Plant-Based Healthy Cream Cheese
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Cream cheese is a delicious food, and having a plant-based diet isn’t a reason to miss out. Here we have a protein-forward nuts-based cream cheese that we’re sure you’ll love (unless you’re allergic to nuts, in which case, maybe skip this one).
You will need
- 1½ cups raw cashews, soaked in warm water and then drained
- ½ cup water
- ½ cup coconut cream
- Juice of ½ lemon
- 3 tbsp nutritional yeast
- ½ tsp onion powder
- ½ tsp garlic powder
- ½ tsp black pepper
- ½ tsp cayenne pepper
- ¼ tsp MSG, or ½ tsp low-sodium salt
- Optional: ⅓ cup fresh basil
Method
(we suggest you read everything at least once before doing anything)
1) Blend all of the ingredients until creamy.
2) Optional: leave on the countertop, covered, for 1–2 hours, if you want a more fermented (effectively: cheesy) taste.
3) Refrigerate, ideally overnight, before serving. Serving on bagels is a classic, but you can also enjoy with the Healthy Homemade Flatbreads we made yesterday

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Pistachios vs Cashews – Which is Healthier? ← Pistachios actually won here, but cashews are also great and are better (from a culinary perspective) for making cream cheese
- Why You Should Diversify Your Nuts!
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Fat’s Real Barriers To Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Fat Justice In Healthcare
This is Aubrey Gordon, an author, podcaster, and fat justice activist. What does that mean?
When it comes to healthcare, we previously covered some ideas very similar to her work, such as how…
There’s a lot of discrimination in healthcare settings
In this case, it often happens that a thin person goes in with a medical problem and gets treated for that, while a fat person can go in with the same medical problem and be told “you should try losing some weight”.
Top tip if this happens to you… Ask: “what would you advise/prescribe to a thin person with my same symptoms?”
Other things may be more systemic, for example:
When a thin person goes to get their blood pressure taken, and that goes smoothly, while a fat person goes to get their blood pressure taken, and there’s not a blood pressure cuff to fit them, is the problem the size of the person or the size of the cuff? It all depends on perspective, in a world built around thin people.
That’s a trivial-seeming example, but the same principle has far-reaching (and harmful) implications in healthcare in general, e.g:
- Surgeons being untrained (and/or unwilling) to operate on fat people
- Getting a one-size-fits-all dose that was calculated using average weight, and now doesn’t work
- MRI machines are famously claustrophobia-inducing for thin people; now try not fitting in it in the first place
…and so forth. So oftentimes, obesity will be correlated with a poor healthcare outcome, where the problem is not actually the obesity itself, but rather the system having been set up with thin people in mind.
It would be like saying “Having O- blood type results in higher risks when receiving blood transfusions”, while omitting to add “…because we didn’t stock O- blood”.
Read more on this topic: Shedding Some Obesity Myths
Does she have practical advice about this?
If she could have you understand one thing, it would be:
You deserve better.
Or if you are not fat: your fat friends deserve better.
How this becomes useful is: do not accept being treated as the problem!
Demand better!
If you meekly accept that you “just need to lose weight” and that thus you are the problem, you take away any responsibility from your healthcare provider(s) to actually do their jobs and provide healthcare.
See also Gordon’s book, which we’ve not reviewed yet but probably will one of these days:
“You Just Need to Lose Weight”: And 19 Other Myths About Fat People – by Aubrey Gordon
Are you saying fat people don’t need to lose weight?
That’s a little like asking “would you say office workers don’t need to exercise more?”; there are implicit assumptions built into the question that are going unaddressed.
Rather: some people might benefit healthwise from losing weight, some might not.
In fact, over the age of 65, being what is nominally considered “overweight” reduces all-cause mortality risk.
For details of that and more, see: When BMI Doesn’t Measure Up
But what if I do want/need to lose weight?
Gordon’s not interested in helping with that, but we at 10almonds are, so…
Check out: Lose Weight, But Healthily
Where can I find more from Aubrey Gordon?
You might enjoy her blog:
Aubrey Gordon | Your Fat Friend
Or her other book, which we reviewed previously:
What We Don’t Talk About When We Talk About Fat – by Aubrey Gordon
Enjoy!
Share This Post
-
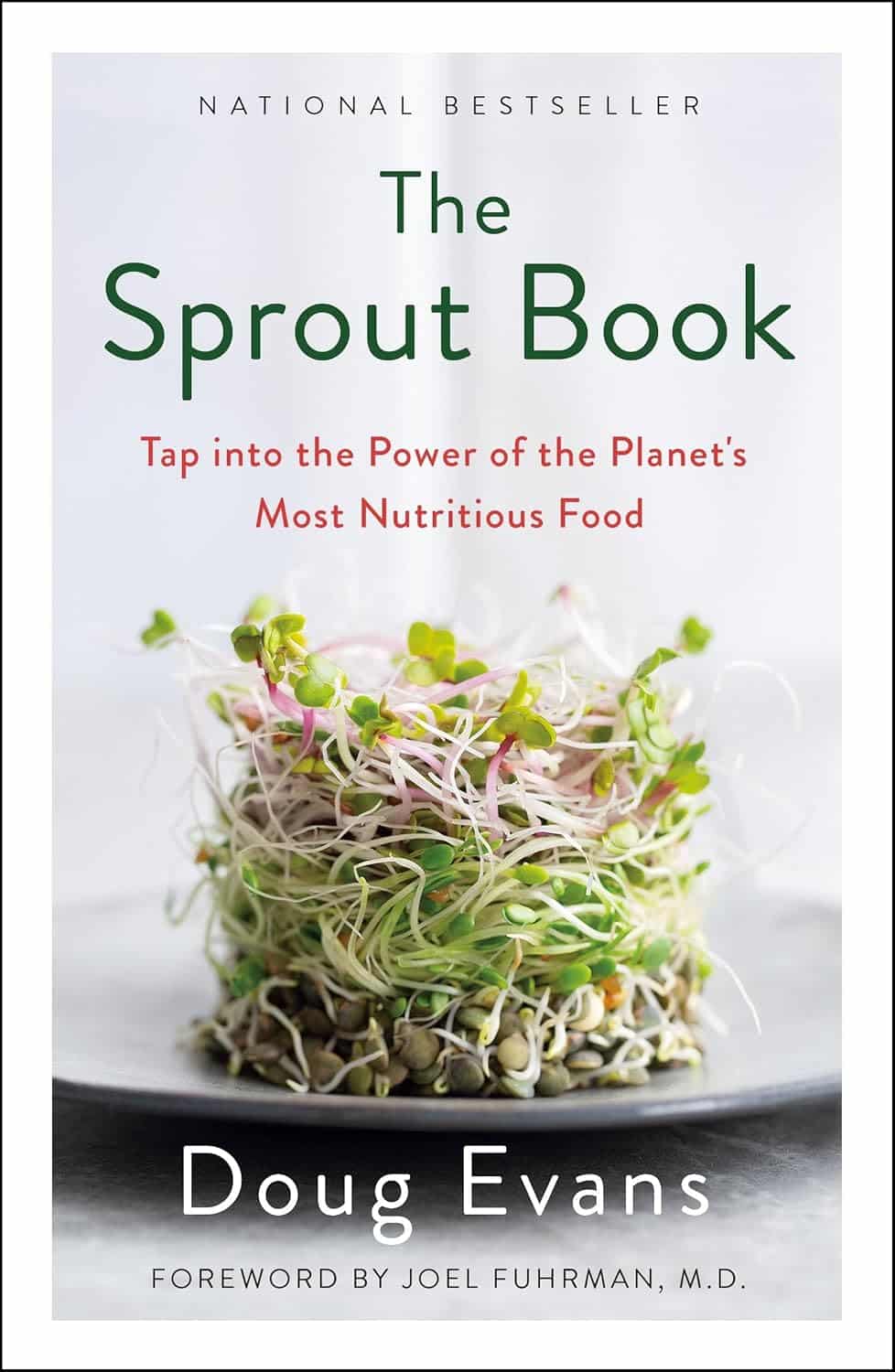
The Sprout Book – by Doug Evans
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Sprouting seeds are more nutritious than most people think, and “seeds” is also a much broader category than people think. Beyond even chia and sunflower and such, this book bids us remember that onions do not just appear on supermarket shelves fully formed (to give just one example of many); most plants come from seeds and of those, most can be usefully sprouted.
The author, most well-known for his tech companies, here is selling us a very low-tech health kick with very little profit to be found except for our health. By sprouting seeds of many kinds at home, we can enjoy powerful superfoods that are not only better than, but also cheaper than, most supplements.
Nor are the benefits of sprouting things marginal; we’re not talking about a 1–10% increase in bioavailable so much as what’s often a 100–1000% increase.
After explaining the science and giving a primer on sprouting things for oneself, there is a wide selection of recipes, but the biggest benefit of the book is in just getting the reader up-and-running with at-home sprouting.
Bottom line: if you like the idea of letting food be your medicine and even like the idea of essentially growing your own food with zero gardening skills, then this is an excellent book for you.
Share This Post
-
Test For Whether You Will Be Able To Achieve The Splits
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Some people stretch for years without being able to do the splits; others do it easily after a short while. Are there people for whom it is impossible, and is there a way to know in advance whether our efforts will be fruitful? Liv (of “LivInLeggings” fame) has the answer:
One side of the story
There are several factors that affect whether we can do the splits, including:
- arrangement of the joint itself
- length of tendons and muscles
- “stretchiness” of tendons and muscles
The latter two things, we can readily train to improve. Yes, even the basic length can be changed over time, because the body adapts.
The former thing, however (arrangement of the joint itself) is near-impossible, because skeletal changes happen more slowly than any other changes in the body. In a battle of muscle vs bone, muscle will always win eventually, and even the bone itself can be rebuilt (as the body fixes itself, or in the case of some diseases, messes itself up). However, changing the arrangement of your joint itself is far beyond the auspices of “do some stretches each day”. So, for practical purposes, without making it the single most important thing in your life, it’s impossible.
How do we know if the arrangement of our hip joint will accommodate the splits? We can test it, one side at a time. Liv uses the middle splits, also called the side splits or box splits, as an example, but the same science and the same method goes for the front splits.
Stand next to a stable elevated-to-hip-height surface. You want to be able to raise your near-side leg laterally, and rest it on the surface, such that your raised leg is now perfectly perpendicular to your body.
There’s a catch: not only do you need to still be stood straight while your leg is elevated 90° to the side, but also, your hips still need to remain parallel to the floor—not tilted up to one side.
If you can do this (on both sides, even if not both simultaneously right now), then your hip joint itself definitely has the range of motion to allow you to do the side splits; you just need to work up to it. Technically, you could do it right now: if you can do this on both sides, then since there’s no tendon or similar running between your two legs to make it impossible to do both at once, you could do that. But, without training, your nerves will stop you; it’s an in-built self-defense mechanism that’s just firing unnecessarily in this case, and needs training to get past.
If you can’t do this, then there are two main possibilities:
- Your joint is not arranged in a way that facilitates this range of motion, and you will not achieve this without devoting your life to it and still taking a very long time.
- Your tendons and muscles are simply too tight at the moment to allow you even the half-split, so you are getting a false negative.
This means that, despite the slightly clickbaity title on YouTube, this test cannot actually confirm that you can never do the middle splits; it can only confirm that you can. In other words, this test gives two possible results:
- “Yes, you can do it!”
- “We don’t know whether you can do it”
For more on the anatomy of this plus a visual demonstration of the test, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Stretching Scientifically – by Thomas Kurz ← this is our review of the book she’s working from in this video; this book has this test!
Take care!
Share This Post
Related Posts
-
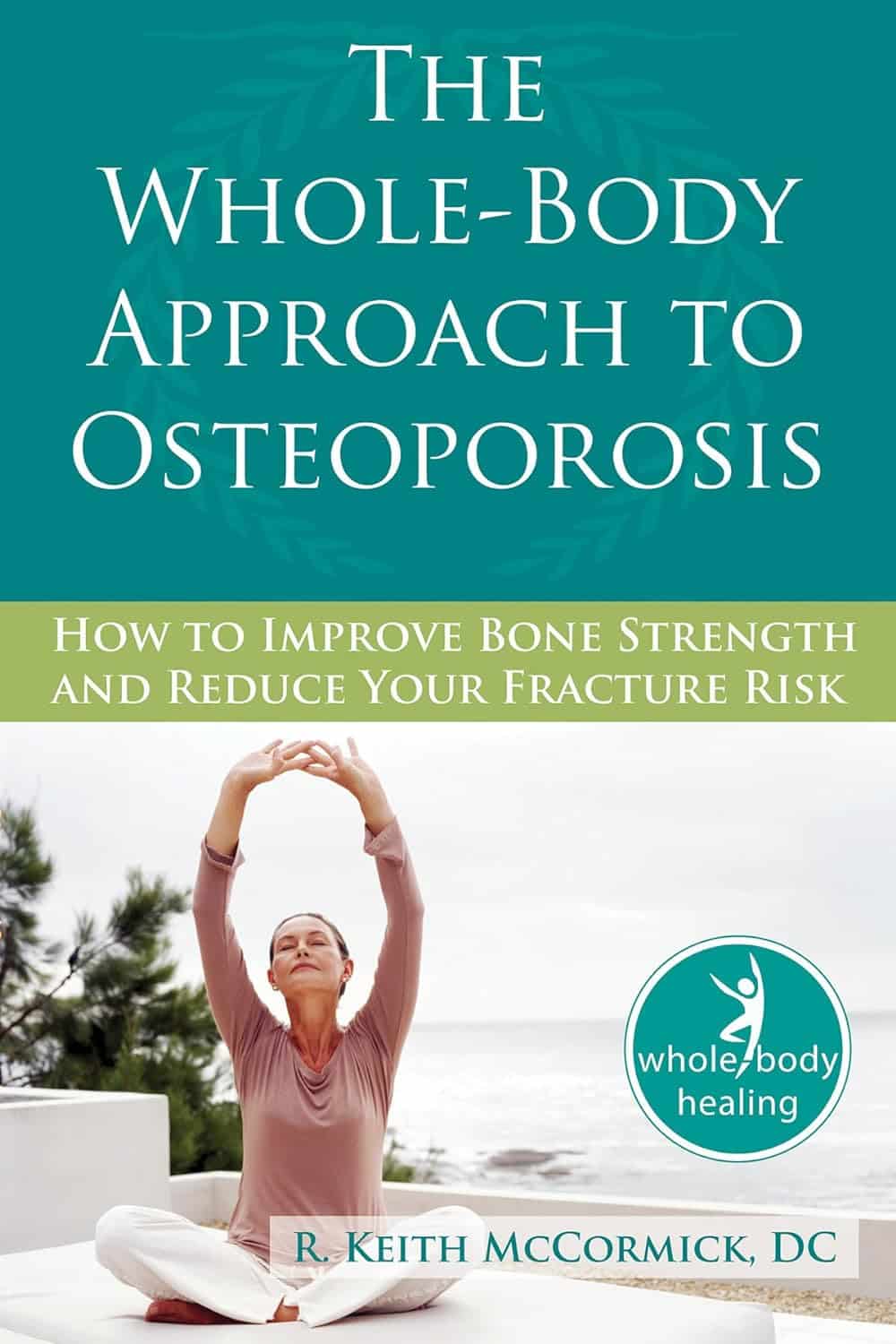
The Whole-Body Approach to Osteoporosis – by Keith McCormick
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
You probably already know to get enough calcium and vitamin D, and do some resistance training. What does this book offer beyond that advice?
It’s pretty comprehensive, as it turns out. It covers the above, plus the wide range of medications available, what supplements help or harm or just don’t have enough evidence either way yet, things like that.
Amongst the most important offerings are the signs and symptoms that can help monitor your bone health (things you can do at home! Like examinations of your fingernails, hair, skin, tongue, and so forth, that will reveal information about your internal biochemical make-up), as well as what lab tests to ask for. Which is important, as osteoporosis is one of those things whereby we often don’t learn something is wrong until it’s too late.
The author is a chiropractor, which doesn’t always have a reputation as the most robustly science-based of physical therapy options, but he…
- doesn’t talk about chiropractic
- did confer with a flock of experts (osteopaths, nutritionists, etc) to inform/check his work
- does refer consistently to good science, and explains it well
- includes 16 pages of academic references, and yes, they are very reputable publications
Bottom line: this one really does give what the subtitle promises: a whole body approach to avoiding (or reversing) osteoporosis.
Click here to check out The Whole Body Approach To Osteoporosis; sooner is better than later!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Zuranolone: What to know about the pill for postpartum depression
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
In the year after giving birth, about one in eight people who give birth in the U.S. experience the debilitating symptoms of postpartum depression (PPD), including lack of energy and feeling sad, anxious, hopeless, and overwhelmed.
Postpartum depression is a serious, potentially life-threatening condition that can affect a person’s bond with their baby. Although it’s frequently confused with the so-called “baby blues,” it’s not the same.
The baby blues include similar, temporary symptoms that affect up to 80 percent of people who have recently given birth and usually go away within the first few weeks. PPD usually begins within the first month after giving birth and can last for months and interfere with a person’s daily life if left untreated. Thankfully, PPD is treatable and there is help available.
On August 4, the FDA approved zuranolone, branded as Zurzuvae, the first-ever oral medication to treat PPD. Until now, besides other common antidepressants, the only medication available to treat PPD specifically was the IV injection brexanolone, which is difficult to access and expensive and can only be administered in a hospital or health care setting.
Read on to find out more about zuranolone: what it is, how it works, how much it costs, and more.
What is zuranolone?
Zurzuvae is the brand name for zuranolone, an oral medication to treat postpartum depression. Developed by Sage Therapeutics in partnership with Biogen, it’s now available in the U.S. Zurzuvae is typically prescribed as two 25 mg capsules a day for 14 days. In clinical trials, the medication showed to be fast-acting, improving PPD symptoms in just three days.
How does zuranolone work?
Zuranolone is a neuroactive steroid, a type of medication that helps the neurotransmitter GABA’s receptors, which affect how the body reacts to anxiety, stress, and fear, function better.
“Zuranolone can be thought of as a synthetic version of [the neuroactive steroid] allopregnanolone,” says Dr. Katrina Furey, a reproductive psychiatrist, clinical instructor at Yale University, and co-host of the Analyze Scripts podcast. “Women with PPD have lower levels of allopregnenolone compared to women without PPD.”
How is it different from other antidepressants?
“What differentiates zuranolone from other previously available oral antidepressants is that it has a much more rapid response and a shorter course of treatment,” says Dr. Asima Ahmad, an OB-GYN, reproductive endocrinologist, and founder of Carrot Fertility.
“It can take effect as early as on day three of treatment, versus other oral antidepressants that can take up to six to 12 weeks to take full effect.”
What are Zurzuvae’s side effects?
According to the FDA, the most common side effects of Zurzuvae include dizziness, drowsiness, diarrhea, fatigue, the common cold, and urinary tract infection. Similar to other antidepressants, the medication may increase the risk of suicidal thoughts and actions in people 24 and younger. However, NPR noted that this type of labeling is required for all antidepressants, and researchers didn’t see any reports of suicidal thoughts in their trials.
“Drug trials also noted that the side effects for zuranolone were not as severe,” says Ahmad. “[There was] no sudden loss of consciousness as seen with brexanolone or weight gain and sexual dysfunction, which can be seen with other oral antidepressants.”
She adds: “Given the lower incidence of side effects and more rapid-acting onset, zuranolone could be a viable option for many,” including those looking for a treatment that offers faster symptom relief.
Can someone breastfeed while taking zuranolone?
It’s complicated. In clinical trials, participants were asked to stop breastfeeding (which, according to Furey, is common in early clinical trials).
A small study of people who were nursing while taking zuranolone found that 0.3 percent of the medication dose was passed on to breast milk, which, Furey says, is a pretty low amount of exposure for the baby. Ahmad says that “though some data suggests that the risk of harm to the baby may be low, there is still overall limited data.”
Overall, people should talk to their health care provider about the risks and benefits of breastfeeding while on the medication.
“A lot of factors will need to be weighed, such as overall health of the infant, age of the infant, etc., when making this decision,” Furey says.
How much does Zurzuvae cost?
Zurzuvae’s price before insurance coverage is $15,900 for the 14-day treatment. However, the Policy Center for Maternal Mental Health says insurance companies and Medicaid are expected to cover it because it’s the only drug of its kind.
Less than 1 percent of U.S. insurers have issued coverage guidelines so far, so it’s still unknown how much it will cost patients after insurance. Some insurers require patients to try another antidepressant first (like the more common SSRIs) before covering Zurzuvae. For uninsured and underinsured people, Sage Therapeutics said it will offer copay assistance.
The hefty price tag and potential issues with coverage may widen existing health disparities, says Ahmad. “We need to ensure that we are seeking out solutions to enable wide-scale access to all PPD treatments so that people have access to whatever treatment may work best for them.”
If you or anyone you know is considering suicide or self-harm or is anxious, depressed, upset, or needs to talk, call the Suicide & Crisis Lifeline at 988 or text the Crisis Text Line at 741-741. For international resources, here is a good place to begin.
For more information, talk to your health care provider.
This article first appeared on Public Good News and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
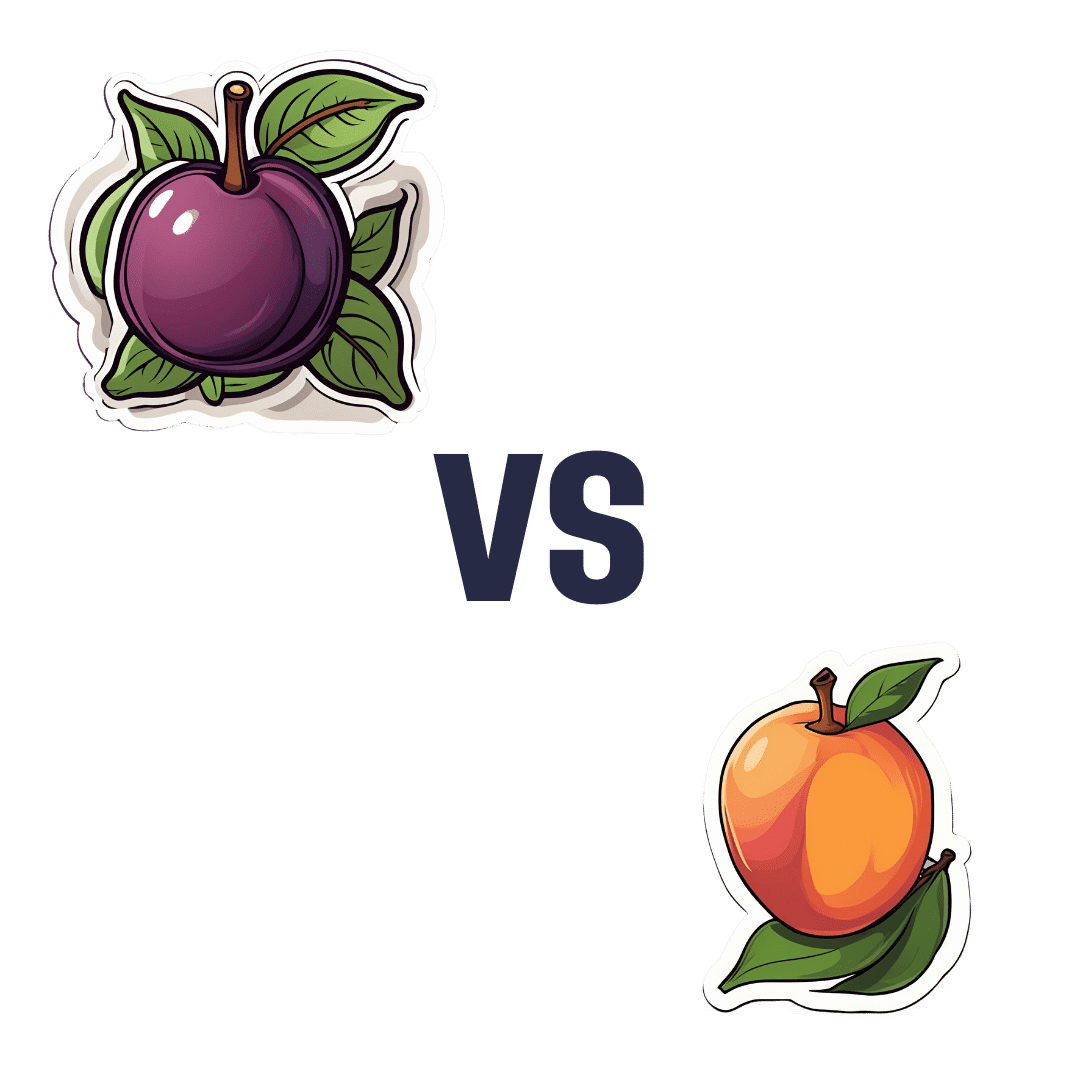
Plum vs Nectarine – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plums to nectarines, we picked the nectarines.
Why?
Both are great! But nectarines win at least marginally in each category we look at.
In terms of macros, plums have more carbs while nectarines have more fiber, resulting of course in a lower glycemic index. Plums do have a low GI also; just, nectarines have it better.
When it comes to vitamins, plums have more of vitamins A, B6, C, and K, while nectarines have more of vitamins B1, B2, B3, B5, E, and choline.
In the category of minerals, plums are great but not higher in any mineral than nectarines; nectarines meanwhile have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc.
All in all, enjoy both. And if having dried fruit, then prunes (dried plums) are generally more widely available than dried nectarines. But if you’re choosing one fruit or the other, nectarine is the way to go.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods
- Top 8 Fruits That Prevent & Kill Cancer
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: