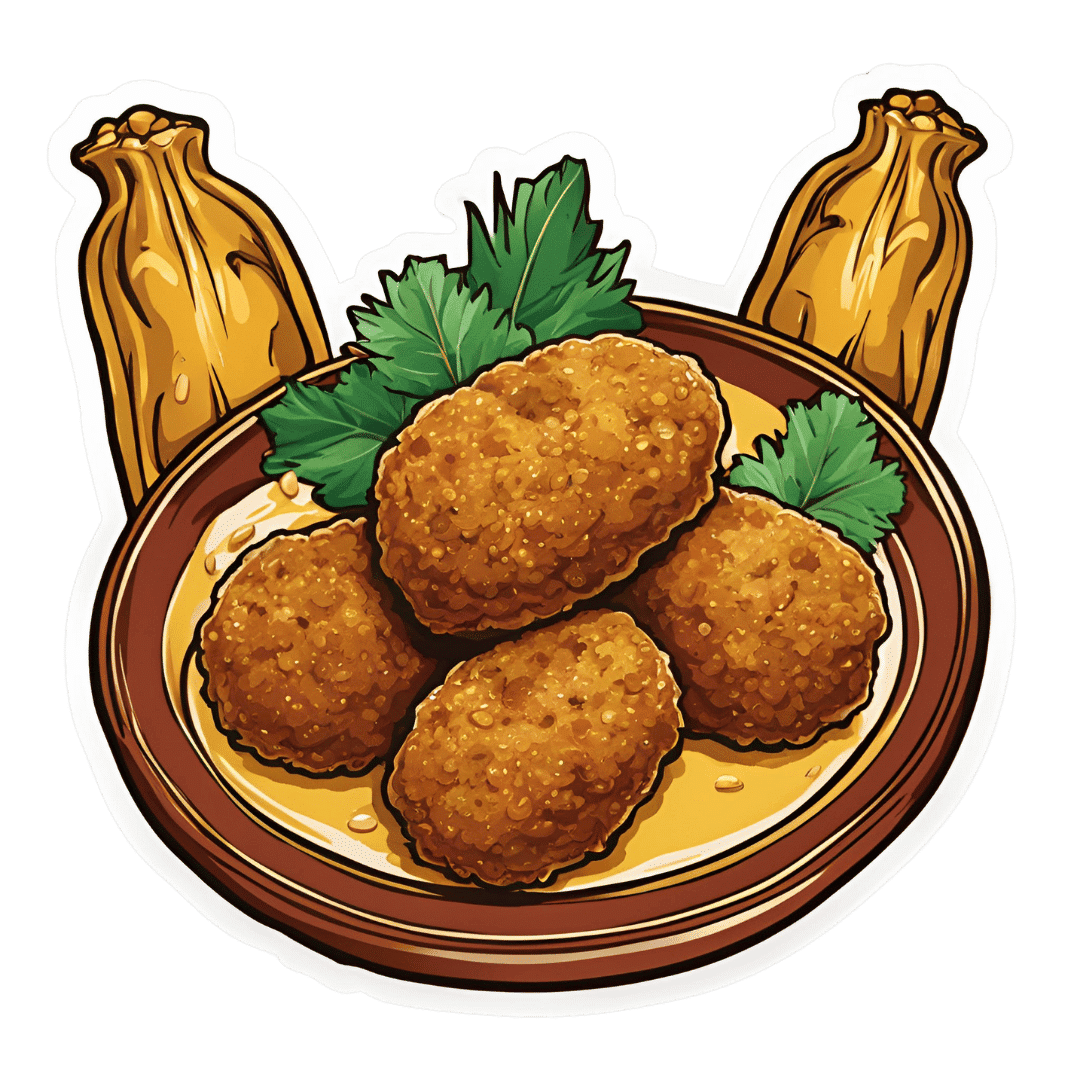
Zucchini & Oatmeal Koftas
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
These vegetarian (and with one tweak, vegan) koftas are delicious as a snack, light lunch, or side to a larger meal. Healthwise, they contain the healthiest kind of fiber, as well as omega-3 fatty acids, and beneficial herbs and spices.
You will need
- ¼ cup oatmeal
- 1 large zucchini, grated
- 1 small carrot, grated
- ¼ cup cheese (your preference; vegan is also fine)
- 2 tbsp ground flaxseed
- 2 tbsp nutritional yeast
- ¼ bulb garlic, minced
- 2 tsp black pepper, coarse ground
- ½ tsp MSG or 1 tsp low-sodium salt
- Small handful fresh parsley, chopped
- Extra virgin olive oil, for frying
Method
(we suggest you read everything at least once before doing anything)
1) Soak the flaxseed in 2 oz hot water for at least 5 minutes
2) Combine all of the ingredients except the olive oil (and including the water that the flax has been soaking in) in a big bowl, mixing thoroughly
3) Shape into small balls, patties, or sausage shapes, and fry until the color is golden and the structural integrity is good. If doing patties, you’ll need to gently flip them to cook both sides; otherwise, rolling them to get all sides is fine.
4) Serve! Traditional is with some kind of yogurt dip, but we’re not the boss of you, so enjoy them how you like:

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- The Best Kind Of Fiber For Overall Health? ← it’s β-glucan, as found in oats
- What Omega-3 Fatty Acids Really Do For Us ← as in the flax
- The Many Health Benefits Of Garlic
- Black Pepper’s Impressive Anti-Cancer Arsenal (And More)
- Monosodium Glutamate: Sinless Flavor-Enhancer Or Terrible Health Risk? ← it’s healthier than table salt
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Navigating the health-care system is not easy, but you’re not alone.
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hello, dear reader!
This is my first column for Healthy Debate as a Patient Navigator. This column will be devoted to providing patients with information to help them through their journey with the health-care system and answering your questions.
Here’s a bit about me: I have been a patient partner at The Ottawa Hospital and Ottawa Hospital Research Institute since 2017, and have joined a variety of governance boards that work on patient and caregiver engagement such as the Patient Advisors Network, the Ontario Health East Region Patient and Family Advisory Council and the Equity in Health Systems Lab.
My journey as a patient partner started much before 2017 though. When I was a teenager, I was diagnosed with a cholesteatoma, a rare and chronic disease that causes the development of fatty tumors in the middle ear. I have had multiple surgeries to try to fix it but will need regular follow-ups to monitor whether the tumor returns. Because of this, I also live with an invisible disability since I have essentially become functionally deaf in one ear and often rely on a hearing aid when I navigate the world.
Having undergone three surgeries in my adolescent years, it was my experience undergoing surgery for an acute hand and wrist injury following a jet ski accident as an adult that was the catalyst for my decision to become a patient partner. There was an intriguing contrast between how I was cared for at two different health-care institutions, my age being the deciding factor at which hospital I went to (a children’s hospital or an adult one).
The most memorable example was how, as a teenager or child, you were never left alone before surgery, and nurses and staff took all the time necessary to comfort me and answer my (and my family’s) questions. I also remember how right before putting me to sleep, the whole staff initiated a surgical pause and introduced themselves and explained to me what their role was during my surgery.
None of that happened as an adult. I was left in a hallway while the operating theater was prepared, anxious and alone with staff walking by not even batting an eye. My questions felt like an annoyance to the care team; as soon as I was wheeled onto the operating room table, the anesthetist quickly put me to sleep. I didn’t even have the time to see who else was there.
Now don’t get me wrong: I am incredibly appreciative with the quality of care I received, but it was the everyday interactions with the care teams that I felt could be improved. And so, while I was recovering from that surgery, I looked for a way to help other patients and the hospital improve its care. I discovered the hospital’s patient engagement program, applied, and the rest is history!
Since then, I have worked on a host of patient-centered policy and research projects and fervently advocate that surgical teams adopt a more compassionate approach with patients before and after surgery.
I’d be happy to talk a bit more about my journey if you ask, but with that out of the way … Welcome to our first patient navigator column about patient engagement.
Conceptualizing the continuum of Patient Engagement
In the context of Canadian health care, patient engagement is a multifaceted concept that involves active collaboration between patients, caregivers, health-care providers and researchers. It involves patients and caregivers as active contributors in decision-making processes, health-care services and medical research. Though the concept is not new, the paradigm shift toward patient engagement in Canada started around 2010.
I like to conceptualize the different levels of patient engagement as a measure of the strength of the relationship between patients and their interlocutors – whether it’s a healthcare provider, administrator or researcher – charted against the duration of the engagement or the scope of input required from the patient.
Defining different levels of Patient Engagement
Following the continuum, let’s begin by defining different levels of patient engagement. Bear in mind that these definitions can vary from one organization to another but are useful in generally labelling the level of patient engagement a project has achieved (or wishes to achieve).
Patient involvement: If the strength of the relationship between patients and their interlocutors is minimal and not time consuming or too onerous, then perhaps it can be categorized as patient involvement. This applies to many instances of transactional engagement.
Patient advisory/consulting: Right in the middle of our continuum, patients can find themselves engaging in patient advisory or consulting work, where projects are limited in scope and duration or complexity, and the relationship is not as profound as a partnership.
Patient partnership: The stronger the relationship is between the patient and their interlocutor, and the longer the engagement activity lasts or how much input the patient is providing, the more this situation can be categorized as patient partnership. It is the inverse of patient involvement.
Examples of the different levels of Patient Engagement
Let’s pretend you are accompanying a loved one to an appointment to manage a kidney disease, requiring them to undergo dialysis treatment. We’ll use this scenario to exemplify what label could be used to describe the level of engagement.
Patient involvement: In our case, if your loved one – or you – fills out a satisfaction or feedback survey about your experience in the waiting room and all that needed to be done was to hand it back to the clerk or care team, then, at a basic level, you could likely label this interaction as a form of patient involvement. It can also involve open consultations around a design of a new look and feel for a hospital, or the understandability of a survey or communications product. Interactions with the care team, administrators or researchers are minimal and often transactional.
Patient advisory/consulting: If your loved one was asked for more detailed information about survey results over the course of a few meetings, this could represent patient advisory/consulting. This could mean that patients meet with program administrators and care providers and share their insights on how things can be improved. It essentially involves patients providing advice to health-care institutions from the perspective of patients, their family members and caregivers.
Patient advisors or consultants are often appointed by hospitals or academic institutions to offer insights at multiple stages of health-care delivery and research. They can help pilot an initiative based on that feedback or evaluate whether the new solutions are working. Often patient advisors are engaged in smaller-term individual projects and meet with the project team as regularly as required.
Patient partnership: Going above and beyond patient advisory, if patients have built a trusting relationship with their care team or administrators, they could feel comfortable enough to partner with them and initiate a project of their own. This could be for a project in which they study a different form of treatment to improve patient-centered outcomes (like the time it takes to feel “normal” following a session); it could be working together to identify and remove barriers for other patients that need to access that type of care. These projects are not fulfilled overnight, but require a collaborative, longstanding and trusting relationship between patients and health-care providers, administrators or researchers. It ensures that patients, regardless of severity or chronicity of their illness, can meaningfully contribute their experiences to aid in improving patient care, or develop or implement policies, pilots or research projects from start to finish.
It is leveraging that lived and living experience to its full extent and having the patient partner involved as an equal voice in the decision-making process for a project – over many months, usually – that the engagement could be labeled a partnership.
Last words
The point of this column will be to answer or explore issues or questions related to patient engagement, health communications or even provide some thoughts on how to handle a particular situation.
I would be happy to collect your questions and feedback at any time, which will help inform future columns. Just email me at [email protected] or connect with me on social media (Linked In, X / Twitter).
It’s not easy to navigate our health-care systems, but you are not alone.
This article is republished from healthydebate under a Creative Commons license. Read the original article.
Share This Post
-
Ruminating vs Processing
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
When it comes to traumatic experiences, there are two common pieces of advice for being able to move forwards functionally:
- Process whatever thoughts and feelings you need to process
- Do not ruminate
The latter can seem, at first glance, a lot like the former. So, how to tell them apart, and how to do one without the other?
Getting tense
One major difference between the two is the tense in which our mental activity takes place:
- processing starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if possible why, and then asks the question “ok, what now?” and begins work on laying out a path for the future.
- rumination starts with the traumatic event (or perhaps even the events leading up to the traumatic event), analyses what happened and if why, oh why oh why, “I was such an idiot, if only I had…” and gets trapped in a fairly tight (and destructive*) cycle of blame and shame/anger, never straying far from the events in question.
*this may be directly self-destructive, but it can also sometimes be only indirectly self-destructive, for example if the blame and anger is consciously placed with someone else.
This idea fits in, by the way, with Dr. Elisabeth Kübler-Ross’s “five stages of grief” model; rumination here represents the stages “bargaining”, “despair”, and “anger”, while emotional processing here represents the stage “acceptance”. Thus, it may be that rumination does have a place in the overall process—just don’t get stuck there!
For more on healthily processing grief specifically:
What Grief Does To The Body (And How To Manage It)
Grief, by the way, can be about more than the loss of a loved one; a very similar process can play out with many other kinds of unwanted life changes too.
What are the results?
Another way to tell them apart is to look at the results of each. If you come out of a long rumination session feeling worse than when you started, it’s highly unlikely that you just stopped too soon and were on the verge of some great breakthrough. It’s possible! But not likely.
- Processing may be uncomfortable at first, and if it’s something you’ve ignored for a long time, that could be very uncomfortable at first, but there should quite soon be some “light at the end of the tunnel”. Perhaps not even because a solution seems near, but because your mind and body recognize “aha, we are doing something about it now, and thus may find a better way forward”.
- Rumination tends to intensify and prolong uncomfortable emotions, increases stress and anxiety, and likely disrupts sleep. At best, it may serve as a tipping point to seek therapy or even just recognize “I should figure out a way to deal with this, because this isn’t doing me any good”. At worst, it may serve as a tipping point to depression, and/or substance abuse, and/or suicidality.
See also: How To Stay Alive (When You Really Don’t Want To) ← which also has a link back to our article on managing depression, by the way!
Did you choose it, really?
A third way to tell them apart is the level of conscious decision that went into doing it.
- Processing is almost always something that one decides “ok, let’s figure this out”, and sits down to figure it out.
- Rumination tends to be about as voluntary as social media doomscrolling. Technically we may have decided to begin it (we also might not have made any conscious decision, and just acted on impulse), but let’s face it, our hands weren’t at the wheel for long, at all.
A good way to make sure that it is a conscious process, is to schedule time for it in advance, and then do it only during that time. If thoughts about it come up at other times, tell yourself “no, leave that for later”, and then deal with it when (and only when) the planned timeslot arrives.
It’s up to you and your schedule what time you pick, but if you’re unsure, consider an hour in the early evening. That means that the business of the day is behind you, but it’s also not right before bed, so you should have some decompression time as a buffer. So for example, perhaps after dinner you might set a timer* for an hour, and sit down to journal, brainstorm, or just plain think, about the matter that needs processing.
*electronic timers can be quite jarring, and may distract you while waiting for the beeps. So, consider investing in a relaxing sand timer like this one instead.
Is there any way to make rumination less bad?
As we mentioned up top, there’s a case to be made for “rumination is an early part of the process that gets us where we need to go, and may not be skippable, or may not be advisable to skip”.
So, if you are going to ruminate, then firstly, we recommend again bordering it timewise (with a timer as above) and having a plan to pull yourself out when you’re done rather than getting stuck there (such as: The Off-Button For Your Brain: How To Stop Negative Thought Spirals).
And secondly, you might want to consider the following technique, which allows one to let one’s brain know that the thing we’re thinking about / imagining is now to be filed away safely; not lost or erased, but sent to the same place that nightmares go after we wake up:
A Surprisingly Powerful Tool: Eye Movement Desensitization & Reprocessing (EMDR)
What if I actually do want to forget?
That’s not usually recommendable; consider talking it through with a therapist first. However, for your interest, there is a way:
The Dark Side Of Memory (And How To Forget)
Take care!
Share This Post
-
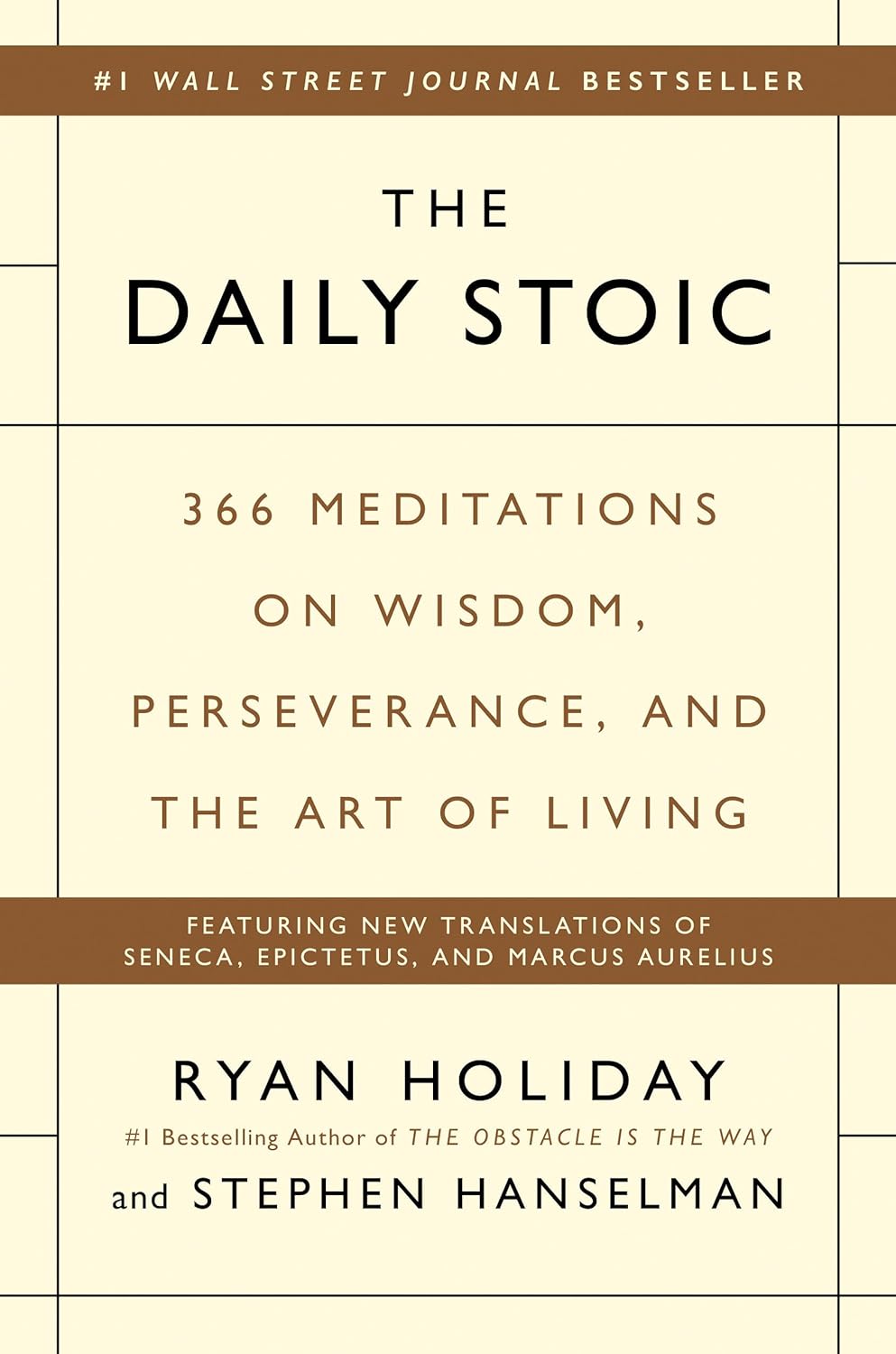
The Daily Stoic – by Ryan Holiday & Stephen Hanselman
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s this, a philosophy book in a health and productivity newsletter? Well, look at it this way: Aristotle basically wrote the “How To Win Friends And Influence People” of his day, and Plato before him wrote a book about management.
In this (chiefly modern!) book, we see what the later Stoic philosophers had to say about getting the most out of life—which is also what we’re about, here at 10almonds!
We tend to use the word “stoic” in modern English to refer to a person who is resolute in the face of hardship. The traditional meaning does encompass that, but also means a lot more: a whole, rounded, philosophy of life.
Philosophy in general is not an easy thing into which to “dip one’s toe”. No matter where we try to start, it seems, it turns out there were a thousand other things we needed to read first!
This book really gets around that. The format is:
- There’s a theme for each month
- Each month has one lesson per day
- Each daily lesson starts with some words from a renowned stoic philosopher, and then provides commentary on such
- The commentary provides a jumping-off point and serves as a prompt to actually, genuinely, reflect and apply the ideas.
Unlike a lot of “a year of…” day-by-day books, this is not light reading, by the way, and you are getting a weighty tome for your money.
But, the page-length daily lessons are indeed digestible—which, again, is what we like at 10almonds!
Share This Post
Related Posts
-
Our ‘food environments’ affect what we eat. Here’s how you can change yours to support healthier eating
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In January, many people are setting new year’s resolutions around healthy eating. Achieving these is often challenging – it can be difficult to change our eating habits. But healthy diets can enhance physical and mental health, so improving what we eat is a worthwhile goal.
One reason it’s difficult to change our eating habits relates to our “food environments”. This term describes:
The collective physical, economic, policy and sociocultural surroundings, opportunities and conditions that influence people’s food and beverage choices and nutritional status.
Our current food environments are designed in ways that often make it easier to choose unhealthy foods than healthy ones. But it’s possible to change certain aspects of our personal food environments, making eating healthier a little easier.
Unhealthy food environments
It’s not difficult to find fast-food restaurants in Australian cities. Meanwhile, there are junk foods at supermarket checkouts, service stations and sporting venues. Takeaway and packaged foods and drinks routinely come in large portion sizes and are often considered tastier than healthy options.
Our food environments also provide us with various prompts to eat unhealthy foods via the media and advertising, alongside health and nutrition claims and appealing marketing images on food packaging.
At the supermarket, unhealthy foods are often promoted through prominent displays and price discounts.
We’re also exposed to various situations in our everyday lives that can make healthy eating challenging. For example, social occasions or work functions might see large amounts of unhealthy food on offer.
Not everyone is affected in the same way
People differ in the degree to which their food consumption is influenced by their food environments.
This can be due to biological factors (for example, genetics and hormones), psychological characteristics (such as decision making processes or personality traits) and prior experiences with food (for example, learned associations between foods and particular situations or emotions).
People who are more susceptible will likely eat more and eat more unhealthy foods than those who are more immune to the effects of food environments and situations.
Those who are more susceptible may pay greater attention to food cues such as advertisements and cooking smells, and feel a stronger desire to eat when exposed to these cues. Meanwhile, they may pay less attention to internal cues signalling hunger and fullness. These differences are due to a combination of biological and psychological characteristics.
These people might also be more likely to experience physiological reactions to food cues including changes in heart rate and increased salivation.
It’s common to eat junk food in front of the TV.
PR Image Factory/ShutterstockOther situational cues can also prompt eating for some people, depending on what they’ve learned about eating. Some of us tend to eat when we’re tired or in a bad mood, having learned over time eating provides comfort in these situations.
Other people will tend to eat in situations such as in the car during the commute home from work (possibly passing multiple fast-food outlets along the way), or at certain times of day such as after dinner, or when others around them are eating, having learned associations between these situations and eating.
Being in front of a TV or other screen can also prompt people to eat, eat unhealthy foods, or eat more than intended.
Making changes
While it’s not possible to change wider food environments or individual characteristics that affect susceptibility to food cues, you can try to tune into how and when you’re affected by food cues. Then you can restructure some aspects of your personal food environments, which can help if you’re working towards healthier eating goals.
Although both meals and snacks are important for overall diet quality, snacks are often unplanned, which means food environments and situations may have a greater impact on what we snack on.
Foods consumed as snacks are often sugary drinks, confectionery, chips and cakes. However, snacks can also be healthy (for example, fruits, nuts and seeds).
Try removing unhealthy foods, particularly packaged snacks, from the house, or not buying them in the first place. This means temptations are removed, which can be especially helpful for those who may be more susceptible to their food environment.
Planning social events around non-food activities can help reduce social influences on eating. For example, why not catch up with friends for a walk instead of lunch at a fast-food restaurant.
Creating certain rules and habits can reduce cues for eating. For example, not eating at your desk, in the car, or in front of the TV will, over time, lessen the effects of these situations as cues for eating.
You could also try keeping a food diary to identify what moods and emotions trigger eating. Once you’ve identified these triggers, develop a plan to help break these habits. Strategies may include doing another activity you enjoy such as going for a short walk or listening to music – anything that can help manage the mood or emotion where you would have typically reached for the fridge.
Write (and stick to) a grocery list and avoid shopping for food when hungry. Plan and prepare meals and snacks ahead of time so eating decisions are made in advance of situations where you might feel especially hungry or tired or be influenced by your food environment.
Georgie Russell, Senior Lecturer, Institute for Physical Activity and Nutrition (IPAN), Deakin University and Rebecca Leech, NHMRC Emerging Leadership Fellow, School of Exercise and Nutrition Sciences, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
10 Ways To Lower Blood Pressure Naturally
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Increasingly many people, especially over a certain age, are taking so many medications that it precipitates a train of other medications to deal with the side effects of the previous ones. This is neither fun nor healthy. Of course, sometimes it’s a necessity, but often it’s not, so if you’d like to avoid blood pressure meds, here are some good first-line things, as recommended by Dr. Siobhan Deshauer:
No-med options
Dr. Deshauer recommends:
- Diet: follow the DASH diet by eating whole foods, lean / plant-based proteins, and reducing salt and processed foods to lower blood pressure by 5–6 points.
- Sodium reduction: limit sodium intake to 2g/day, focusing on reducing processed foods, which account for 80% of sodium consumption.
- Increase potassium intake: eat potassium-rich foods (e.g. fruit, vegetables) to lower blood pressure by 5–7 points but consult a doctor if you have kidney issues or take certain medications.
- Exercise: engage in isometric exercises like wall squats or planks, which lower systolic pressure by up to 8 points; any exercise is beneficial.
- Weight loss: lose weight (specifically: fat) if (and only if!) carrying excess fat, as each 1 kg (2.2 lbs) excess adiposity reduction can decrease blood pressure by 1 point.
- Limit alcohol: avoid consuming more than two alcoholic drinks per day, as it raises blood pressure.
- Quit smoking: stop smoking to prevent increased blood pressure and long-term vessel damage caused by nicotine.
- Improve sleep: aim for at least 6 hours of sleep per night, ideally 7–9, and seek medical advice if you suspect sleep apnea.
- Manage stress: adopt healthy stress management strategies to avoid the indirect effects of stress on blood pressure.
- Adopt a pet: pet ownership, particularly dogs, can lower blood pressure more effectively than some medications.
For more on each of these, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Ideal Blood Pressure Numbers Explained
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
How To Gain Weight (Healthily!)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What Do You Have To Gain?
We have previously promised a three-part series about changing one’s weight:
- Losing weight (specifically, losing fat)
- Gaining weight (specifically, gaining muscle)
- Gaining weight (specifically, gaining fat)
There will be, however, no need for a “losing muscle” article, because (even though sometimes a person might have some reason to want to do this), it’s really just a case of “those things we said for gaining muscle? Don’t do those and the muscle will atrophy naturally”.
Here’s our first article: How To Lose Weight (Healthily!)
While some people will want to lose fat, please do be aware that the association between weight loss and good health is not nearly so strong as the weight loss industry would have you believe:
And, while BMI is not a useful measure of health in general, it’s worth noting that over the age of 65, a BMI of 27 (which is in the high end of “overweight”, without being obese) is associated with the lowest all-cause mortality:
BMI and all-cause mortality in older adults: a meta-analysis
Here was our second article: How To Build Muscle (Healthily!)
And now, it’s time for the last part, which yes, is also something that some people want/need to do (healthily!), and want/need help with that.
How to gain fat, healthily
Fat gets a bad press, but when it comes to health, we would die without it.
Even in the case of having excess fat, the fat itself is not generally the problem, so much as comorbid metabolic issues that are often caused by the same things as the excess fat.
So, how to gain fat healthily?
- Obvious but potentially dangerously misleading answer: “in moderation”
- More useful answer: “carefully”
Because, you can “in moderation” put on less than one pound per week for a few years and be in very bad health by the end of it. So how does this “carefully” work any differently to “in moderation”?
The key is in how we store the fat
Not merely where we store it (though that’ll follow from the “how”), but specifically: how we store it.
- When we consume energy from food in excess of our immediate survival needs, our body stores what it can. This is good!
- When our body is receiving energy from food faster than it can physically process it to store it healthily, it will start shoving it wherever it can instead. This is bad!
This is the physiological equivalent of the difference between tidying a room carefully, and cramming everything into one cupboard in 30 seconds just to get it out of sight.
So, you do need to consume calories yes, but you need to consume them in a way your body can take its time about storing them.
We’ve written before about the science of this, so we’ll share some links, but first, here are the practical tips:
- Do not drink your calories. Drinking calories tends to be the equivalent of injecting sugars directly into your veins, in terms of how quickly it gets received.
- See also: How To Unfatty A Fatty Liver ← this is highly relevant, because the same process that results in unhealthy weight gain, results in liver disease, by the same mechanism (the liver gets overwhelmed).
- Eat your greens. No, they won’t provide many calories, but they are critical to your body not being overwhelmed by the arrival of sugars.
- See also: 10 Ways To Balance Blood Sugars ← the other 9 things are also helpful for not putting on fat unhealthily, so using these alongside a calorie-dense diet can result in healthy fat gain as needed
- Get more of your calories from fats than carbs. Fats will not overwhelm your body’s glycemic response in the same way that carbs will.
- Again this is about getting calories while not getting metabolic disease. See also: How To Prevent And Reverse Type Two Diabetes as the advice is the same for that, for the same reason!
- Consider going low-carb, but even if you choose not to, go for carbs with a low glycemic index instead of a high glycemic index.
- For reference, see: Glycemic Index Chart: Glycemic index and glycemic load ratings for 500+ foods
- Need healthy fats in a snack? Enjoy nuts (unless you have an allergy); they will be your best friend in this regard. As an example, a mere 1oz portion of cashew nuts has 157 calories.
- See also: Why You Should Diversify Your Nuts
- Need healthy fats for cooking? Enjoy olive oil, as it has one of the healthiest lipids profiles available, and is a great way to increase the calorific content of many meals.
Lastly…
Be patient, enjoy your food, and stick as best you can to the above considerations. All strength to you.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: