Early Bird Or Night Owl? Genes vs Environment
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A Sliding Slope?
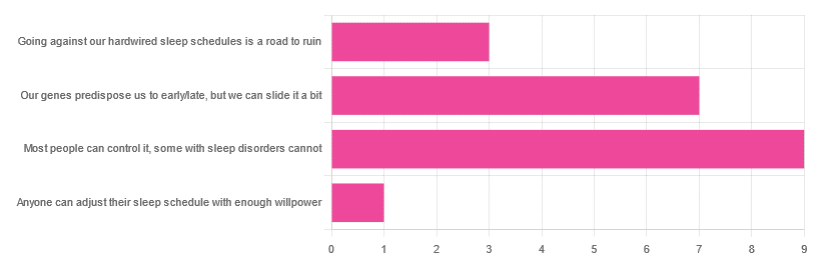
In Tuesday’s newsletter, we asked you how much control you believe we have over our sleep schedule, and got the above-depicted, below-described, set of responses:
- 45% said “most people can control it; some people with sleep disorders cannot
- 35% said “our genes predispose us to early/late, but we can slide it a bit
- 15% said: “going against our hardwired sleep schedules is a road to ruin”
- 5% said “anyone can adjust their sleep schedule with enough willpower”
You may be wondering: what’s with those single-digit numbers in the graph there? And the answer is: Tuesday’s email didn’t go out at the usual time due to a scheduling mistake (sorry!), which is probably what affected the number of responses (poll response levels vary, but are usually a lot higher than this).
Note: yes, this does mean most people who read our newsletter don’t vote. So, not to sound like a politician on the campaign trail, but… Your vote counts! We always love reading your comments when you add those, too—often they provide context that allow us to tailor what we focus on in our articles
However, those are the responses we got, so here we are!
What does the science say?
Anyone can adjust their sleep with enough willpower: True or False?
False, simply. It’s difficult for most people, but for many people with sleep disorders, it is outright impossible.
In a battle of narcolepsy vs willpower, for example, no amount of willpower will stop the brain from switching to sleep mode when it thinks it’s time to sleep:
❝Narcolepsy is the most common neurological cause of chronic sleepiness. The discovery about 20 years ago that narcolepsy is caused by selective loss of the neurons producing orexins sparked great advances in the field
[There is also] developing evidence that narcolepsy is an autoimmune disorder that may be caused by a T cell-mediated attack on the orexin neurons and explain how these new perspectives can inform better therapeutic approaches.❞
~ Dr. Carrie Mahoney et al. (lightly edited for brevity)
Source: The neurobiological basis of narcolepsy
For further reading, especially if this applies to you or a loved one:
Our genes predispose us to early/late, but we can slide it a bit: True or False?
True! First, about our genes predisposing us:
…and also:
Gene distinguishes early birds from night owls and helps predict time of death
Now, as for the “can slide it a bit”, this is really just a function of the general categories of “early bird” and “night owl” spanning periods of time that allow for a few hours’ wiggle-room at either side.
However, it is recommended to make any actual changes more gradually, with the Sleep Foundation going so far as to recommend 30 minutes, or even just 15 minutes, of change per day:
Sleep Foundation | How to Fix Your Sleep Schedule
Going against our hardwired sleep schedule is a road to ruin: True or False?
False, contextually. By this we mean: our “hardwired” sleep schedule is (for most of us), genetically predisposed but not predetermined.
Also, genetic predispositions are not necessarily always good for us; one would not argue, for example, for avoiding going against a genetic predisposition to addiction.
Some genetic predispositions are just plain bad for us, and genes can be a bit of a lottery.
That said, we do recommend getting some insider knowledge (literally), by getting personal genomics tests done, if that’s a viable option for you, so you know what’s really a genetic trait (and what to do with that information) and what’s probably caused by something else (and what to do with that information):
Genetic Testing: Health Benefits & Methods
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
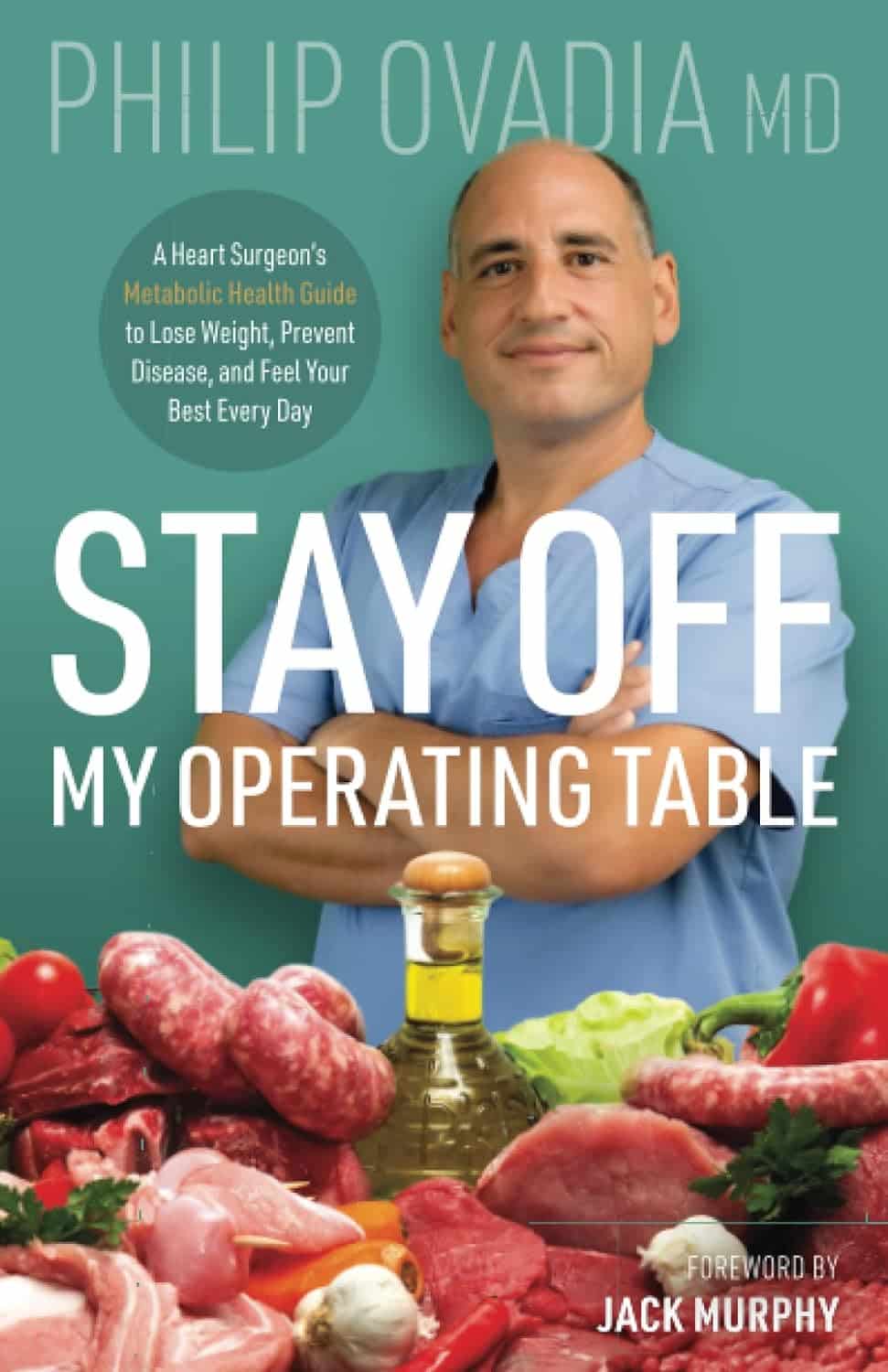
Stay off My Operating Table – by Dr. Philip Ovadia
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
With heart disease as the #1 killer worldwide, and 88% of adults being metabolically unhealthy (leading cause of heart disease), this is serious!
Rather than taking a “quick fix” advise-and-go approach, Dr. Ovadia puts the knowledge and tools in our hands to do better in the long term.
As a heart surgeon himself, his motto here is:
❝What foods to put on your table so you don’t end up on mine❞
There’s a lot more to this book than the simple “eat the Mediterranean diet”:
- While the Mediterranean diet is generally considered the top choice for heart health, he also advises on how to eat healthily on all manner of diets… Carnivore, Keto, Paleo, Atkins, Gluten-Free, Vegan, you-name-it.
- A lot of the book is given to clearing up common misconceptions, things that sounded plausible but are just plain dangerous. This information alone is worth the price of the book, we think.
- There’s also a section given over to explaining the markers of metabolic health, so you can monitor yourself effectively
- Rather than one-size-fits-all, he also talks about common health conditions and medications that may change what you need to be doing
- He also offers advice about navigating the health system to get what you need—including dealing with unhelpful doctors!
Bottom line: A very comprehensive (yet readable!) manual of heart health.
Get your copy of Stay Off My Operating Table from Amazon today!
Share This Post
-
How To Make Your Doctor’s Appointment Do More For You
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Doctor: “So, how are you today?”
Patient: “Can’t complain; how about you?”Hopefully your medical appointments don’t start quite like that, but there can be an element of being “along for the ride” when it comes to consultations. They ask questions, we answer, they prescribe something, we thank them.
In principle, the doctor should be able to handle that; ask the right questions, determine the problem, and not need too much from you. After all, they have been trained to deal with an unconscious patient, so the fact you can communicate at all is a bonus.
However, leaving it all to them isn’t really playing the field.
Before the appointment
Research your issue, as best you understand it. Some doctors will be very averse to you telling them about having done this (taking it as an affront to their expertise), but here’s the thing:
You don’t have to tell them.
You just have to understand as much as possible, so that you will be as “up to speed” as possible in the conversation, and not be quickly out of your depth.
Have an agenda, based on the above. Literally, have a little set of bullet-points to remind you what you came in to discuss, so that nothing escapes you in the moment. This should also include:
- If you have additional reasons for a particular concern (e.g. family history of a certain problem), make them known
- If you plan to request any specific tests or treatments, be able to clearly state your reasons for the specific tests or treatments
- If you plan to write off any specific tests or treatments as something to which you will not consent, have your reasons ready—in a way that makes it clear it’s something more than “don’t want it”, for example, “I’ve already decided that this treatment would make a sufficient hit to my quality of life, as to make it not worthwhile for me personally” (or whatever the reason may be for you). It needs to be something they can write on their notes instead of simply “patient refused treatment”.
Compile a record of your symptoms (as appropriate), and any previous tests/treatments (as appropriate), in chronological order. If you take all this with you, perhaps in a nice folder, you will enjoy the following advantages:
- not forgetting anything
- ability to answer questions accurately
- give the (correct) impression you take your health seriously, which means they are more likely to do so also—especially because they will now know that if they fob you off and/or mess something up, you’ll be taking a record of that to your next appointment.
Plan your outfit. No, you don’t have to dress for the red carpet, but you want to satisfy two main conditions:
- Accessibility for examination (for example, if you are going in with a knee pain, maybe don’t wear the tight jeans today; if they’re going to take blood, be either sleeveless or have sleeves that are easily moved out of the way, etc)
- General presentability (it’s a sad fact that doctors are not immune to biases, and will treat people better if they respect them more)
During the appointment
Be friendly; doctors (like most people) will respond much better to that than to grumpiness—even if you have good reason for grumpiness and even if the doctor has been trained to help grumpy patients.
Be confident: when we say “be friendly”, that doesn’t mean to necessarily be so agreeable as to not advocate for yourself. In particular:
- If they explain something and it isn’t clear to you, ask them to clarify
- If you disagree with them about a value judgement, say so. By “a value judgement” here we mean things in the realm of subjectivity. If the doctor says you are prediabetic, then you won’t get much mileage out of arguing otherwise; the numbers have the final say on that one. But if the doctor says “the side effects of the treatment you’re requesting will make it not worthwhile for you” and you have understood the side effects and you still disagree, then your opinion counts for more than theirs—it is your decision to make.
- If they dismiss a concern, ask them to put in writing that they dismissed your concern of X, despite you providing evidence that Y, and it being well-known that Z. Often, rather than doing that, they’ll just fold and actually address your concern instead.
Writer’s example in that last category: I recently made a request for a bone density scan. I expect my bone density is great, because I do all the right things, however, as both of my parents suffered from osteoporosis and assorted resultant crushed bones and the terrible consequences thereof, I a) have reasonable grounds for extra concern, and b) I believe that even if my bone density is fine now, it’s good to establish a baseline so I can know, in 5, 10, 20 years etc, whether there has been any deterioration. Now, happily the doctor I saw agreed with my assessment at first presentation and so I got the referral, but had she not been, I would have said “Could you please put in writing that I asked for a bone density scan, and you refused, on the grounds that [details about what happened with my parents], and that osteoporosis is known to have a strong genetic component is not, in your opinion, any reason to worry?”
Be honest, and/but err on the side of overstating your symptoms rather than understating. For example, if it is about a chronic condition and the doctor asks “are you able to do xyz”, take the question as meaning “are you able to do xyz on your worst days?”. You can clarify that if you like in your answer, but you need to include the information that xyz is something that your condition can and sometimes does impede you from doing.
Leave your embarrassment at the door. To the doctor (unless they are a very unprofessional one), you really are just one more patient with symptoms they have (unless your condition is very rare) seen a thousand times before. If your symptom is embarrassing, it will not faze them and you definitely should not hold back from mentioning it, for example. This goes extra in the case of discussions around sexual health, by the way, in which field the details you’d perhaps rather not share with anybody, are the details they need to adequately treat you.
After the appointment
Follow up on anything that doesn’t happen as promised (e.g. referrals, things ordered, etc), to make sure nothing got lost in a bureacratic error.
Get a second opinion if you’re not satisfied with the first one. Doctors are fallible, and as a matter of professional pride, it’s likely the second doctor will be glad to find something the first doctor missed.
See also: Make Your Negativity Work For You
Take care!
Share This Post
-
Soap vs Sanitizer – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing soap to sanitizer, we picked the soap.
Why?
Both are good at killing bacteria / inactivating viruses, but there are several things that set them apart:
- Soap doesn’t just kill them; it slides them off and away down the drain. That means that any it failed to kill are also off and down the drain, not still on your hands. This is assuming good handwashing technique, of course!
- Sanitizer gel kills them, but can take up to 4 minutes of contact to do so. Given that people find 20 seconds of handwashing laborious, 240 seconds of sanitizer gel use seems too much to hope for.
Both can be dehydrating for the hands; both can have ingredients added to try to mitigate that.
We recommend a good (separate) moisturizer in either case, but the point is, the dehydration factor doesn’t swing it far either way.
So, we’ll go with the one that gets rid of the germs the most quickly: the soap
10almonds tip: splash out on the extra-nice hand-soaps for your home—this will make you and others more likely to wash your hands more often! Sometimes, making something a more pleasant experience makes all the difference.
Want to know more?
Check out:
Take care!
Share This Post
Related Posts
-
The Cough Doctor
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Cough Doctor
This is Dr. Peter Small, who worked in epidemiology since the beginning of HIV epidemic. He became a pioneer in the field of molecular epidemiology. As such, his work was a guiding beacon for the public health response to the resurgence of tuberculosis. He’s travelled the world spending years in various institutions studying all manner of respiratory illnesses…. These have ranged from tuberculosis to pneumonia to lung cancer and (back to epidemiology) Covid-19.
He’s now the Chief Medical Officer at…
Hyfe
Hyfe, a medical AI company, was founded in 2020. Its objective: to build acoustic tools for respiratory diagnostics and monitoring.
In other words: it records coughs and collects data about coughing.
❝It’s ironic how much people focus on counting steps while ignoring cough, which is far more consequential. Hyfe is a science-driven company with the technology to make cough count. Particularly now, with increased awareness of cough and the rapid growth of digital health driven by Covid-19, this technology can improve the lives of patients, the care provided by doctors, and the efficiency of health systems.❞
~ Dr. Peter Small, CMO, Hyfe
How does it do it?
Hyfe’s AI monitors the number of times a person coughs and the sound of the cough through any smartphone or other smart device.
This data collected over time provides increasingly more reliable information than a single visit to the doctor! By constantly listening and analyzing, it can detect patterns that might otherwise go unnoticed.
How big is this “big data” effort?
Hyfe maintains the largest cough dataset in the world. This means it can compare the sound of a patient’s cough with more than 400 million cough-like sounds from 83 countries across all continents.
The human brain doesn’t handle big numbers well. So, just to illustrate: if the average cough is 1 second long, that means it’d take more than 12 years to listen to them all.
Hyfe, meanwhile, can:
- listen to many things simultaneously
- index them all against user and location,
- use its ever-growing neural net to detect and illustrate patterns.
It’s so attentive, that it can learn to distinguish between different people’s coughs in the same household.
❝Companies like Google Health see even basic information such as getting an accurate count of the number of times a person coughs a day as a useful resource, and part of a larger need to collect and chronicle more health information to refine the way doctors diagnose disease and manage treatments in the future.❞
What are the public health implications?
The most obvious application is to note when there’s a spike in coughing, and see how such spikes grow and spread (if they do), to inform of contagion risks.
Another is to cross-reference it with data about local environmental allergens. Knowing how things like pollution and even pollen affect individuals differently could be helpful in identifying (and managing) chronic conditions like asthma.
What are the private health implications?
❝It’s going to transform the whole clinical approach for this common and chronic symptom. Patients will come in, have the data on how much they are coughing, and the physician can suggest a treatment based on that information to see if it makes the coughs better❞
~ Dr. Peter Small
Dr. Small’s colleague Dr. Cai, speaking for Google Health on this project, sees even more utility for diagnostics:
❝When I was in medical school, never ever did they teach us that we could listen to somebody cough and identify whether that person has TB (tuberculosis), COPD, or a tumor. But I keep seeing more and more studies of people coughing into a microphone, and an algorithm can detect whether somebody has TB with 95% specificity and sensitivity, or if someone has pneumonia or an exacerbation of COPD❞
~ Dr. Lawrence Cai
And the privacy implications?
Perhaps you don’t quite fancy the idea of not being able to cough without Google knowing about it. Hyfe’s software is currently opt-in, but…
If you cough near someone else’s Hyfe app, their app will recognize you’re not the app’s user, and start building a profile for you. Of course, that won’t be linked to your name, email address, or other IDs, as it would if you were the app’s user.
Hyfe will ask to connect to your social media, to collect more information about you and your friends.
Whether you’d like to try this or perhaps you’re just curious to learn more about this fascinating project, you can check out:
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hazelnuts vs Chestnuts – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing hazelnuts to chestnuts, we picked the hazelnuts.
Why?
This one’s not close.
In terms of macros, we have some big difference to start with, since chestnuts contain a lot more water and carbs whereas hazelnuts contain a lot more protein, fats, and fiber. The fats, as with most nuts, are healthy; in this case mostly being monounsaturated fat.
Because of the carbs and fiber being so polarized (i.e., chestnuts have most of the carbs and hazelnuts have most of the fiber), there’s a big difference in glycemic index; hazelnuts have a GI of 15 while chestnuts have a GI of 52.
In the category of vitamins, hazelnuts contain more of vitamins A, B1, B2, B3, B5, B6, and B9, while chestnuts contain more vitamin C.
When it comes to minerals, the story is similar: hazelnuts contain a lot more calcium, copper, iron, magnesium, manganese, phosphorus, and zinc, while chestnuts contain a tiny bit more potassium.
All in all, enjoy either or both, but nutritionally speaking, hazelnuts are a lot better in almost every way.
Want to learn more?
You might like to read:
Why You Should Diversify Your Nuts
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Oh, Honey
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The Bee’s Knees?
If you’d like to pre-empt that runny nose, some say that local honey is the answer. The rationale is that bees visiting the local sources of pollen and making honey will introduce the same allergens to you in a non allergy-inducing fashion (the honey). The result? Inoculation against the allergens in question.
But does it work?
Researching this, we found a lot of articles saying there was no science to back it up.
And then! We found one solitary study from 2013, and the title was promising:
But we don’t stop at titles; that’s not the kind of newsletter we are. We pride ourselves on giving good information!
And it turned out, upon reading the method and the results, that:
- Both the control and test groups also took loratadine for the first 4 weeks of the study
- The test group additionally took 1g/kg bodyweight of honey, daily—so for example if you’re 165lb (75kg), that’s about 4 tablespoons per day
- The control group took the equivalent amount of honey-flavored syrup
- Both groups showed equal improvements by week 4
- The test group only showed continued improvements (over the control group) by week 8
The researchers concluded from this:
❝Honey ingestion at a high dose improves the overall and individual symptoms of AR, and it could serve as a complementary therapy for AR.❞
We at 10almonds concluded from this:
❝That’s a lot of honey to eat every day for months!❞
We couldn’t base an article on one study from a decade ago, though! Fortunately, we found a veritable honeypot of more recent research, in the form of this systematic review:
Read: The Potential Use Of Honey As A Remedy For Allergic Diseases
…which examines 13 key studies and 43 scientific papers over the course of 21 years. That’s more like it! This was the jumping-off point we needed into more useful knowledge.
We’re not going to cite all those here—we’re a health and productivity newsletter, not an academic journal of pharmacology, but we did sift through them so that you don’t have to, and:
The researchers (of that review) concluded:
❝Although there is limited evidence, some studies showed remarkable improvements against certain types of allergic illnesses and support that honey is an effective anti-allergic agent.❞
Our (10almonds team) further observations included:
- The research review notes that a lot of studies did not confirm which phytochemical compounds specifically are responsible for causing allergic reactions and/or alleviating such (so: didn’t always control for what we’d like to know, i.e. the mechanism of action)
- Some studies showed results radically different from the rest. The reviewers put this down to differences that were not controlled-for between studies, for example:
- Some studies used very different methods to others. There may be an important difference between a human eating a tablespoon of honey, and a rat having aerosolized honey shot up its nose, for instance. We put more weight to human studies than rat studies!
- Some kinds of honey (such as manuka) contain higher quantities of gallic acid which itself can relieve allergies by chemically inhibiting the release of histamine. In other words, never mind pollen-based inoculations… it’s literally an antihistamine.
- Certain honeys (such as tualang, manuka and gelam) contain higher quantities of quercetin. What’s quercetin? It’s a plant flavonoid that a recent study has shown significantly relieves symptoms of seasonal allergies. So again, it works, just not for the reason people say!
In summary:
The “inoculation by local honey” thing specifically may indeed remain “based on traditional use only” for now.
But! Honey as a remedy for allergies, especially manuka honey, has a growing body of scientific evidence behind it.
Bottom line:
If you like honey, go for it (manuka seems best)! It may well relieve your symptoms.
If you don’t, off-the-shelf antihistamines remain a perfectly respectable option.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: