Take This Two-Minute Executive Dysfunction Test
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Roll For Initiative
Some of us struggle with executive dysfunction a lot; others, a little.
What Is Executive Dysfunction?
• Executive function is a broad group of mental skills that enable people to complete tasks and interact with others.
• Executive dysfunction can impair a person’s ability to organize and manage behavior
• Executive dysfunction is not a specific stand-alone diagnosis or condition.
• Instead, conditions such as depression and ADHD (amongst others) can affect a person’s executive function.
Take This Two-Minute Executive Dysfunction Test
How did you score? (8/16 here!)
Did you do it? (it honestly is really two minutes and is quite informative)
If not, here’s your cue to go back up and do it
For almost all of us, we sometimes find ourselves torn between several competing tasks, and end up doing… none of them.
For such times, compile yourself a “productivity buffet”, print it, and pin it above your desk or similar space.
What’s a productivity buffet?
It’s a numbered list of 6, 8, 10, 12 or 20 common tasks that pretty much always need doing (to at least some extent!). Doesn’t matter how important they are, just that they are frequently recurring tasks. For example:
- Tidy desk (including that drawer!)
- Reply to emails/messages
- Drink water
- Collect stray one-off to-dos into a list
- Stretch (or at least correct your posture!)
- Extend that Duolingo streak
- Read one chapter of a book
- Etc
Why 6, 8, 10, 12, or 20?
Because those are common denominations of polyhedral dice that are very cheap to buy!
Keep the relevant die to hand (perhaps in your pocket or on your desk), and when you know you should be doing something but can’t decide what exactly, roll the die and do the item corresponding to the number you roll.
And if you find yourself thinking “damn, I got 12, I wanted 7!” then go ahead and do item 7—the dice aren’t the boss of you, they’re just there to break the ice between you and your to-do list!
The Housekeeper In Your Pocket?
If you found the tidying tips (up top) helpful, but don’t like cleaning schedules because you just can’t stick to them, this one’s for you.
It’s easy to slip into just doing the same few easy tasks while neglecting others for far too long.
The answer? Outsource!
Not “get a cleaner” (though if you want to and can, great, go for it, this one won’t be for you after all), but rather, try this nifty little app that helps you keep on top of daily cleaning—which we all know is better than binge-cleaning every few months.
Sweepy keeps track of:
- What jobs there are that might need doing in each room (or type of room) in the house
- How often those jobs generally need doing
- How much of your energy (a finite resource, which it also takes into account!) those jobs will take
- How much energy you are prepared to spend per day (you can “lighter/heavier” days, or even “off-days”, too)
…and then it populates a small daily task list according to what needs cleaning and how much energy it’ll take.
For example, today Sweepy gives me (your trusty writer, hi! ) the tasks:
- Bathroom: clean sink (every 3 days, 1pt of energy)
- Dining room: clean and tidy table (every day, 1pt of energy)
- Bedroom: vacuum floor (every 7 days, 2pts of energy)
- Kitchen: clean coffee machine (every 30 days, 2pts of energy)
And that’s my 6pts of energy I’ve told Sweepy I’m happy to spend per day cleaning. There are “3 pts” tasks too—cleaning the oven, for example—but none came up today.
Importantly: it does not bother me about any other tasks today (even if something’s overdue), and I don’t have to worry my pretty head about it.
I don’t have to feel guilty for not doing other cleaning tasks; if they need doing, Sweepy will tell me tomorrow, and it will make sure I don’t get behind or leave anything neglected for too long.
Check it out (available for both iOS and Android)
PS: to premium or not to premium? We think the premium is worth it (unlocks some extra customization features) but the free version is sufficient to get your house in order, so don’t be afraid to give it a try first.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

No-Frills, Evidence-Based Mindfulness
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s on your mind, really?
We hear a lot about “the evidence-based benefits of mindfulness”, but what actually are they? And what is the evidence? And, perhaps most importantly: how do we do it?
What are the benefits?
The benefits of mindfulness are many, and include:
- reducing stress
- reducing pain
- improving quality of life
- reducing fatigue
- providing relief from digestive disorders
- reducing symptoms of sleep disorders
- improving immune response
- providing support for caregivers
The evidence is also abundant, and includes:
- Effects of mindfulness exercises as stand-alone intervention on symptoms of anxiety and depression: Systematic review and meta-analysis
- Fusing character strengths and mindfulness interventions: Benefits for satisfaction and performance
- Evidence for the Role of Mindfulness in Cancer: Benefits and Techniques
- Effects of mindfulness-based stress reduction on anxiety symptoms: A systematic review and meta-analysis
- The benefits of meditation and mindfulness practices during times of crisis such as COVID-19
Sounds great… What actually is it, though?
Mindfulness is the state of being attentive to one’s mind. This is at its heart a meditative practice, but that doesn’t necessarily mean you have to be sitting in the lotus position with candles—mindfulness can be built into any daily activity, or even no activity at all.
An exercise you can try right now:
Take a moment to notice everything you can hear. For this writer, that includes:
- The noise of my keystrokes as I type
- The ticking of the clock on the wall
- The gentle humming of my computer’s processor
- The higher-pitched noise of my computer’s monitor
- Birdsong outside
- Traffic further away
- My own breathing
- The sound of my eyelids as I blink
Whatever it is for you, notice how much you can notice that you had previously taken for granted.
You can repeat this exercise with other senses, by the way! For example:
- Notice five things you can see in your immediate environment that you’ve never noticed before. If you’re at home reading this, you probably think you’re very familiar with everything around you, but now see that mark on the wall you’d never noticed before, or a quirk of some electrical wiring, or the stitching on some furnishing, for example.
- Notice the textures of your clothes, or your face, or perhaps an object you’ve never paid attention to touching before. Your fingertips, unless you have some special reason this doesn’t apply to you, are far more sensitive than you probably give them credit for, and can notice the tiniest differentiation in textures, so take a moment to do that now.
- Mindful eating can be an especially healthful practice because it requires that we pay every attention to what we’re putting in our mouth, tasting, chewing, swallowing. No more thoughtlessly downing a box of cookies; every bite is now an experience. On the one hand, you’ll probably eat less at a sitting. On the other hand, what a sensory experience! It really reminds one that life is for living, not just for zipping through at a speed-run pace!
What about mindfulness as a meditative practice?
Well, those are meditative practices! But yes, mindfulness goes for more formal meditation too. For example:
Sit comfortably, with good posture, whatever that means to you. No need to get too caught up in the physical mechanics here—it’d take a whole article. For now, if you’re sitting and comfortable, that’s enough.
Notice your breathing. No need to try to control it—that’s not what this is about today. Just notice it. The in, the out, whether you breathe to your chest or abdomen, through your nose or mouth, don’t worry about doing it “right”, just notice what you are doing. Observe without judgement.
Notice your thoughts—no need to try to stop them. Notice noticing your thoughts, and again, observe without judgement. Notice your feelings; are you angry, hopeful, stressed, serene? There are no wrong answers here, and there’s nothing you should try to “correct”. Just observe. No judgement, only observe. Watch your thoughts, and watch your thoughts go.
Did you forget about your breathing while watching your thoughts? Don’t worry about that either if so, just notice that it happened. If you have any feelings about that, notice them too, and carry on observing.
We go through so much of our lives in “autopilot”, that it can be an amazing experience to sometimes just “be”—and be aware of being.
Share This Post

Butter vs Margarine
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Butter vs Margarine

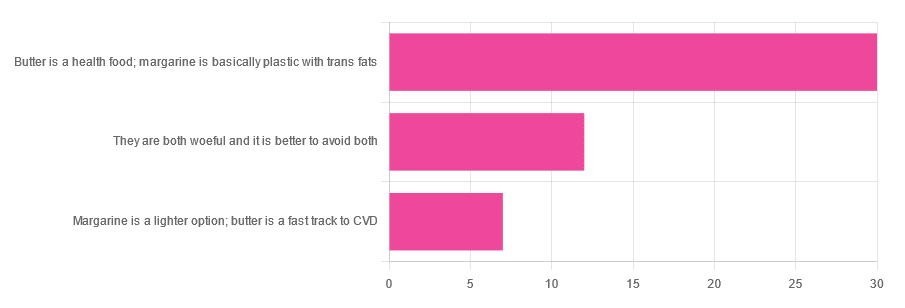
Yesterday, we asked you for your (health-related) opinion on butter vs margarine, and got the above-depicted, below-described, set of responses:
- A little over 60% said butter is a health food and margarine is basically plastic with trans fats
- A little over 20% said that both are woeful and it’s better to avoid both
- A little over 10% said that margarine is a lighter option, and butter is a fast track to cardiovascular disease.
Comments included (we will summarize/paraphrase, for space):
- “…in moderation, though”
- “I’m vegan so I use vegan butter but I know it’s not great, so I use it sparingly”
- “butter is healthy if and only if it’s grass-fed”
- “margarine has unpronounceable ingredients”
To address those quickly:
- “…in moderation” is a stipulation with which one can rarely go too far wrong
- Same! Speaking for myself (your writer here, hi) and not for the company
- Grass-fed is indeed better; alas that so little of it is grass-fed, in the US!
- Butter contains eicosatrienoic acid, linolelaidic acid, and more*. Sometimes big words don’t mean that something is worse for the health, though!
So, what does the science say?
Butter is a health food: True or False?
True or False, depending on amount! Moderation is definitely key, but we’ll return to that (and why not to have more than a small amount of butter) later. But it is a rich source of many nutrients, iff it’s grass-fed, anyway.
The nutritional profile of something isn’t a thing that’s too contentious, so rather than take too much time on it, in this case we’ll point you back up to the scientific paper we linked above, or if you prefer a pop-science rendering, here’s a nice quick rundown:
7 Reasons to Switch to Grass-Fed Butter
Margarine is basically plastic with trans fats: True or False?
False and usually False now, respectively, contingently.
On the first part: chemically, it’s simply not “basically plastic” and everything in it is digestible
On the second part: it depends on the margarine, and here’s where it pays to read labels. Historically, margarines all used to be high in trans fats (which are indeed woeful for the health). Nowadays, since trans fats have such a (well-earned) bad press, there are increasingly many margarines with low (or no) trans fats, and depending on your country, it may be that all margarines no longer have such:
❝It’s a public health success story. Consumers no longer have to worry about reading product nutritional labels to see if they contain hydrogenated oils and trans fats. They can just know that they no longer do❞
Source: Margarines now nutritionally better than butter after hydrogenated oil ban
So this is one where the science is clear (trans fats are unequivocally bad), but the consumer information is not always (it may be necessary to read labels, to know whether a margarine is conforming to the new guidelines).
Butter is a fast track to cardiovascular disease: True or False?
True or False depending on amount. In moderation, predictably it’s not a big deal.
But for example, the World Health Organization recommends that saturated fats (of which butter is a generous source) make up no more than 10% of our calorie intake:
Source: Saturated fatty acid and trans-fatty acid intake for adults and children: WHO guideline
So if you have a 2000 kcal daily intake, that would mean consuming not more than 200 kcal from butter, which is approximately two tablespoons.
If you’d like a deeper look into the complexities of saturated fats (for and against), you might like our previous main feature specifically about such:
Can Saturated Fats Be Healthy?
Enjoy!
Share This Post

Exercises for Aging-Ankles
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Can Ankles Deterioration be Stopped?
As we all know (or have experienced!), Ankle mobility deteriorates with age.
We’re here to argue that it’s not all doom and gloom!
(In fact, we’ve written about keeping our feet, and associated body parts, healthy here).
This video by “Livinleggings” (below) provides a great argument that yes, ankle deterioration can be stopped, or even reversed. It’s a must-watch for anyone from yoga enthusiasts to gym warriors who might be unknowingly crippling their ankle-health.
How We Can Prioritise Our Ankles
Poor ankle flexibility isn’t just an inconvenience – it’s a direct route to knee issues, hip hiccups, and back pain. More importantly, ankle strength is a core component of building overall mobility.
With 12 muscles in the ankle, it can be overwhelming to work out which to strengthen – and how. But fear not, we can prioritise three of the twelve: the calf duo (gastrocnemius and soleus) and the shin’s main muscle, the tibialis anterior.
The first step is to test yourself! A simple wall test reveals any hidden truths about your ankle flexibility. Go to the 1:55 point in the video to see how it’s done.
If you can’t do it, you’ve got work to be done.
If you read the book we recommended on great functional exercises for seniors, then you may already be familiar with some super ankle exercises.
Otherwise, these four ankle exercises are a great starting point:
How did you find that video? If you’ve discovered any great videos yourself that you’d like to share with fellow 10almonds readers, then please do email them to us!
Share This Post
Related Posts

Gravitas – by Caroline Goyder
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A no-nonsense guide to (more than!) public speaking that isn’t just “tell jokes in your speech and imagine the audience naked”.
Because this isn’t just about speech-writing or speech delivery, so much as giving you important life skills. The kind that weren’t taught in school, but that nevertheless make a huge impact on success… whether you’re giving a presentation or hosting a party or negotiating a deal or just attending a social event. Or making a phonecall, even.
Whereas a lot of books of this kind treat “the audience” as a nebulous and purely responsive passive crowd of extras, Goyder does better. People are individuals, even if they’re all facing the same way for a moment. She works with that! She also teaches how to deal with not just hecklers, but also simply those people who sap your confidence and find fault with you and anything you do or say.b
Bottom line is: if you for whatever reason communicate with people, and would like them to think better of you, this is the book for you.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Brain Power – by Michael Gelb & Kelly Howell
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What’s most important when it comes to brain health? Is it the right diet? Supplements? Brain-training? Attitude? Sleep? Physical exercise? Social connections? Something else?
This book covers a lot of bases, including all of the above and more. The authors are not scientists by training and this is not a book of science, so much as a book of aggregated science-based advice from other sources. The authors did consult with many scientists, and their input is shown throughout.
In the category of criticism, nothing here goes very deeply into the science, and there’s also nothing you wouldn’t find we’ve previously written about in a 10almonds article somewhere. But all the same, it’s good to have a wide variety of brain-healthy advices all in one place.
Bottom line: if you’re looking for a one-stop-shop “look after your brain as you age” guide, then this is a good one.
Click here to check out Brain Power, and improve your mind as you age!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:

Wise Old Fool
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
How old is this dish? Well, let’s put it this way, it used to be called ” ” and remnants of it have been found at neolithic burial sites in Egypt. Nowadays it’s called “فول مدمس”, which gets rendered a lot of different ways in the Latin alphabet, but “fūl mudammas” is one option. For short, it’s just called “fūl”, which is pronounced like the English word “fool”, and it’s about the beans.
From chana masala with poori to frijoles refritos to beans on toast, lots of cultures have some version of this breakfast food, and all can be great (yes, even the beans on toast). But today we’re about this particular kind of morning protein, fiber, fats, and healthful spices.
You will need
- 2x 14 oz cans fava beans (other kinds of beans work as substitute; kidney beans are common substitution, but this writer prefers black beans personally if she doesn’t have fava in), drained
- 4 garlic cloves, crushed
- 1 tbsp extra virgin olive oil
- 1 teaspoon cinnamon (or ½ cinnamon stick)
- 1 tsp cumin seeds
- 1 tsp chili flakes
- 1 tsp paprika
- 1 tsp black pepper
- Juice of ½ lemon
- For the relish: 1 medium tomato, finely chopped; 1 tbsp extra virgin olive oil; 2 tbsp parsley, finely chopped
- To serve: 4 pitta breads, 2 eggs (omit if vegan), and a selection of pickled vegetables, drained
Method
(we suggest you read everything at least once before doing anything)
1) Add the olive oil to a saucepan over a medium heat; add the garlic, cumin seeds, and cinnamon. Keep these moving for a minute or two before moving to the next step.
2) Add the fava beans, as well as the other seasonings (chili flakes, paprika, black pepper), and mix thoroughly
3) Add 1 cup boiling water, and keep everything on a simmer for about 20 minutes, stirring often. Add the lemon juice while it’s simmering; when the beans start to break down and the mixture starts to thicken, it’s ready.
4) Mix the relish ingredients (finely chopped tomato, olive oil, parsley) thoroughly in a small bowl
5) Toast the pitta breads, and if using, soft-boil the eggs.
6) Serve! We suggest: fūl in a bowl, with one half of a soft-boiled egg per bowl, topped with the relish, and served with the pitta bread and pickled vegetables on the side.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Level-Up Your Fiber Intake! (Without Difficulty Or Discomfort)
- Making Friends With Your Gut (You Can Thank Us Later)
- Less Obvious Probiotic Benefits ← the pickled vegetables contain the probiotics here, while the beans are a great source of prebiotic fiber; this is why they work so well together
- Our Top 5 Spices: How Much Is Enough For Benefits?
- A Tale Of Two Cinnamons
- Eggs: All Things In Moderation?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: