, you’re telling them we need to slow down your revenue growth,” says Michael Bailit, president of Bailit Health, a Massachusetts-based consulting group, who has consulted for various states, including California. “And maybe that’s going to be heard as ‘we have to restrain your margins.’ These are very difficult conversations.”
Some of California’s most significant health care sectors have voiced disagreement with the fledgling affordability agency, even as they avoid overtly opposing its goals.
In April, when the affordability office was considering an annual per capita spending growth target of 3%, the California Hospital Association sent it a letter saying hospitals “stand ready to work with” the agency. But the proposed number was far too low, the association argued, because it failed to account for California’s aging population, new investments in Medi-Cal, and other cost pressures.
The hospital group suggested a spending increase target averaging 5.3% over five years, 2025-29. That’s slightly higher than the 5.2% average annual increase in per capita health spending over the five years from 2015 to 2020.
Five days after the hospital association sent its letter, the affordability board approved a slightly less aggressive target that starts at 3.5% in 2025 and drops to 3% by 2029. Carmela Coyle, the association’s chief executive, said in a statement that the board’s decision still failed to account for an aging population, the growing need for mental health and addiction treatment, and a labor shortage.
The California Medical Association, which represents the state’s doctors, expressed similar concerns. The new phased-in target, it said, was “less unreasonable” than the original plan, but the group would “continue to advocate against an artificially low spending target that will have real-life negative impacts on patient access and quality of care.”
But let’s give the state some credit here. The mission on which it is embarking is very ambitious, and it’s hard to argue with the motivation behind it: to interject some financial reason and provide relief for millions of Californians who forgo needed medical care or nix other important household expenses to afford it.
Sushmita Morris, a 38-year-old Pasadena resident, was shocked by a bill she received for an outpatient procedure last July at the University of Southern California’s Keck Hospital, following a miscarriage. The procedure lasted all of 30 minutes, Morris says, and when she received a bill from the doctor for slightly over $700, she paid it. But then a bill from the hospital arrived, totaling nearly $9,000, and her share was over $4,600.
Morris called the Keck billing office multiple times asking for an itemization of the charges but got nowhere. “I got a robotic answer, ‘You have a high-deductible plan,’” she says. “But I should still receive a bill within reason for what was done.” She has refused to pay that bill and expects to hear soon from a collection agency.
The road to more affordable health care will be long and chock-full of big challenges and unforeseen events that could alter the landscape and require considerable flexibility.
Some flexibility is built in. For one thing, the state cap on spending increases may not apply to health care institutions, industry segments, or geographic regions that can show their circumstances justify higher spending — for example, older, sicker patients or sharp increases in the cost of labor.
For those that exceed the limit without such justification, the first step will be a performance improvement plan. If that doesn’t work, at some point — yet to be determined — the affordability office can levy financial penalties up to the full amount by which an organization exceeds the target. But that is unlikely to happen until at least 2030, given the time lag of data collection, followed by conversations with those who exceed the target, and potential improvement plans.
In California, officials, consumer advocates, and health care experts say engagement among all the players, informed by robust and institution-specific data on cost trends, will yield greater transparency and, ultimately, accountability.
Richard Kronick, a public health professor at the University of California-San Diego and a member of the affordability board, notes there is scant public data about cost trends at specific health care institutions. However, “we will know that in the future,” he says, “and I think that knowing it and having that information in the public will put some pressure on those organizations.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Willpower: A Muscle To Flex, Or Spoons To Conserve?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Willpower: A Muscle To Flex, Or Spoons To Conserve?
We have previously written about motivation; this one’s not about that.
Rather, it’s about willpower itself, and especially, the maintenance of such. Which prompts the question…
Is willpower something that can be built up through practice, or something that is a finite resource that can be expended?
That depends on you—and your experiences.
- Some people believe willpower is a metaphorical “muscle” that must be exercised to be built up
- Some people believe willpower is a matter of metaphorical “spoons” that can be used up
A quick note on spoon theory: this traces its roots to Christine Miserandino’s 2003 essay about chronic illness and the management of limited energy. She details how she explained this to a friend in a practical fashion, she gave her a bunch of spoons from her kitchen, as an arbitrary unit of energy currency. These spoons would then need to be used to “pay” for tasks done; soon her friend realised that if she wanted to make it through the day, she was going to have to give more forethought to how she would “spend” her spoons, or she’d run out and be helpless (and perhaps hungry and far from home) before the day’s end. So, the kind of forethought and planning that a lot of people with chronic illnesses have to give to every day’s activities.
You can read it here: But You Don’t Look Sick? The Spoon Theory
So, why do some people believe one way, and some believe the other? It comes down to our experiences of our own willpower being built or expended. Researchers (Dr. Vanda Siber et al.) studied this, and concluded:
❝The studies support the idea that what people believe about willpower depends, at least in part, on recent experiences with tasks as being energizing or draining.❞
Source: Autonomous Goal Striving Promotes a Nonlimited Theory About Willpower
In other words, there’s a difference between going out running each morning while healthy, and doing so with (for example) lupus.
On a practical level, this translates to practicable advice:
- If something requires willpower but is energizing, this is the muscle kind! Build it.
- If something requires willpower and is draining, this is the spoons kind! Conserve it.
Read the above two bullet-points as many times as necessary to cement them into your hippocampus, because they are the most important message of today’s newsletter.
Do you tend towards the “nonlimited” belief, despite getting tired? If so, here’s why…
There is something that can continue to empower us even when we get physically fatigued, and that’s the extent to which we truly get a choice about what we’re doing. In other words, that “Autonomous” at the front of the title of the previous study, isn’t just word salad.
- If we perceive ourselves as choosing to do what we are doing, with free will and autonomy (i.e., no externally created punitive consequences), we will feel much more empowered, and that goes for our willpower too.
- If we perceive ourselves as doing what we have to (or suffer the consequences), we’ll probably do it, but we’ll find it draining, and that goes for our willpower too.
Until such a time as age-related physical and mental decline truly take us, we as humans tend to gradually accumulate autonomy in our lives. We start as literal babies, then are children with all important decisions made for us, then adolescents building our own identity and ways of doing things, then young adults launching ourselves into the world of adulthood (with mixed results), to a usually more settled middle-age that still has a lot of external stressors and responsibilities, to old age, where we’ve often most things in order, and just ourselves and perhaps our partner to consider.
Consequently…
Age differences in implicit theories about willpower: why older people endorse a nonlimited theory
…which explains why the 30-year-old middle-manager might break down and burn out and stop going to work, while an octogenarian is busy training for a marathon daily before getting back to their daily book-writing session, without fail.
One final thing…
If you need a willpower boost, have a snack*. If you need to willpower boost to avoid snacking, then plan for this in advance by finding a way to keep your blood sugars stable. Because…
The physiology of willpower: linking blood glucose to self-control
*Something that will keep your blood sugars stable, not spike them. Nuts are a great example, unless you’re allergic to such, because they have a nice balance of carbohydrates, protein, and healthy fats.
Want more on that? Read: 10 Ways To Balance Blood Sugars
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: