Staying Alive – by Dr. Jenny Goodman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A lot of “healthy long life” books are science-heavy to the point of being quite challenging to read—they become excellent reference sources, but not exactly “curl up in the armchair” books.
Dr. Goodman writes in a much more reader-friendly fashion, casual yet clear.
She kicks off with season-specific advice. What does that mean? Basically, our bodies need different things at different times of year, and we face different challenges to good health. We may ignore such at our peril!
After a chapter for each of the four seasons (assuming a temperate Northern Hemisphere climate), she goes on to cover the seasons of our life. Once again, our bodies need different things at different times in our life, and we again face different challenges to good health!
There’s plenty of “advice for all seasons”, too. Nutritional dos and don’t, and perennial health hazards to avoid.
As a caveat, she does also hold some unscientific views that may be skipped over. These range from “plant-based diets aren’t sustainable” to “this detox will get rid of heavy metals”. However, the value contained in the rest of the book is more than sufficient to persuade us to overlook those personal quirks.
In particular, she offers very good advice on overcoming cravings (and distinguishing them from genuine nutritional cravings), and taking care of our “trillions of tiny companions” (beneficial gut microbiota) without nurturing Candida and other less helpful gut flora and fauna.
In short, a fine lot of information in a very readable format.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Sugar, Hazelnuts, Books & Brains
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day!
Each Thursday, we respond to subscriber questions and requests! If it’s something small, we’ll answer it directly; if it’s something bigger, we’ll do a main feature in a follow-up day instead!
So, no question/request to big or small; they’ll just get sorted accordingly
Remember, you can always hit reply to any of our emails, or use the handy feedback widget at the bottom. We always look forward to hearing from you!
Q: Interesting info, however, I drink hazelnut milk LOL so would have liked a review of that. But now I want to give hemp and pea milks a try. Thanks
Aww! Here then just for you, is a quick rundown…
- Pros: high in protein¹, vitamin B, and vitamin E
- Cons: high in fat², low in calcium
¹Compared head-to-head with almond milk for example, it has double the protein (but also double the calories)
²However, is also has been found to lower LDL (bad) cholesterol (and incidentally, also reduce inflammation), and in a later systematic review, it was found to not correlate to weight gain, despite its high calorie-content.
If you don’t already, and would like to try making your own…
Click here for step-by-step instructions to make your own hazelnut milk! (very simple)
Q: Wondering if you can evaluate CLA and using it to assist with weight loss. Thanks
Will do! (Watch this space)
Q: What’s the process behind the books you recommend? You seem to have a limitless stream of recommendations
We do our best!
The books we recommend are books that…
- are on Amazon—it makes things tidy, consistent, and accessible. And if you end up buying one of the books, we get a small affiliate commission*.
- we have read—we would say “obviously”, but you might be surprised how many people write about books without having read them.
- pertain in at least large part to health and/or productivity.
- are written by humans—bookish people (and especially Kindle Unlimited users) may have noticed lately that there are a lot of low quality AI-written books flooding the market, sometimes with paid 5-star reviews to bolster them. It’s frustrating, but we can tell the difference and screen those out.
- are of a certain level of quality. They don’t have to be “top 5 desert-island books”, because well, there’s one every day and the days keep coming. But they do have to genuinely deliver the value that we describe, and merit a sincere recommendation.
- are varied—we try to not give a run of “samey” books one after another. We will sometimes review a book that covers a topic another previously-reviewed book did, but it must have something about it that makes it different. It may be a different angle or a different writing style, but it needs something to set it apart.
*this is from Amazon and isn’t product-specific, so this is not affecting our choice of what books to review at all—just that they will be books that are available on Amazon.
Q: Great video on dopamine. Thumbs up on the book recommendation. Would you please consider doing a piece or two on inflammation? I live with Lupus and it is a constant struggle. Thanks for the awesome work you do. Have an excellent day.
Great suggestion! We will do that, and thank you for the kind words!
Q: Why is your newsletter called 10almonds? Maybe I missed it in the intro email, but my curiosity wants to know the significance. Thanks!”
It’s a reference to a viral Facebook hoax! There was a post going around that claimed:
❝HEADACHE REMEDY. Eat 10–12 almonds, the equivalent of two aspirins, next time you have a headache❞ ← not true!
It made us think about how much health-related disinformation there was online… So, calling ourselves 10almonds was a bit of a tongue-in-cheek reference to that story… but also a reminder to ourselves:
We must always publish information with good scientific evidence behind it!
Share This Post
-
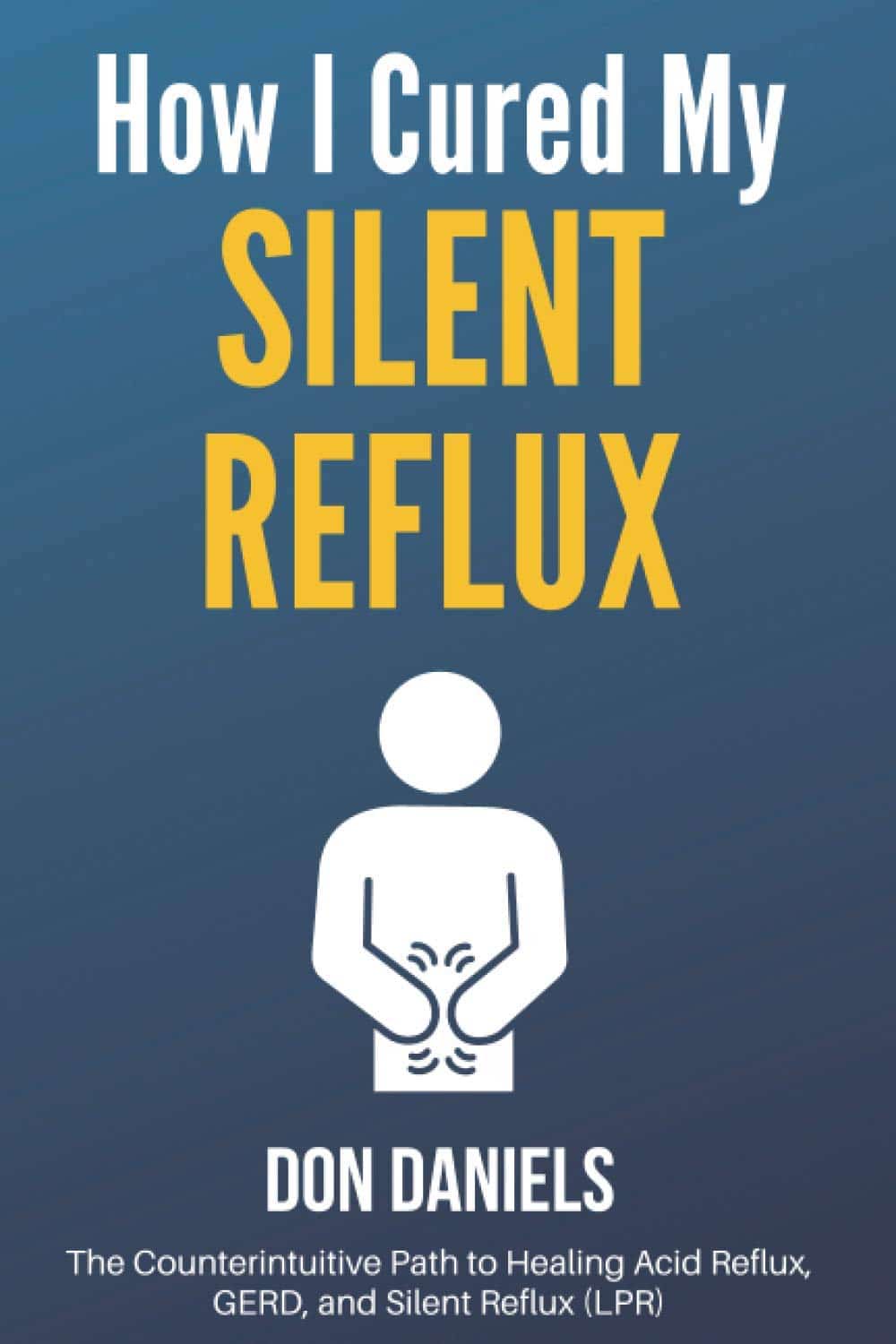
How I Cured My Silent Reflux – by Don Daniels
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Acid reflux, in its various forms (not all of which include heartburn as a symptom!), affects around 1 in 8 people. Often it takes the form of coughing or excess mucus after eating, and it can trigger ostensibly random sweats, for example.
Don Daniels does an excellent job of demystifying the various kinds of acid reflux, explaining clearly and simply the mechanics of what is going on for each of them and why.
Further, he talks about the medications that can make things worse (and how and why), and supplements that can make it better (and supplements that can make it worse, too!), and a multiphase plan (diet on, meds weaned off, supplements on, supplements weaned off when asymptomatic, diet adjust to a new normal) to get free from acid reflux.
The writing style is simple, clear, and jargon-free, while referencing plenty of scientific literature, often quoting from it and providing sources, much like we often do at 10almonds. There are 50+ such references in all, for a 105-page book.
So, do also note that yes, it’s quite a short book for the price, but the content is of value and wouldn’t have benefitted from padding of the kind that many authors do just to make the book longer.
Bottom line: if you have, or suspect you may have, an acid reflux condition of any kind, then this book can guide you through fixing that.
Click here to check out How I Cured My Silent Reflux, and put up with it no longer!
Share This Post
-
Gentler Hair Health Options
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hair, Gently
We have previously talked about the medicinal options for combatting the thinning hair that comes with age especially for men, but also for a lot of women. You can read about those medicinal options here:
Hair-Loss Remedies, By Science
We also did a whole supplement spotlight research review for saw palmetto! You can read about how that might help you keep your hair present and correct, here:
One Man’s Saw Palmetto Is Another Woman’s Serenoa Repens
Today we’re going to talk options that are less “heavy guns”, and/but still very useful.
Supplementation
First, the obvious. Taking vitamins and minerals, especially biotin, can help a lot. This writer takes 10,000µg (that’s micrograms, not milligrams!) biotin gummies, similar to this example product on Amazon (except mine also has other vitamins and minerals in, but the exact product doesn’t seem to be available on Amazon).
When thinking “what vitamins and minerals help hair?”, honestly, it’s most of them. So, focus on the ones that count for the most (usually: biotin and zinc), and then cover your bases for the rest with good diet and additional supplementation if you wish.
Caffeine (topical)
It may feel silly, giving one’s hair a stimulant, but topical caffeine application really does work to stimulate hair growth. And not “just a little help”, either:
❝Specifically, 0.2% topical caffeine-based solutions are typically safe with very minimal adverse effects for long-term treatment of AGA, and they are not inferior to topical 5% minoxidil therapy❞
(AGA = Androgenic Alopecia)
Argan oil
As with coconut oil, argan oil is great on hair. It won’t do a thing to improve hair growth or decrease hair shedding, but it will help you hair stay moisturized and thus reduce breakage—thus, may not be relevant for everyone, but for those of us with hair long enough to brush, it’s important.
Bonus: get an argan oil based hair serum that also contains keratin (the protein used to make hair), as this helps strengthen the hair too.
Here’s an example product on Amazon
Silk pillowcases
Or a silk hair bonnet to sleep in! They both do the same thing, which is prevent damaging the hair in one’s sleep by reducing the friction that it may have when moving/turning against the pillow in one’s sleep.
- Pros of the bonnet: if you have lots of hair and a partner in bed with you, your hair need not be in their face, and you also won’t get it caught under you or them.
- Pros of the pillowcase: you don’t have to wear a bonnet
Both are also used widely by people without hair loss issues, but with easily damaged and/or tangled hair—Black people especially with 3C or tighter curls in particular often benefit from this. Other people whose hair is curly and/or gray also stand to gain a lot.
Here are Amazon example products of a silk pillowcase (it’s expensive, but worth it) and a silk bonnet, respectively
Want to read more?
You might like this article:
From straight to curly, thick to thin: here’s how hormones and chemotherapy can change your hair
Take care!
Share This Post
Related Posts
-
Give Your Adrenal Glands A Chance
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Hats Of Wrath
Your adrenal glands are two little hat-shaped glands that sit on top of your kidneys (like your kidneys are wearing them as hats, in fact).
They produce adrenaline, as you might have guessed, and also cortisol and aldosterone, which you might or might not have known, as well as some miscellaneous corticosteroids that are beyond the scope of today’s article.
Fun fact! For a long time, doctors thought adrenal glands were much larger than they usually are, because of learning anatomy from corpses that were dissected, but invariably the corpses were those of poor people, especially criminals, whose adrenal glands were almost always overworked and swollen.
You don’t want yours to be like that.
What goes wrong
Assuming you don’t have a rare disorder like Addison’s disease (in which the adrenal glands don’t produce enough of the hormones they’re supposed to), your adrenal glands will usually not have trouble producing enough adrenaline et al.
However, as we learned from the Victorian vagabonds, they can also have no problems producing too much—much like any organ that gets overworked, however, this has consequences.
Hopefully you’re not living a life of stressful crime on the streets, but maybe you have other reasons your adrenal glands are working overtime, such as any source of chronic stress, bad sleep (can’t recharge without this downtime), overuse of stimulants (including caffeine and/or nicotine), and, counterintuitively, alcohol. All these things can tax the adrenal glands considerably.
When this happens, in the extreme we can get Cushing’s syndrome, characterized by the symptoms: hypertension, cortisol-based fat distribution i.e. especially face and abdomen, weakness, fragile easily irritable skin, hair loss and/or hirsutism, paradoxically, and of course general fatigue.
In the non-extreme, we get all the same symptoms just to a lower level, and experience what the medical profession is begging us not to call “Adrenal Fatigue Syndrome” because that’s not an official diagnosis, whereas if it gets a name then they’ll be expected to treat it.
What keeps things going right
Obviously, the opposite of the above, for a start. Which means:
Manage chronic stress; see: How To Manage Chronic Stress
Get good sleep; see: Why You Probably Need More Sleep
Go easy on the caffeine; see: Caffeine Mythbusting
Skip the nicotine; see: Nicotine Benefits (That We Don’t Recommend)!
Avoid alcohol; see: How To Reduce Or Quit Alcohol
There are specific vitamins and minerals that support adrenal health too; they are: vitamins B5, B6, B12, C, & D, and also magnesium and zinc.
Good dietary sources of the above include green leafy things, cruciferous vegetables*, nuts and seeds, avocados, olive oil, and if you eat fish, then also fatty fish.
In contrast, it is good to cut down (or avoid entirely) red meat and unfermented dairy.
*Unsure how to get cruciferous vegetables in more often? Try today’s featured recipe, superfood broccoli pesto
Want to know more?
A large part of adrenal health is about keeping cortisol levels down generally (except: for most of us, we can have a little hormesis, as a treat), so for the rest of that you might like to read:
Lower Your Cortisol! (Here’s Why & How)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tips For Avoiding/Managing Rheumatoid Arthritis
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Avoiding/Managing Rheumatoid Arthritis
Arthritis is the umbrella term for a cluster of joint diseases involving inflammation of the joints, hence “arthr-” (joint) “-itis” (suffix used to denote inflammation). These are mostly, but not all, autoimmune diseases, in which the body’s immune system mistakenly attacks our own joints.
Inflammatory vs Non-Inflammatory Arthritis
Arthritis is broadly divided into inflammatory arthritis and non-inflammatory arthritis.
You may be wondering: how does one get non-inflammatory inflammation of the joints?
The answer is, in “non-inflammatory” arthritis, such as osteoarthritis, the damage comes first (by general wear-and-tear) and inflammation generally follows as part of the symptoms, rather than the cause. So the name can be a little confusing. In the case of osteo- and other “non-inflammatory” forms of arthritis, you definitely still want to keep your inflammation at bay as best you can, but it’s not as absolutely critical a deal as it is for “inflammatory” forms of arthritis.
We’ll tackle the beast that is osteoarthritis another day, however.
Today we’re going to focus on…
Rheumatoid Arthritis
This is the most common of the autoimmune forms of arthritis. Some quick facts:
- It affects a little under 1% of the global population, but the older we get, the more likely it becomes
- Early onset of rheumatoid arthritis is most likely to show up around the age of 50 (but it can show up at any age)
- However, incidence (not onset) of rheumatoid arthritis peaks in the 70s age bracket
- It is 2–4 times more common in women than in men
- Approximately one third of people stop work within two years of its onset, and this increases thereafter.
Well, that sounds gloomy.
Indeed it’s not fun. There’s a lot of stiffness and aching of joints (often with swelling too), loss of joint function can be common, and then there are knock-on effects like fatigue, weakness, and loss of appetite.
Beyond that it’s an autoimmune disorder, its cause is not known, and there is no known cure.
Is there any good news?
If you don’t have rheumatoid arthritis at the present time, you can reduce your risk factors in several ways:
- Having an anti-inflammatory diet. Get plenty of fiber, greens, and berries. Fatty fish is great too, as are oily nuts. On the other side of things, high consumption of salt, sugar, alcohol, and red meat are associated with a greater risk of developing rheumatoid arthritis.
- Not smoking. Smoking is bad for pretty much everything, including your chances of developing rheumatoid arthritis.
- Not being obese. This one may be more a matter of correlation than causation, because of the dietary factors (if one eats an anti-inflammatory diet, obesity is less likely), but the association is there.
There are other risk factors that are harder to control, such as genetics, age, sex, and having a mother who smoked.
See: Genetic and environmental risk factors for rheumatoid arthritis
What if I already have rheumatoid arthritis?
If you already have rheumatoid arthritis, it becomes a matter of symptom management.
First, reduce inflammation any (reasonable) way you can. We did a main feature on this before, so we’ll just drop that again here:
Next, consider the available medications. Your doctor may or may not have discussed all of the options with you, so be aware that there are more things available than just pain relief. To talk about them all would require a whole main feature, so instead, here’s a really well-compiled list, along with explanations about each of them, up to date as of this year:
Rheumatoid Arthritis Medication List (And What They Do, And How)
Finally, consider other lifestyle adjustments to manage your symptoms. These include:
- Exercise—gently, though! You do not want to provoke a flare-up, but you do want to maintain your mobility as best you can. There’s a use-it-or-lose-it factor here. Swimming and yoga are great options, as is tai chi. You may want to avoid exercises that involve repetitive impacts to your joints, like running.
- Rest—while keeping mobility going. Get good sleep at night (this is important), but don’t make your bed your new home, or your mobility will quickly deteriorate.
- Hot & cold—both can help, and alternating them can reduce inflammation and stiffness by improving your body’s ability to respond appropriately to these stimuli rather than getting stuck in an inappropriate-response state of inflammation.
- Mobility aids—if it helps, it helps. Maybe you only need something during a flare-up, but when that’s the case, you want to be as gentle on your body as possible while keeping moving, so if crutches, handrails etc help, then by all means get them and use them.
- Go easy on the use of braces, splints, etc—these can offer short-term relief, but at a long term cost of loss of mobility. Only you can decide where to draw the line when it comes to that trade-off.
You can also check out our previous article:
Managing Chronic Pain (Realistically!)
Take good care of yourself!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Carrots vs Parsnips – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing carrots to parsnips, we picked the parsnips.
Why?
There are arguments for both! But we say parsnips win on overall nutritional density.
In terms of macros, parsnips vary quite a lot from region to another, but broadly speaking, parsnips have more carbs and fiber, and/but the ratios are such that carrots have the lower glycemic index. We’ll call this one a win for carrots.
When it comes to vitamins, carrots have more of vitamins A, B2, B3, B6, and choline, while parsnips have more of vitamins B1, B5, B9, C, E, and K. A small win for parsnips here.
In the category of minerals, carrots are not higher in any minerals, while parsnips are higher in calcium, copper, iron, magnesium, manganese, phosphorus, potassium, selenium, and zinc. An overwhelming win for parsnips.
While the overall vitamin and mineral content puts parsnips ahead, it’s still worth noting that carrots have highly bioavailable megadoses of vitamin A.
Another thing to note is that the glycemic index recorded for both is when peeled and boiled, whereas both of these root vegetables can be enjoyed raw if you wish, which has a much lower GI.
In short, enjoy either or both, but parsnips are the more nutritionally dense overall.
Want to learn more?
You might like to read:
Glycemic Index vs Glycemic Load vs Insulin Index
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: