Move over, COVID and Flu! We Have “Hybrid Viruses” To Contend With Now
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Move over, COVID and Flu! We have “hybrid viruses” to contend with now
COVID and influenza viruses can be serious, of course, so let’s be clear up front that we’re not being dismissive of those. But, most people are hearing a lot about them, whereas respiratory syncytial virus (RSV) has flown under a lot of radars.
Simply put, until recently it hasn’t been considered much of a threat except to the young, the old, or people with other respiratory illnesses. Only these days, the prevalence of “other respiratory illnesses” is a lot higher than it used to be!
It’s not just a comorbidity
It’s easy to think “well of course if you have more than one illness at once, especially similar ones, that’s going to suck” but it’s a bit more than that; it produces newer, more interesting, hybrid viruses. Here’s a research paper from last year’s “flu season”:
Coinfection by influenza A virus and respiratory syncytial virus produces hybrid virus particles
Best to be aware of this if you’re in the “older” age-range
It’s not just that the older we are, the more likely we are to get it. Critically, the older we are, the more likely we are to be hospitalized by it.
And..the older we are, the less likely we are to come back from hospital if hospitalized by it.
Some years back, the intensive care and mortality rates for people over the age of 65 were 8% and 7%, respectively:
Respiratory syncytial virus infection in elderly and high-risk adults
…but a new study this year has found the rates like to be 2.2x that, i.e. 15% intensive care rate and 18% mortality, respectively:
Want to know more?
Here are some hot-off-the-press news articles on the topic:
- Better awareness of RSV in older adults is needed to reduce hospitalizations
- Is there also a connection between RSV and asthma?
- Respiratory syncytial virus coinfections conspire to worsen disease
And as for what to do…
Same general advice as for COVID and Flu, just, ever-more important:
- Try to keep to well-ventilated places as much as possible
- Get any worrying symptoms checked out quickly
- Mask up when appropriate
- Get your shots as appropriate
See also:
Harvard Health Review | Fall shots: Who’s most vulnerable to RSV, COVID, and the flu, and which shots are the right choice for you to help protect against serious illness and hospitalization?
Stay safe!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
What To Do If Having A Stroke Alone?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small 😎
❝Thank you for the video about what to do if you have a heart attack alone, what about what to do if you have a stroke alone?❞
(for anyone who missed that video, here it is)
That’s a good question, especially as stroke risk is rising in the industrialized world in general, and the US in particular.
However, let’s start with the caveat that if you are having a stroke, there’s a good chance you will forget what we are about to say, what with the immediate effects it has on the brain. That said…
The general advice when it comes to looking after someone else who is experiencing a stroke, is, “don’t”.
In other words, call emergency services, and don’t do anything else, e.g:
- don’t give them anything to eat or drink
- don’t give them any medications
- don’t let them go to sleep
- don’t let them talk you out of calling emergency services
- don’t let them drive themselves to hospital
- don’t drive them to hospital yourself either*
*This is for two reasons:
- an ambulance crew has skills and resources that you don’t, and can begin treatment en-route, and also,
- not all hospitals have appropriate resources to treat stroke, so the ambulance crew will know to drive to one that does, instead of driving to a random hospital and hoping for the best
So, flipping this for if it’s you having the stroke, and you’re cognizant enough to remember this:
- do call an ambulance; stay on the line and don’t do anything else unless instructed by the emergency services.
In order to do that, of course it’s important to recognize the symptoms; you probably know these but just in case, the mnemonic is “FAST”:
- Face: is there weakness on one side of their face?
- Arms: if they raise both arms, does one drift downwards?
- Speech: if they speak, is their speech slurred or otherwise unusual?
- Time: to call emergency services
It’s great to not get caught out by surprise, so you might also want to check out:
6 Signs Of Stroke (One Month In Advance)
Take care!
Share This Post
-
The Worst Way to Wake Up (and What to Do Instead)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Not everyone is naturally inclined to be a morning person, but there are things we can do to make things go more easily for our brains!
Cause for alarm?
Dr. Tracey Marks, psychiatrist, explains the impact of our first moments upon awakening, and what that can do to/for us in terms of sleep inertia (i.e. grogginess).
Sleep inertia is worse when waking from deep sleep—and notably, we don’t naturally wake directly from deep sleep unless we are externally aroused (e.g. by an alarm clock).
Dr. Marks suggests the use of more gradual alarms, including those with soft melodies, perhaps birdsong or other similarly gentle things (artificial sunlight alarms are also good), to ease our transition from sleeping to waking. It might take us a few minutes longer to be woken from sleep, but we’re not going to spend the next hour in a bleary-eyed stupor.
For more details on these things and more (including why not to hit “snooze”), enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
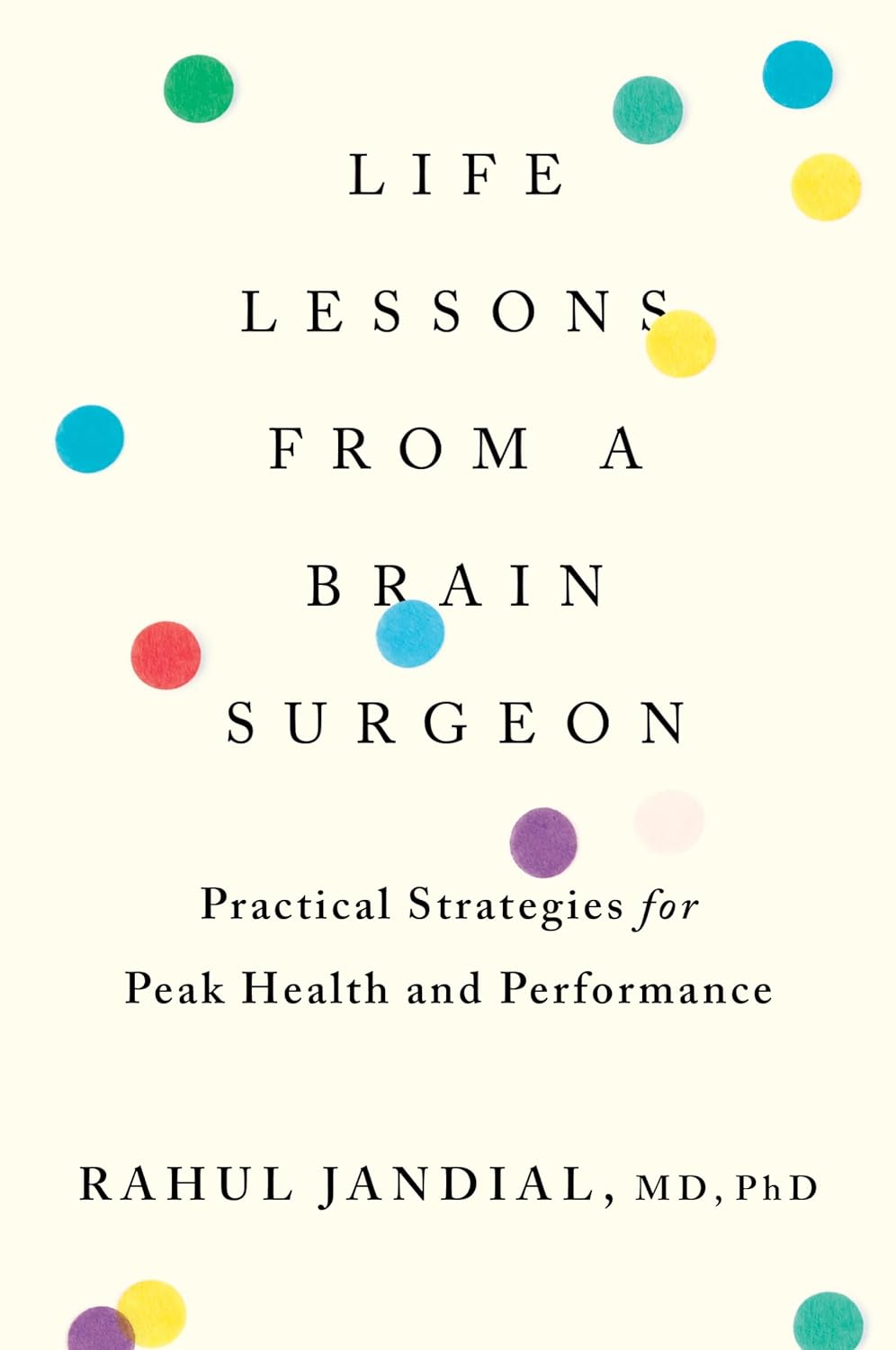
Life Lessons From A Brain Surgeon – by Dr. Rahul Jandial
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the category of surgeons with a “what to put on your table to stay off mine” angle, this book packs an extra punch. As well as being an experienced brain surgeon, Dr. Jandial also does a lot of cutting edge lab research too. What does this mean for us?
This book gives, as the subtitle promises, “practical strategies for peak health and performance”—with a brain-centric bias, of course.
From diet and nootropic supplements, to exercise and brain-training, we get a good science-based view of which ones actually work, and which don’t. The style is also very readable; Dr. Jandial is a great educator, presenting genuine scientific content with very accessible language.
Bottom line: if you’d indeed like to look after your most important organ optimally, this book gives a lot of key pointers, without unnecessary fluff.
Share This Post
Related Posts
-
Can You Step Backwards Without Your Foot Or Torso Turning Out?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Walking backwards is often overlooked, but research shows it can enhance forward walking, especially in stroke patients; it has other benefits for everyone else, too. The physiotherapists at Fitness4Life Physical Therapy explain:
…and one step back
How it works: walking backwards heightens proprioception and stimulates muscles, improving balance and posture. Additionally, our daily lives tend to involve forward-leaning postures, causing upper back bending, and walking backwards helps counterbalance this.
Extra benefits: training to walk backwards can reduce the risk of falls, as stepping back is a common movement that is often untrained.
Exercise: try doing backwards lunges, to assess your skill and balance while moving backward. If foot rotation or torso rotation occurs during the exercise, then there’s room for improvement. Correcting these movements is then simply a matter of practicing backward lunges without turning.
10almonds tip: any exercise is only as good as your will to actually do it. For this reason, dancing is a great exercise in this case, as almost all forms of dance involve stepping backwards (in order to have steps without travelling somewhere, forwards steps are usually balanced with backwards ones)
For more on all this, plus a visual demonstration of the exercise, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Fall Special ← About how to avoid falling, and how to avoid (and failing that, at least minimize) injury if you do fall. If you think this only happens to other/older people, remember, there’s a first time for everything, so it is better to be prepared in advance!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
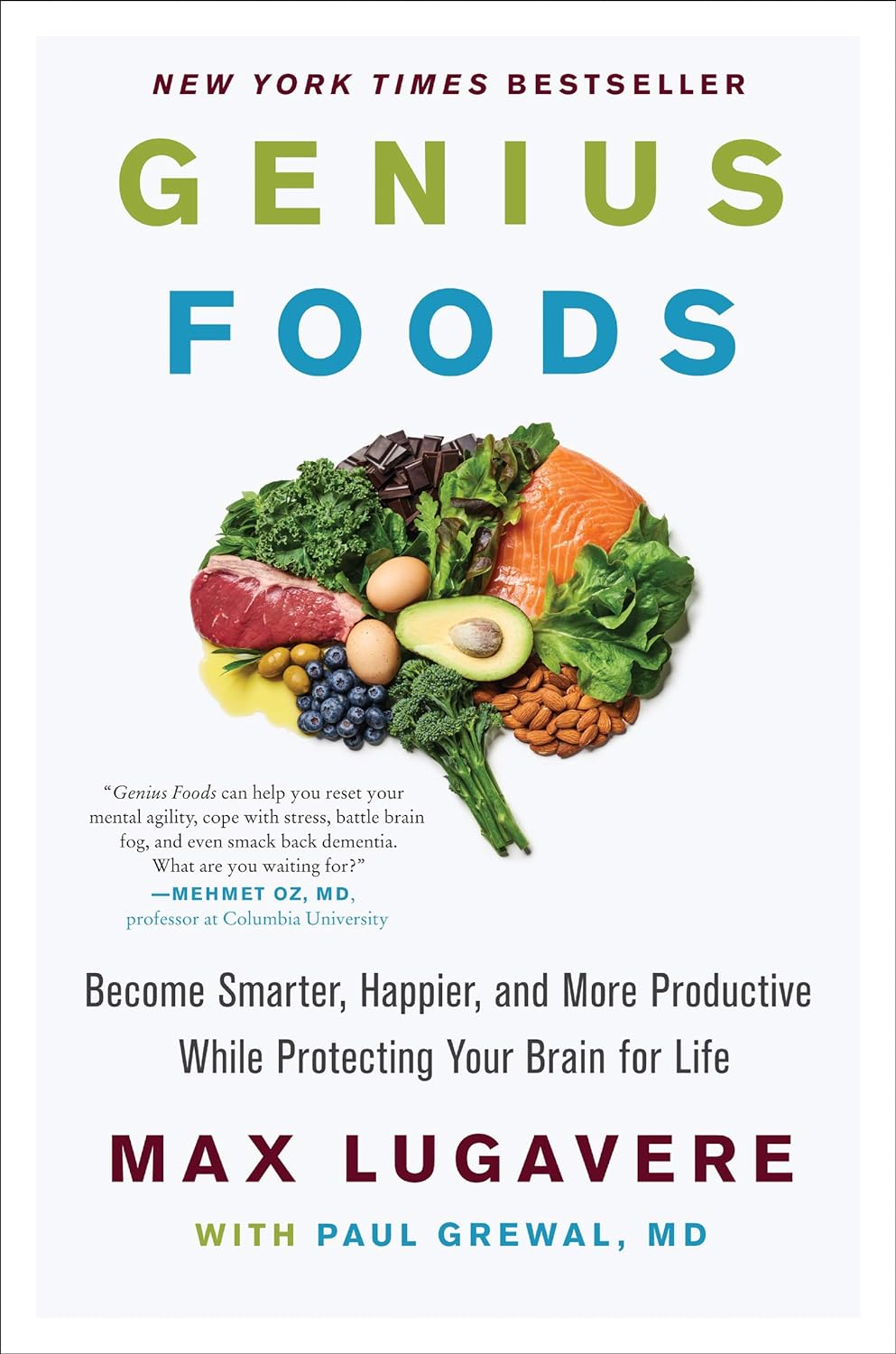
Genius Foods – by Max Lugavere
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is a lot of seemingly conflicting (or sometimes: actually conflicting!) information out there with regard to nutrition and various aspects of health. Why, for example, are we told:
- Be sure to get plenty of good healthy fats from nuts and seeds, for metabolic health and brain health too!
- But these terrible nut and seed oils lead to heart disease and dementia! Avoid them at all costs!
Max Lugavere demystifies this and more.
His science-led approach is primarily focused on avoiding dementia, and/but is at least not bad when it comes to other areas of health too.
He takes us on a tour of different parts of our nutrition, including:
- Perhaps the clearest explanation of “healthy” vs “unhealthy” fats this reviewer has read
- Managing carbs (simple and complex) for healthy glucose management—essential for good brain health
- What foods to improve or reduce—a lot you might guess, but this is a comprehensive guide to brain health so it’d be remiss to skip it
- The role that intermittent fasting can play as a bonus extra
While the main thrust of the book is about avoiding cognitive impairment in the long-term (including later-life dementia), he makes good, evidence-based arguments for how this same dietary plan improves cognitive function in the short-term, too.
Speaking of that dietary plan: he does give a step-by-step guide in a “make this change first, then this, then this” fashion, and offers some sample recipes too. This is by no means a recipe book though—most of the book is taking us through the science, not the kitchen.
Bottom line: this is the book for getting unconfused with regard to diet and brain health, making a lot of good science easy to understand. Which we love!
Click here to check out “Genius Foods” on Amazon today, give your brain a boost!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Tilapia vs Cod – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing tilapia to cod, we picked the tilapia.
Why?
Another case of “that which is more expensive is not necessarily the healthier”!
In terms of macros, tilapia has more protein and fats, as well as more omega-3 (and omega-6). On the downside, tilapia does have relatively more saturated fat, but at 0.94g/100g, it’s not exactly butter.
The vitamins category sees that tilapia has more of vitamins B1, B3, B5, B12, D, and K, while cod has more of vitamins B6, B9, and choline. A moderate win for tilapia.
When it comes to minerals, things are most divided; tilapia has more copper, iron, phosphorus, potassium, manganese, and selenium, while cod has more magnesium and zinc. An easy win for tilapia.
One other thing to note is that both of these fish contain mercury these days (and it’s worth noting: cod has nearly 10x more mercury). Mercury is, of course, not exactly a health food.
So, excessive consumption of either is not recommended, but out of the two, tilapia is definitely the one to pick.
Want to learn more?
You might like to read:
Farmed Fish vs Wild Caught: Know The Health Differences
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: