Can Medical Schools Funnel More Doctors Into the Primary Care Pipeline?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Throughout her childhood, Julia Lo Cascio dreamed of becoming a pediatrician. So, when applying to medical school, she was thrilled to discover a new, small school founded specifically to train primary care doctors: NYU Grossman Long Island School of Medicine.
Now in her final year at the Mineola, New York, school, Lo Cascio remains committed to primary care pediatrics. But many young doctors choose otherwise as they leave medical school for their residencies. In 2024, 252 of the nation’s 3,139 pediatric residency slots went unfilled and family medicine programs faced 636 vacant residencies out of 5,231 as students chased higher-paying specialties.
Lo Cascio, 24, said her three-year accelerated program nurtured her goal of becoming a pediatrician. Could other medical schools do more to promote primary care? The question could not be more urgent. The Association of American Medical Colleges projects a shortage of 20,200 to 40,400 primary care doctors by 2036. This means many Americans will lose out on the benefits of primary care, which research shows improves health, leading to fewer hospital visits and less chronic illness.
Many medical students start out expressing interest in primary care. Then they end up at schools based in academic medical centers, where students become enthralled by complex cases in hospitals, while witnessing little primary care.
The driving force is often money, said Andrew Bazemore, a physician and a senior vice president at the American Board of Family Medicine. “Subspecialties tend to generate a lot of wealth, not only for the individual specialists, but for the whole system in the hospital,” he said.
A department’s cache of federal and pharmaceutical-company grants often determines its size and prestige, he said. And at least 12 medical schools, including Harvard, Yale, and Johns Hopkins, don’t even have full-fledged family medicine departments. Students at these schools can study internal medicine, but many of those graduates end up choosing subspecialties like gastroenterology or cardiology.
One potential solution: eliminate tuition, in the hope that debt-free students will base their career choice on passion rather than paycheck. In 2024, two elite medical schools — the Albert Einstein College of Medicine and the Johns Hopkins University School of Medicine — announced that charitable donations are enabling them to waive tuition, joining a handful of other tuition-free schools.
But the contrast between the school Lo Cascio attends and the institution that founded it starkly illustrates the limitations of this approach. Neither charges tuition.
In 2024, two-thirds of students graduating from her Long Island school chose residencies in primary care. Lo Cascio said the tuition waiver wasn’t a deciding factor in choosing pediatrics, among the lowest-paid specialties, with an average annual income of $260,000, according to Medscape.
At the sister school, the Manhattan-based NYU Grossman School of Medicine, the majority of its 2024 graduates chose specialties like orthopedics (averaging $558,000 a year) or dermatology ($479,000).
Primary care typically gets little respect. Professors and peers alike admonish students: If you’re so smart, why would you choose primary care? Anand Chukka, 27, said he has heard that refrain regularly throughout his years as a student at Harvard Medical School. Even his parents, both PhD scientists, wondered if he was wasting his education by pursuing primary care.
Seemingly minor issues can influence students’ decisions, Chukka said. He recalls envying the students on hospital rotations who routinely were served lunch, while those in primary care settings had to fetch their own.
Despite such headwinds, Chukka, now in his final year, remains enthusiastic about primary care. He has long wanted to care for poor and other underserved people, and a one-year clerkship at a community practice serving low-income patients reinforced that plan.
When students look to the future, especially if they haven’t had such exposure, primary care can seem grim, burdened with time-consuming administrative tasks, such as seeking prior authorizations from insurers and grappling with electronic medical records.
While specialists may also face bureaucracy, primary care practices have it much worse: They have more patients and less money to hire help amid burgeoning paperwork requirements, said Caroline Richardson, chair of family medicine at Brown University’s Warren Alpert Medical School.
“It’s not the medical schools that are the problem; it’s the job,” Richardson said. “The job is too toxic.”
Kevin Grumbach, a professor of family and community medicine at the University of California-San Francisco, spent decades trying to boost the share of students choosing primary care, only to conclude: “There’s really very little that we can do in medical school to change people’s career trajectories.”
Instead, he said, the U.S. health care system must address the low pay and lack of support.
And yet, some schools find a way to produce significant proportions of primary care doctors — through recruitment and programs that provide positive experiences and mentors.
U.S. News & World Report recently ranked 168 medical schools by the percentage of graduates who were practicing primary care six to eight years after graduation.
The top 10 schools are all osteopathic medical schools, with 41% to 47% of their students still practicing primary care. Unlike allopathic medical schools, which award MD degrees, osteopathic schools, which award DO degrees, have a history of focusing on primary care and are graduating a growing share of the nation’s primary care physicians.
At the bottom of the U.S. News list is Yale, with 10.7% of its graduates finding lasting careers in primary care. Other elite schools have similar rates: Johns Hopkins, 13.1%; Harvard, 13.7%.
In contrast, public universities that have made it a mission to promote primary care have much higher numbers.
The University of Washington — No. 18 in the ranking, with 36.9% of graduates working in primary care — has a decades-old program placing students in remote parts of Washington, Wyoming, Alaska, Montana, and Idaho. UW recruits students from those areas, and many go back to practice there, with more than 20% of graduates settling in rural communities, according to Joshua Jauregui, assistant dean for clinical curriculum.
Likewise, the University of California-Davis (No. 22, with 36.3% of graduates in primary care) increased the percentage of students choosing family medicine from 12% in 2009 to 18% in 2023, even as it ranks high in specialty training. Programs such as an accelerated three-year primary care “pathway,” which enrolls primarily first-generation college students, help sustain interest in non-specialty medical fields.
The effort starts with recruitment, looking beyond test scores to the life experiences that forge the compassionate, humanistic doctors most needed in primary care, said Mark Henderson, associate dean for admissions and outreach. Most of the students have families who struggle to get primary care, he said. “So they care a lot about it, and it’s not just an intellectual, abstract sense.”
Establishing schools dedicated to primary care, like the one on Long Island, is not a solution in the eyes of some advocates, who consider primary care the backbone of medicine and not a separate discipline. Toyese Oyeyemi Jr., executive director of the Social Mission Alliance at the Fitzhugh Mullan Institute of Health Workforce Equity, worries that establishing such schools might let others “off the hook.”
Still, attending a medical school created to produce primary care doctors worked out well for Lo Cascio. Although she underwent the usual specialty rotations, her passion for pediatrics never flagged — owing to her 23 classmates, two mentors, and her first-year clerkship shadowing a community pediatrician. Now, she’s applying for pediatric residencies.
Lo Cascio also has deep personal reasons: Throughout her experience with a congenital heart condition, her pediatrician was a “guiding light.”
“No matter what else has happened in school, in life, in the world, and medically, your pediatrician is the person that you can come back to,” she said. “What a beautiful opportunity it would be to be that for someone else.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
This article first appeared on KFF Health News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Try This At Home: ABI Test For Clogged Arteries
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Arterial plaque is a big deal, and statistically it’s more of a risk as we get older, often coming to a head around age 72 for women and 65 for men—these are the median ages at which people who are going to get heart attacks, get them. Or get it, because sometimes one is all it takes.
The Ankle-Brachial Index Test
Dr. Brewer recommends a home test for detecting arterial plaque called the Ankle-Brachial Index (ABI), which uses a blood pressure monitor. The test involves measuring blood pressure in both the arms and ankles, then calculating the ratio of these measurements:
- A healthy ABI score is between 1.0 and 1.4; anything outside this range may indicate arterial problems.
- Low ABI scores (below 0.8) suggest plaque is likely obstructing blood flow
- High ABI scores (above 1.4) may indicate artery hardening
Peripheral Artery Disease (PAD), associated with poor ABI results (be they high or low), can cause a whole lot of problems that are definitely better tackled sooner rather than later—remember that atherosclerosis is a self-worsening thing once it gets going, because narrower walls means it’s even easier for more stuff to get stuck in there (and thus, the new stuff that got stuck also becomes part of the walls, and the problem gets worse).
If you need a blood pressure monitor, by the way, here’s an example product on Amazon.
Do note also that yes, if you have plaque obstructing blood flow and hardened arteries, your scores may cancel out and give you a “healthy” score, despite your arteries being very much not healthy. For this reason, this test can be used to raise the alarm, but not to give the “all clear”.
For more on all of the above, plus a demonstration and more in-depth explanation of the test, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Share This Post
-
One More Reason To Prioritize Sleep To Fight Cognitive Decline
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve talked sometimes at 10almonds about how important sleep is for many aspects of health, including for brain health, and including in later life.
There’s a common myth that older people require less sleep; the reality is that sleeping less and not dying of it does not equate to needing less.
See also: Sleep: Yes, You Really Do Still Need It!
And: How Sleep-Deprived Are You, Really?
Quantity is not everything though; quality absolutely matters too. We’ve written about that here:
The 6 Dimensions Of Sleep (And Why They Matter) ← duration is just one dimension out of the six
We’ve even gone into some more obscure, but still very important things, such as: How Your Sleep Position Changes Dementia Risk
We’ve also talked about the role of sleep in memory (and forgetting): How Your Brain Chooses What To Remember
With that in mind…
Some more recent science
This study was about spatial memory, but what’s important (in our opinion) is that it’s about solidifying recent learning.
Researchers measured brain activity in rats for up to 20 hours of sleep following spatial learning tasks. Initially, the neuronal patterns observed during sleep mirrored those from the learning phase. However, as sleep progressed, these patterns transformed to resemble the activity seen when the rats later recalled the locations of food rewards. Interestingly, this reorganization happened during non-REM sleep, which means it wasn’t just a case of “the rats were dreaming about their day” (which is a well-established way in which memories do get encoded), but rather, the newly-learned experiences were being actively encoded in the rest of sleep.
This is critical, because in age-related cognitive decline, it’s very common for very long-term memory (VLTM) to remain intact, while LTM and short-term memory (STM) crumble. For example, someone may remember many details of their life from 20 years ago, but forget where they currently live, or what happened in the conversation two minutes ago.
In other words, the biggest problem is not the storage of memories, but rather the encoding of them in the first place.
Which sleep facilitates!
And it’s also important to note that part about it being the rest of sleep, because when the brain is sleep-deprived, it’ll tend to prioritize REM sleep, which is important, but that means cutting back on other phases of sleep, and from this study, we can see that memory & learning will be amongst the things adversely affected by such cuts.
Here’s the paper, for those interested:
Sleep stages antagonistically modulate reactivation drift
And for those who prefer lighter reading, here’s a pop-science article about the same study, which explains it in more words than we can here:
But wait, there’s more!
Sleep resets neurons for new memories the next day, study finds
So, once again… It is absolutely critical to prioritize good sleep.
Want to know more?
Check out:
Calculate (And Enjoy) The Perfect Night’s Sleep
Take care!
Share This Post
-
Coach’s Plan – by Mike Kavanagh
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A sports coach’s job is to prepare a plan, give it to the player(s), and hold them accountable to it. Change the strategy if needs be, call the shots. The job of the player(s) is then to follow those instructions.
If you have trouble keeping yourself accountable, Kavanagh argues that it can be good to separate how you approach things.
Not just “coach yourself”, but put yourself entirely in the coach’s shoes, as though you were a separate person, then switch back, and follow those instructions, trusting in your coach’s guidance.
The book also provides illustrative examples and guides the reader through some potential pitfalls—for example, what happens when morning you doesn’t want to do the things that evening you decided would be best?
The absolute backbone of this method is that it takes away the paralysing self-doubt that can occur when we second-guess ourselves mid-task.
In short, this book will fire up your enthusiasm and give you a reliable fall-back for when your motivation’s flagging.
Share This Post
Related Posts
-
Boundary-Setting Beyond “No”
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
More Than A “No”
A lot of people struggle with boundary-setting, and it’s not always the way you might think.
The person who “can’t say no” to people probably comes to mind, but the problem is more far-reaching than that, and it’s rooted in not being clear over what a boundary actually is.
For example: “Don’t bring him here again!”
Pretty clear, right?
And while it is indeed clear, it’s not a boundary; it’s a command. Which may or may not be obeyed, and at the end of the day, what right have we to command people in general?
Same goes for less dramatic things like “Don’t talk to me about xyz”, which can still be important or trivial, depending on whether the topic of xyz is deeply traumatizing for you, or mildly annoying, or something else entirely.
Why this becomes a problem
It becomes a problem not because of any lack of clarity about your wishes, but rather, because it opens the floor for a debate. The listener may be given to wonder whether your right to not experience xyz is greater or lesser than their right to do/say/etc xyz.
“My right to swing my fist ends where someone else’s nose begins”
…does not help here, firstly because both sides will believe themself (or nobody) to be the injured party; for the fist-swinger, the other person’s nose made a vicious assault on their freedom. Or secondly, maybe there was some higher principle at stake; a reason why violence was justified. And then ten levels of philosophical debate. We see this a lot when it comes to freedom of expression, and vigorous debate over whether this entails freedom from social consequences of one’s words/actions.
How a good boundary-setting works (if this, then that)
Consider two signs:
- No trespassing!
- Trespassers will be shot!
Superficially, the second just seems like a more violent rendition of the first. But in fact, the second is more informationally useful: it explains what will happen if the boundary is not respected, and allows the reader to make their own informed decision with regard to what to do with that information.
We can employ this method (and can even do so gently, if we so wish and hopefully we mostly do wish to be gentle) when it comes to social and interpersonal boundary-setting:
- If you bring him here again, I will refuse you entrance
- If you bring up that topic again, I will ask you to leave
- If you do that, I will never speak to you again
- If you don’t stop drinking, I will divorce you
This “if-this-then-that” model does the very first thing that any good boundary does: make itself clear.
It doesn’t rely on moral arguments; it doesn’t invite debate. For example in that last case, it doesn’t argue that the partner doesn’t have the right to drink—it simply expresses what the speaker will exercise their own right to do, in that eventuality.
(as an aside, the situation that occurs when one is enmeshed with someone who is dependent on a substance is a complex topic, and if you’re interested in that, check out: Codependency Isn’t What Most People Think)
Back on track: boundary-setting is not about what’s right or good—it’s about nothing more nor less than a clear delineation between what we will and won’t accept, and how we’ll enforce that.
We can also, in particularly personal boundary-setting (such as with sexual boundaries’ oft-claimed “gray areas”), fix an improperly-set boundary that forgot to do the above, e.g:
“How about [proposition]?”
“No thank you” ← casually worded answer; contextually reasonable, and yet not a clear boundary per what we discussed above
“Come on, I think you’d like it”
“I said no. No means no. Ask me again and I will [consequences that are appropriate and actionable]”What’s “appropriate and actionable” may vary a lot from one situation to another, but it’s important that it’s something you can do and are prepared to do and will do if the condition for doing it is met.
Anything less than that is not a boundary—it’s just a request.
Note: this does not require that we have power, by the way. If we have zero power in a situation, well, that definitely sucks, but even then we can still express what is actionable, e.g. “I will never trust you again”.
“Price of entry”
You may have wondered, upon reading “boundary-setting is not about what’s right or good—it’s about nothing more nor less than a clear delineation between what we will and won’t accept, and how we’ll enforce that”, can’t that be used to control and manipulate people, essentially coercing them to do or not do things with the threat of consequences (specifically: bad ones)?
And the answer is: yes, yes it can.
But that’s where the flipside comes into play—the other person gets to set their boundaries, too.
For all of us, if we have any boundaries at all, there is a “price of entry” and all who want to be in our lives, or be close to us, have to decide for themselves whether that price of entry is worth it.
- If a person says “do not talk about topic xyz to me or I will leave”, that is a price of entry for being close to them.
- If you are passionate about talking about topic xyz to the point that you are unwilling to shelve it when in their presence, then that is the price of entry for being close to you.
- If one or more of you is not willing to pay the price of entry, then guess what, you’re just not going to be close.
In cases of forced proximity (e.g. workplaces or families) this is likely to get resolved by the workplace’s own rules (i.e. the price of entry that you agreed to when signing a contract to work there), and if something like that doesn’t exist (such as in families), well, that forced proximity is going to reach a breaking point, and somebody may discover it wasn’t enforceable after all.
See also: Family Estrangement: More Common Than Most People Think
…which also details how to fix it, where possible.
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Spice Of Life
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Great newsletter. Am taking turmeric for inflammation of hips and feet. Works like magic. Would like to know how it works, and what tumeric is best combined with – also whether there any risks in longterm use.❞
Glad you’re enjoying! As for turmeric, it sure is great, isn’t it? To answer your questions in a brief fashion:
- How it works: it does a lot of things, but perhaps its most key feature is its autoxidative metabolites that mediate its anti-inflammatory effect. Thus, it slows or inhibits oxidative stress that would otherwise cause inflammation, increase cancer risk, and advance aging.
- Best combined with: black pepper
- Any risks in long-term use: there are no known risks in long-term use ← that’s just one study, but there are lots. Some studies were prompted by reported hepatotoxicity of curcumin supplements, but a) the reports themselves seem to be without evidence b) the reported hepatoxicity was in relation to contaminants in the supplements, not the curcumin itself c) clinical trials were unable to find any hepatotoxicity (or other) risks anyway. Here’s an example of such a study.
You might also like our previous main feature: Why Curcumin (Turmeric) Is Worth Its Weight In Gold
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’ve recovered from a cold but I still have a hoarse voice. What should I do?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cold, flu, COVID and RSV have been circulating across Australia this winter. Many of us have caught and recovered from one of these common upper respiratory tract infections.
But for some people their impact is ongoing. Even if your throat isn’t sore anymore, your voice may still be hoarse or croaky.
So what happens to the voice when we get a virus? And what happens after?
Here’s what you should know if your voice is still hoarse for days – or even weeks – after your other symptoms have resolved.
Why does my voice get croaky during a cold?
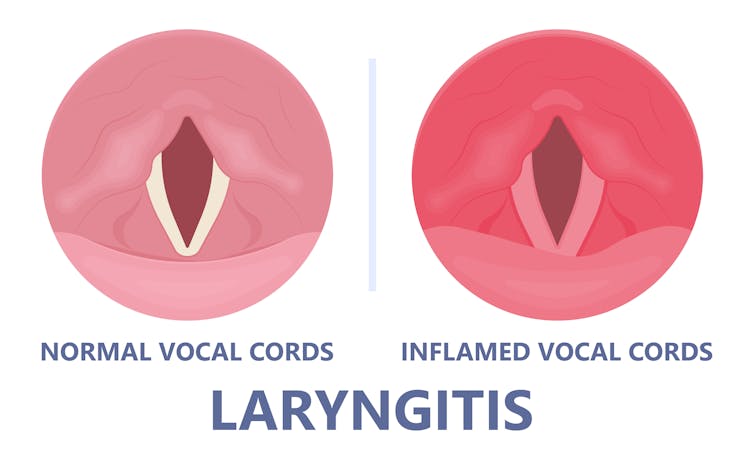
A healthy voice is normally clear and strong. It’s powered by the lungs, which push air past the vocal cords to make them vibrate. These vibrations are amplified in the throat and mouth, creating the voice we hear.
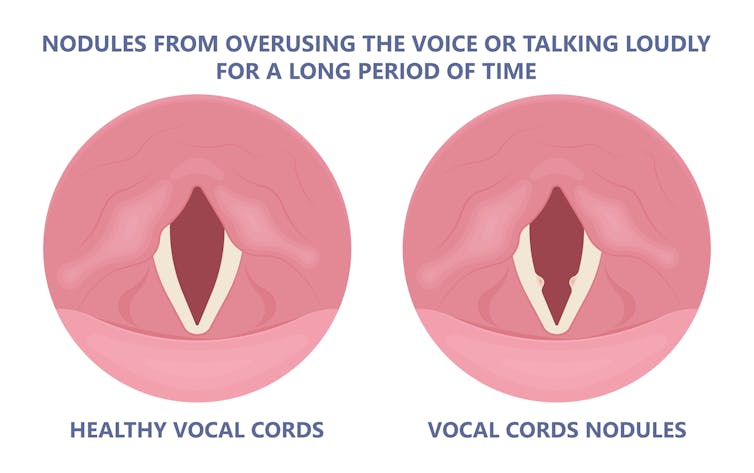
The vocal cords are two elastic muscles situated in your throat, around the level of your laryngeal prominence, or Adam’s apple. (Although everyone has one, it tends to be more pronounced in males.) The vocal cords are small and delicate – around the size of your fingernail. Any small change in their structure will affect how the voice sounds.
When the vocal cords become inflamed – known as laryngitis – your voice will sound different. Laryngitis is a common part of upper respiratory tract infections, but can also be caused through misuse.
Viruses such as the common cold can inflame the vocal cords. Pepermpron/Shutterstock Catching a virus triggers the body’s defence mechanisms. White blood cells are recruited to kill the virus and heal the tissues in the vocal cords. They become inflamed, but also stiffer. It’s harder for them to vibrate, so the voice comes out hoarse and croaky.
In some instances, you may find it hard to speak in a loud voice or have a reduced pitch range, meaning you can’t go as high or loud as normal. You may even “lose” your voice altogether.
Coughing can also make things worse. It is the body’s way of trying to clear the airways of irritation, including your own mucus dripping onto your throat (post-nasal drip). But coughing slams the vocal cords together with force.
Chronic coughing can lead to persistent inflammation and even thicken the vocal cords. This thickening is the body trying to protect itself, similar to developing a callus when a pair of new shoes rubs.
Thickening on your vocal cords can lead to physical changes in the vocal cords – such as developing a growth or “nodule” – and further deterioration of your voice quality.
Coughing and exertion can cause inflamed vocal cords to thicken and develop nodules. Pepermpron/Shutterstock How can you care for your voice during infection?
People who use their voices a lot professionally – such as teachers, call centre workers and singers – are often desperate to resume their vocal activities. They are more at risk of forcing their voice before it’s ready.
The good news is most viral infections resolve themselves. Your voice is usually restored within five to ten days of recovering from a cold.
Occasionally, your pharmacist or doctor may prescribe cough suppressants to limit additional damage to the vocal cords (among other reasons) or mucolytics, which break down mucus. But the most effective treatments for viral upper respiratory tract infections are hydration and rest.
Drink plenty of water, avoid alcohol and exposure to cigarette smoke. Inhaling steam by making yourself a cup of hot water will also help clear blocked noses and hydrate your vocal cords.
Rest your voice by talking as little as possible. If you do need to talk, don’t whisper – this strains the muscles.
Instead, consider using “confidential voice”. This is a soft voice – not a whisper – that gently vibrates your vocal cords but puts less strain on your voice than normal speech. Think of the voice you use when communicating with someone close by.
During the first five to ten days of your infection, it is important not to push through. Exerting the voice by talking a lot or loudly will only exacerbate the situation. Once you’ve recovered from your cold, you can speak as you would normally.
What should you do if your voice is still hoarse after recovery?
If your voice hasn’t returned to normal after two to three weeks, you should seek medical attention from your doctor, who may refer you to an ear nose and throat specialist.
If you’ve developed a nodule, the specialist would likely refer you to a speech pathologist who will show you how to take care of your voice. Many nodules can be treated with voice therapy and don’t require surgery.
You may have also developed a habit of straining your vocal cords, if you forced yourself to speak or sing while they were inflamed. This can be a reason why some people continue to have a hoarse voice even when they’ve recovered from the cold.
In those cases, a speech pathologist may play a valuable role. They may teach you to exercises that make voicing more efficient. For example, lip trills (blowing raspberries) are a fun and easy way you can learn to relax the voice. This can help break the habit of straining your voice you may have developed during infection.
Yeptain Leung, Postdoctoral Research and Lecturer of Speech Pathology, School of Health Sciences, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: