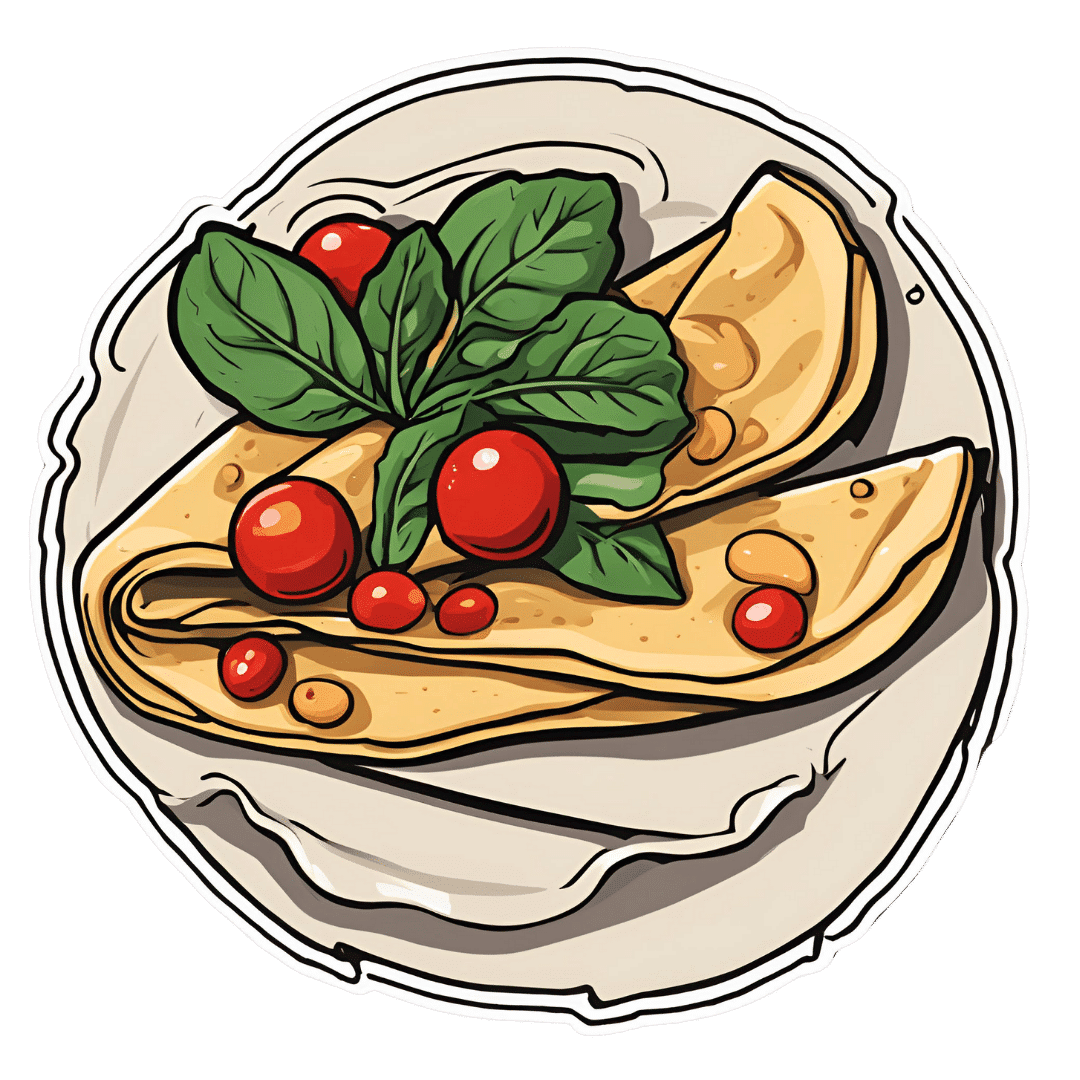
Savory Protein Crêpe
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pancakes have a bad reputation healthwise, but they don’t have to be so. Here’s a very healthy crêpe recipe, with around 20g of protein per serving (which is about how much protein most people’s body’s can use at one sitting) and a healthy dose of fiber too:
You will need
Per crêpe:
- ½ cup milk (your preference what kind; we recommend oat milk for this)
- 2 oz chickpea flour (also called garbanzo bean flour, or gram flour)
- 1 tsp nutritional yeast
- 1 tsp ras el-hanout (optional but tasty and contains an array of beneficial phytochemicals)
- 1 tsp dried mixed herbs
- ⅛ tsp MSG or ¼ tsp low-sodium salt
For the filling (also per crêpe):
- 6 cherry tomatoes, halved
- Small handful baby spinach
- Extra virgin olive oil
Method
(we suggest you read everything at least once before doing anything)
1) Mix the dry crêpe ingredients in a bowl, and then stir in the milk, whisking to mix thoroughly. Leave to stand for at least 5 minutes.
2) Meanwhile, heat a little olive oil in a skillet, add the tomatoes and fry for 1 minute, before adding the spinach, stirring, and turning off the heat. As soon as the spinach begins to wilt, set it aside.
3) Heat a little olive oil either in the same skillet (having been carefully wiped clean) or a crêpe pan if you have one, and pour in a little of the batter you made, tipping the pan so that it coats the pan evenly and thinly. Once the top is set, jiggle the pan to see that it’s not stuck, and then flip your crêpe to finish on the other side.
If you’re not confident of your pancake-tossing skills, or your pan isn’t good enough quality to permit this, you can slide it out onto a heatproof chopping board, and use that to carefully turn it back into the pan to finish the other side.
4) Add the filling to one half of the crêpe, and fold it over, pushing down at the edges with a spatula to make a seal, cooking for another 30 seconds or so. Alternatively, you can just serve a stack of crêpes and add the filling at the table, folding or rolling per personal preference:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Three Daily Servings of Beans?
- Lycopene’s Benefits For The Gut, Heart, Brain, & More
- Our Top 5 Spices: How Much Is Enough For Benefits?
- Sea Salt vs MSG – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Miracle of Flexibility – by Miranda Esmonde-White
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve reviewed books about stretching before, so what makes this one different?
Mostly, it’s that this one takes a holistic approach, making the argument for looking after all parts of flexibility (even parts that might seem useless) because if one bit of us isn’t flexible, the others will start to suffer in compensation because of how that affects our posture, or movement, or in many cases our lack of movement.
Esmonde-White’s “flexibility, from your toes to your shoulders” approach is very consistent with her background as a professional ballet dancer, and now she brings it into her profession as a coach.
The book’s not just about stretching, though. It looks at problems and what can go wrong with posture and the body’s “musculoskeletal trifecta”, and also shares daily training routines that are tailored for specific sporting interests, and/or for those with specific chronic conditions and/or chronic pain. Working around what needs to be worked around, but also looking at strengthening what can be strengthened and fixing what can be fixed along the way.
Bottom line: if your flexibility needs an overhaul, this book is a very good “one-stop shop” for that.
Click here to check out The Miracle Of Flexibility, and discover what you can do!
Share This Post
-
Makkō-Hō – by Haruka Nagai
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve all heard the claims, “Fluent in 3 Months!”, “Russian in Two Weeks!”, “Overnight Mandarin Chinese”, “15-Minute Arabic!”, “Instant Italian!”.
We see the same in the world of health and fitness too. So how does this one’s claim of “five minutes’ physical fitness” hold up?
Well, it is 5 minutes per day. And indeed, the author writes:
❝The total time [to do these exercises], then, is only one minute and thirty seconds. This series I call one round. When it has been completed, execute another complete round. You should find the exercises easier to do the second time. Executed this way, the exercsies will prove very effective, though they take only three minutes in all. After you have leaned back into the final position, you must remain in that posture for one minute. That brings the total time to four minutes. Even when [some small additions] are added, it takes only five minutes at most.❞
The exercises themselves are from makkō-hō, which is a kind of Japanese dynamic yoga. They involve repetitions of (mostly) moving stretches with good form, and are excellent for mobility and general health, keeping us supple and robust as we get older.
The text descriptions are clear, as are the diagrams and photos. The language is a little dated, as this book was written in the 1970s, but the techniques themselves are timeless.
Bottom line: consider it a 5-minute anti-aging regimen. And, as Nagai says, “the person who cannot find 5 minutes out of 24 hours, was never truly interested in their health”.
Click here to check out Makkō-Hō and schedule your five minutes!
Share This Post
-
Tasty Hot-Or-Cold Soup
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Full of fiber as well as vitamins and minerals, this versatile “serve it hot or cold” soup is great whatever the weather—give it a try!
You will need
- 1 quart low-sodium vegetable stock—ideally you made this yourself from vegetable offcuts you kept in the freezer until you had enough to boil in a big pan, but failing that, a large supermarket will generally be able to sell you low-sodium stock cubes.
- 2 medium potatoes, peeled and diced
- 2 leeks, chopped
- 2 stalks celery, chopped
- 1 large onion, diced
- 1 large carrot, diced, or equivalent small carrots, sliced
- 1 zucchini, diced
- 1 red bell pepper, diced
- 1 tsp rosemary
- 1 tsp thyme
- ¼ bulb garlic, minced
- 1 small piece (equivalent of a teaspoon) ginger, minced
- 1 tsp red chili flakes
- 1 tsp black pepper, coarse ground
- ½ tsp turmeric
- Extra virgin olive oil, for frying
- Optional: ½ tsp MSG or 1 tsp low-sodium salt
About the MSG/salt: there should be enough sodium already from the stock and potatoes, but in case there’s not (since not all stock and potatoes are made equal), you might want to keep this on standby.
Method
(we suggest you read everything at least once before doing anything)
1) Heat some oil in a sauté pan, and add the diced onion, frying until it begins to soften.
2) Add the ginger, potato, carrot, and leek, and stir for about 5 minutes. The hard vegetables won’t be fully cooked yet; that’s fine.
3) Add the zucchini, red pepper, celery, and garlic, and stir for another 2–3 minutes.
4) Add the remaining ingredients; seasonings first, then vegetable stock, and let it simmer for about 15 minutes.
5) Check the potatoes are fully softened, and if they are, it’s ready to serve if you want it hot. Alternatively, let it cool, chill it in the fridge, and enjoy it cold:
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Eat More (Of This) For Lower Blood Pressure
- Our Top 5 Spices: How Much Is Enough For Benefits? ← 5/5 in our recipe today!
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk?
Take care!
Share This Post
Related Posts
-
Carbonated Water: For Weight Loss, Satiety, Or Just Gas?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are two main mechanisms of action by which sparkling water is considered to help satiety and/or weight loss; they are:
- It “fills us up” such that we feel fuller sooner, and thus eat less, and thus (all other things being equal) perhaps lose weight
- The carbon dioxide is absorbed into the bloodstream, where (as a matter of chemistry) it improves glucose metabolism, thus lowering blood sugars and indirectly leading (potentially) to weight loss, but even if not, lowered blood sugars are good for most people most of the time, right?
However, there are just a few problems:
Full of gas?
Many people self-report enjoying sparkling water as a way to feel fuller while fasting (or even while eating). However, the plural of “anecdote” is not “data”, so, here be data… Ish:
❝In order to determine whether such satiating effects occur through oral carbonic stimulation alone, we conducted modified sham-feeding (SF) tests (carbonated water ingestion (CW), water ingestion (W), carbonated water sham-feeding (CW-SF), and water sham-feeding (W-SF)), employing an equivalent volume and standardized temperature of carbonated and plain water, in a randomized crossover design.
Thirteen young women began fasting at 10 p.m. on the previous night and were loaded with each sample (15ºC, 250 mL) at 9 a.m. on separate days. Electrogastrography (EGG) recordings were obtained from 20 min before to 45 min after the loading to determine the power and frequency of the gastric myoelectrical activity. Appetite was assessed using visual analog scales. After ingestion, significantly increased fullness and decreased hunger ratings were observed in the CW group. After the load, transiently but significantly increased fullness as well as decreased hunger ratings were observed in the CW-SF group. The powers of normogastria (2-4 cpm) and tachygastria (4-9 cpm) showed significant increases in the CW and W groups, but not in the CW-SF and W-SF groups. The peak frequency of normogastria tended to shift toward a higher band in the CW group, whereas it shifted toward a lower band in the CW-SF group, indicating a different EGG rhythm.
Our results suggest that CO2-induced oral stimulation is solely responsible for the feeling of satiety.❞
~ Dr. Maki Suzuki et al.
Now, that’s self-reported, and a sample size of 13, so it’s not the most airtight science ever, but it is at least science. Here’s the paper, by the way:
Oral Carbonation Attenuates Feeling of Hunger and Gastric Myoelectrical Activity in Young Women
Here’s another small study with 8 people, which found that still and sparkling water had the exact same effect:
Effect of carbonated water on gastric emptying and intragastric meal distribution
However, drinking water (still or sparkling) with a meal will not have anywhere near the same effect for satiety as consuming food that has a high water-content.
See also: Some Surprising Truths About Hunger And Satiety ← our main feature in which we examine the science of volumetrics, including a study that shows how water incorporated into a food (but not served with a food) decreases caloric intake.
As an aside, one difference that carbonation can make is to increase ghrelin levels—that’s the hunger hormone (the satiety hormone is leptin, by the way). This one’s a rat study, but it seems reasonable that the same will be true of humans:
…which is worth bearing in mind even if you yourself are not, in fact, a male rat.
The glucose guzzler?
This one has simply been the case of a study being misrepresented, for example here:
Fizzy water might aid weight loss by providing a small boost to glucose uptake and metabolism
The idea is that higher levels of carbon dioxide in the blood mean faster glucose metabolism, which is technically true. Now, often “technically true” is the best kind of true, but not here, because it’s simply not useful.
In short, we produce so much carbon dioxide as part of our normal respiratory processes, that any carbon dioxide we might consume in a carbonated water is barely a blip in the graph.
Oh, and that article we just linked? Even within the article, despite running with that headline, the actual scientists quoted are saying such things as:
❝While there is a hypothetical link between carbonated water and glucose metabolism, this has yet to be tested in well-designed human intervention studies❞
~ Professor Sumantra Ray
Note: the word “hypothetical” means “one level lower than theoretical”. This is very far from being a conclusion.
And the study itself? Wasn’t even about carbonated water, it was about kidney dialysis and how the carbon dioxide content can result in hypoglycemia:
The mechanism of hypoglycemia caused by hemodialysis
…which got referenced in this paper (not a study):
Can carbonated water support weight loss?
…and even that concluded:
❝CO2 in carbonated water may promote weight loss by enhancing glucose uptake and metabolism in red blood cells.
However, the amount is so small that it is difficult to expect weight loss effects solely from the CO2 in carbonated water.
Drinking carbonated water may also affect blood glucose measurements.❞
Note: the word “may”, when used by a scientist and in the absence of any stronger claims, means “we haven’t ruled out the possibility”.
What breaking news that is.
Stop the press! No, really, stop it!
So… What does work?
There are various ways of going about actually hacking hunger (and they stack; i.e. you can use multiple methods and get cumulative results), and we wrote about them here:
Enjoy!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Death by Food Pyramid – by Denise Minger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one is less about “here’s the perfect way of eating” or even “these specific foods are ontologically evil”, but more about teaching science literacy.
The author explores various health trends from the 70s until time of writing (the book was published in 2014), what rationales originally prompted them, and what social phenomena either helped them to persist, or caused them to get dropped quite quickly.
Of course, even in the case of fads that are societally dropped quite quickly, on an individual level there will always be someone just learning about it for the first time, reading some older material, and thinking “that sounds like just the miracle life-changer I need!”
What she teaches the reader to do is largely what we do a lot of here at 10almonds—examine the claims, go to the actual source material (studies! Not just books about studies!), and see whether the study conclusions actually support the claim, to start with, and then further examine to see if there’s some way (or sometimes, a plurality of ways) in which the study itself is methodologically flawed.
Which does happen sometimes, do actually watch out for that!
The style is quite personal and entertaining for the most part, and yet even moving sometimes (the title is not hyperbole; deaths will be discussed). As one might expect of a book teaching science literacy, it’s very easy to read, with copious footnotes (well, actually they are at the back of the book doubling up as a bibliography, but they are linked-to throughout) for those who wish to delve deeper—something the author, of course, encourages.
Bottom line: if you’d like to be able to sort the real science from the hype yourself, then this book can set you on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
More Things Dopamine Does For Us
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In this week’s news roundup, we have two dopamine items and one other for variety:
The real “dopamine switch”
Dopamine is well-known as “the reward chemical”, and indeed it is that, but it also plays a central role in many neurological processes, including:
- Linear task processing
- Motivation
- Learning and memory
- Motor functions
- Language faculties
Recent research has now shown its importance in cognitive flexibility, i.e. the ability to adapt to circumstances, and switch approaches appropriately to such, and generally not get stuck in a cognitive rut:
Read in full: Scientists confirm neurobiochemical link between dopamine and cognitive flexibility
Related: The Dopamine Myth
You may like the sound of this
It’s been known for a while that dopamine is involved in learning and memory (as mentioned above), but this has been established largely by associative studies, e.g. “people with lower dopamine levels learn less easily”. But scientists have now mapped out more of how it actually does that.
One more reason to ensure we have and maintain healthy dopamine levels!
Read in full: Songbirds highlight dopamine’s role in learning
Related: 10 Ways To Naturally Boost Dopamine
Resist Or Run!
When it comes to protecting against bone loss, resistance exercise remains key, but impact-laden activities such as running (but not lower-level everyday activity) can help too. There have been studies on the extent to which walking (a load-bearing activity) may be protective against bone loss, and the results of those studies have mostly been inconclusive.
This study looked into the incidence (or not, as the case may be) of bone-loading impacts in everyday movements, using accelerometers, and measured bone mineral density before and after testing periods. Those that had higher-intensity bone-loading movements (so, resistance training or running, for example) retained the best measures of bone density through menopause into postmenopause:
Read in full: Everyday physical activity does not slow bone loss during menopause, finds study
Related: The Bare-Bones Truth About Osteoporosis
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: