PFAS Exposure & Cancer: The Numbers Are High
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
PFAS & Cancer Risk: The Numbers Are High

This is Dr. Maaike van Gerwen. Is that an MD or a PhD, you wonder? It’s both.
She’s also Director of Research in the Department of Otolaryngology at Mount Sinai Hospital in New York, Scientific Director of the Program of Personalized Management of Thyroid Disease, and Member of the Institute for Translational Epidemiology and the Transdisciplinary Center on Early Environmental Exposures.
What does she want us to know?
She’d love for us to know about her latest research published literally today, about the risks associated with PFAS, such as the kind widely found in non-stick cookware:
Per- and polyfluoroalkyl substances (PFAS) exposure and thyroid cancer risk
Dr. van Gerwen and her team tested this several ways, and the very short and simple version of the findings is that per doubling of exposure, there was a 56% increased rate of thyroid cancer diagnosis.
(The rate of exposure was not just guessed based on self-reports; it was measured directly from PFAS levels in the blood of participants)
- PFAS exposure can come from many sources, not just non-stick cookware, but that’s a “biggie” since it transfers directly into food that we consume.
- Same goes for widely-available microwaveable plastic food containers.
- Relatively less dangerous exposures include waterproofed clothing.
To keep it simple and look at the non-stick pans and microwavable plastic containers, doubling exposure might mean using such things every day vs every second day.
Practical take-away: PFAS may be impossible to avoid completely, but even just cutting down on the use of such products is already reducing your cancer risk.
Isn’t it too late, by this point in life? Aren’t they “forever chemicals”?
They’re not truly “forever”, but they do have long half-lives, yes.
See: Can we take the “forever” out of forever chemicals?
The half-lives of PFOS and PFOA in water are 41 years and 92 years, respectively.
In the body, however, because our body is constantly trying to repair itself and eliminate toxins, it’s more like 3–7 years.
That might seem like a long time, and perhaps it is, but the time will pass anyway, so might as well get started now, rather than in 3–7 years time!
Read more: National Academies Report Calls for Testing People With High Exposure to “Forever Chemicals”
What should we use instead?
In place of non-stick cookware, cast iron is fantastic. It’s not everyone’s preference, though, so you might also like to know that ceramic cookware is a fine option that’s functionally non-stick but without needing a non-stick coating. Check for PFAS-free status; they should advertise this.
In place of plastic microwaveable containers, Pyrex (or equivalent) glass dishes (you can get them with lids) are a top-tier option. Ceramic containers (without metallic bits!) are also safely microwaveable.
See also:
Here’s a List of Products with PFAS (& How to Avoid Them)
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Basic Baked Tofu
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the main criticisms of tofu is that it is tasteless. Well, so is flour, but you’re not supposed to eat it plain, and the same goes for tofu. It’s a blank canvas that you get to decide what to do with—not to mention, it’s a canvas that’s very high in protein, and is a complete protein too, containing all essential amino acids. Anyway, here’s a starter recipe that elevates tofu from “nutrition” to “nutritious tasty snack”!
We were going to do a fancier recipe today, but considered that it might be judicious to cover this basic element first, that can be incorporated into a larger recipe later, a bit like we have done with recipes such as our Tasty Versatile Rice, and Plant-Based Healthy Cream Cheese (amongst others).
You will need
- 1 block of extra-firm tofu; these are quite standardized in size; it should be about 12oz; don’t worry if it’s a little more or less.
- 2 tbsp arrowroot powder (or potato starch if you don’t have arrowroot)
- 1½ tbsp extra virgin olive oil
- 1 tbsp nutritional yeast
- 1 tsp black pepper
- ½ tsp MSG or 1 tsp low-sodium salt
- Optional: ½ tsp garlic powder
- Optional: ½ tsp ground turmeric
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 425ºF / 220ºC.
2) Press the tofu for about 15 minutes (to remove excess moisture), using a tofu press if you have one. If you don’t, then here is an example product on Amazon, or alternatively, you can go with the time-honored tradition of cutting the tofu lengthways into slabs, and wrapping it in a lint-free kitchen towel or muslin cloth, and pressing it with heavy books. We don’t recommend pressing for more than about 15 minutes, as you are going to bake the tofu so you don’t want it too dry going in.
3) Cut the tofu into cubes. Size is up to you, but half-inch cubes are very respectable.
4) Combine the tofu cubes in a big bowl with the oil and seasonings, including the nutritional yeast but not the arrowroot powder or potato starch yet. You will need to toss them gently (very gently; they are fragile!) to combine.
5) Add the arrowroot powder or potato starch, and again toss gently to combine. We do this last, because it would stop the other things from sticking properly if we did it earlier.
6) Arrange the tofu on a baking tray lined with baking paper, in a single layer so that the cubes don’t touch. Bake for 15 minutes, turn them over, and bake for a further 15 minutes on the other side. They should now be golden and crisp, but if they’re not, just give them a little more time.
7) Serve as a snack, or set aside for whatever else you’re going to do with them in a larger more complex recipe.
Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tofu vs Seitan – Which is Healthier?
- Plant vs Animal Protein: Head to Head
- Our Top 5 Spices: How Much Is Enough For Benefits?
Take care!
Share This Post
-
The Doctor Who Wants Us To Exercise Less, & Move More
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Today we’re talking about Dr. Rangan Chatterjee. He’s a medical doctor with decades of experience, and he wants us all to proactively stay in good health, rather than waiting for things to go wrong.
Great! What’s his deal?
Dr. Chatterjee advises that we take care of the following four pillars of good health:
- Relaxation
- Food
- Movement
- Sleep
And, they’re not in this order at random. Usually advice starts with diet and exercise, doesn’t it?
But for Dr. Chatterjee, it’s useless to try to tackle diet first if one is stressed-to-death by other things. As for food next, he knows that a good diet will fuel the next steps nicely. Speaking of next steps, a day full of movement is the ideal setup to a good night’s sleep—ready for a relaxing next day.
Relaxation
Here, Dr. Chatterjee advises that we go with what works for us. It could be meditation or yoga… Or it could be having a nice cup of tea while looking out of the window.
What’s most important, he says, is that we should take at least 15 minutes per day as “me time”, not as a reward for when we’ve done our work/chores/etc, but as something integrated into our routine, preferably early in the day.
Food
There are no grand surprises here: Dr. Chatterjee advocates for a majority plant-based diet, whole foods, and importantly, avoiding sugar.
He’s also an advocate of intermittent fasting, but only so far as is comfortable and practicable. Intermittent fasting can give great benefits, but it’s no good if that comes at a cost of making us stressed and suffering!
Movement
This one’s important. Well, they all are, but this one’s particularly characteristic to Dr. Chatterjee’s approach. He wants us to exercise less, and move more.
The reason for this is that strenuous exercise will tend to speed up our metabolism to the point that we will be prompted to eat high calorie quick-energy foods to compensate, and when we do, our body will rush to store that as fat, understanding (incorrectly) that we are in a time of great stress, because why else would we be exerting ourselves that much?
Instead, he advocates for building as much natural movement into our daily routine as possible. Walking more, taking the stairs, doing the gardening/housework.
That said, he does also advise some strength-training on a daily basis—bodyweight exercises like squats and lunges are top of his list.
Sleep
Here, aside from the usual “sleep hygiene” advices (dark cool room, fresh bedding, etc), he also advises we do as he does, and take an hour before bedtime as a purely wind-down time. In gentle lighting, perhaps reading (not on a bright screen!), for example.
Ready to start the next day, relaxed and ready to go.
If you’d like to know more about Dr. Chatterjee’s approach…
You can check out his:
If you don’t know where to start, we recommend the blog! It has a lot of guests there too, including Wim Hof, Gabor Maté, Mindy Pelz, and come to think of it, a lot of other people we’ve also featured ideas from previously!
Enjoy!
Share This Post
-
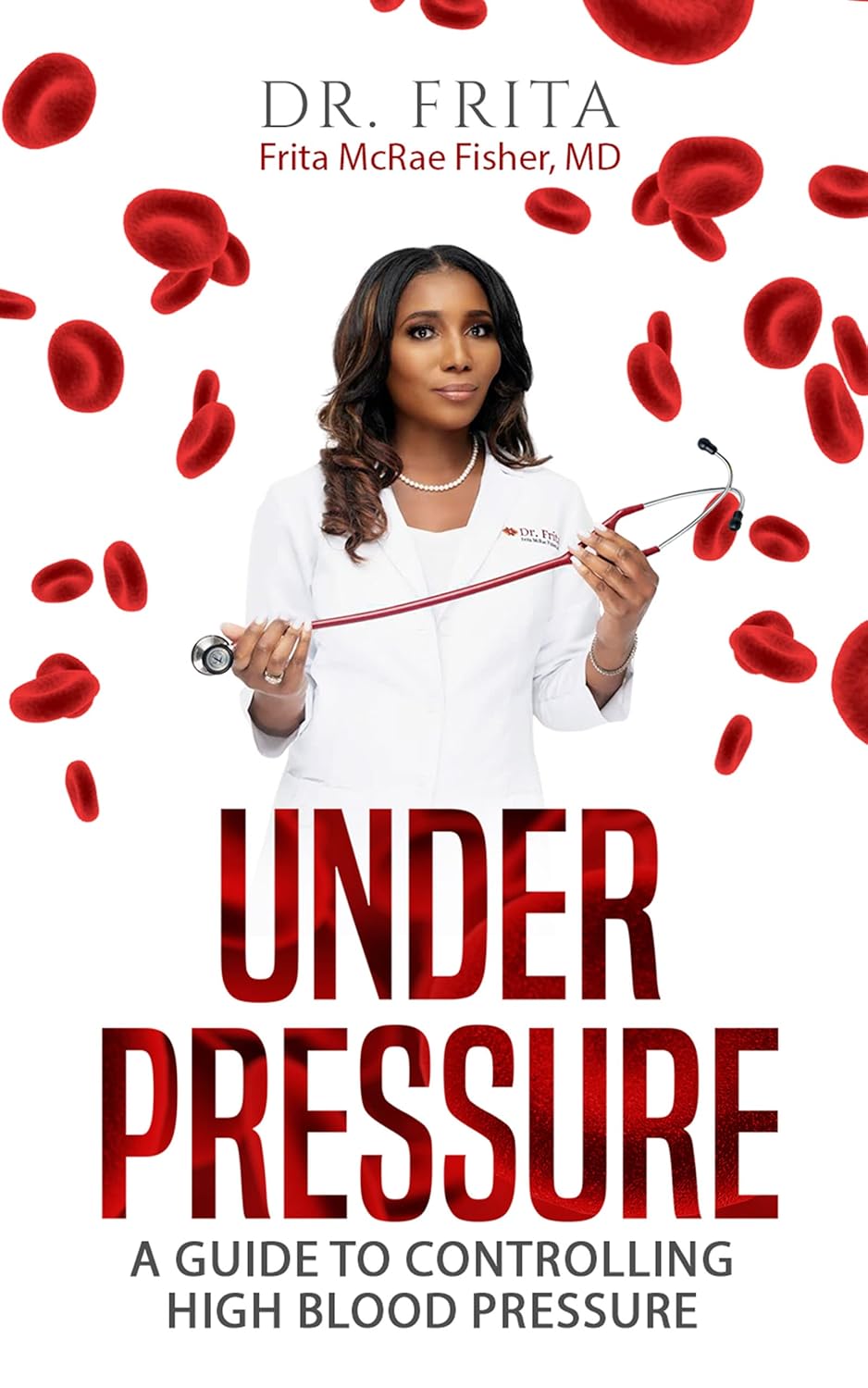
Under Pressure: A Guide To Controlling High Blood Pressure – by Dr. Frita Fisher
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Hypertension kills a lot of people, and does so with little warning—it can be asymptomatic before it gets severe enough to cause harm, and once it causes harm, well, one heart attack or stroke is already one too many.
Aimed more squarely at people in the 35–45 danger zone (young enough to not be getting regular blood pressure checks, old enough that it may have been building up for decades), this is a very good primer on blood pressure, factors affecting it, what goes wrong, what to do about it, and how to make a good strategy for managing it for life.
The style is easy-reading, making this short (91 pages) book a very quick read, but an informative one.
Bottom line: if you are already quite knowledgeable about blood pressure and blood pressure management, this one’s probably not for you. But if you’re in the category of “what do those numbers mean again?”, then this is a very handy book to have, to get you up to speed so that you can handle things as appropriate.
Click here to check out Under Pressure, and get/keep yours under control!
Share This Post
Related Posts
-
Upgrade Your Life – by Pat Divilly
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Pat Divilly takes us through the steps to establish what it is we want out of life, adopt daily habits of success, build our self-esteem and confidence, and pursue what’s actually fulfilling, whatever that is for us as individuals.
The general layout of the book is: first, figuring out where you genuinely want to go (not just where people expect you to want to go!), and then seeing about what things you can change, first small and then larger, to get there.
The scope of the book covers work life and personal life, and treats them both as something where you can optimize how things work for you, and those around you. All in all, unless your life is literally perfect in every way imaginable, there’s probably something in this book that will help you to, indeed, “upgrade your life”. And who wouldn’t want that?
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
I’m feeling run down. Why am I more likely to get sick? And how can I boost my immune system?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It has been a long winter, filled with many viruses and cost-of-living pressures, on top of the usual mix of work, study, life admin and caring responsibilities.
Stress is an inevitable part of life. In short bursts, our stress response has evolved as a survival mechanism to help us be more alert in fight or flight situations.
But when stress is chronic, it weakens the immune system and makes us more vulnerable to illnesses such as the common cold, flu and COVID.
Pexels/Ketut Subiyanto Stress makes it harder to fight off viruses
When the immune system starts to break down, a virus that would normally have been under control starts to flourish.
Once you begin to feel sick, the stress response rises, making it harder for the immune system to fight off the disease. You may be sick more often and for longer periods of time, without enough immune cells primed and ready to fight.
In the 1990s, American psychology professor Sheldon Cohen and his colleagues conducted a number of studies where healthy people were exposed to an upper respiratory infection, through drops of virus placed directly into their nose.
These participants were then quarantined in a hotel and monitored closely to determine who became ill.
One of the most important factors predicting who got sick was prolonged psychological stress.
Cortisol suppresses immunity
“Short-term stress” is stress that lasts for a period of minutes to hours, while “chronic stress” persists for several hours per day for weeks or months.
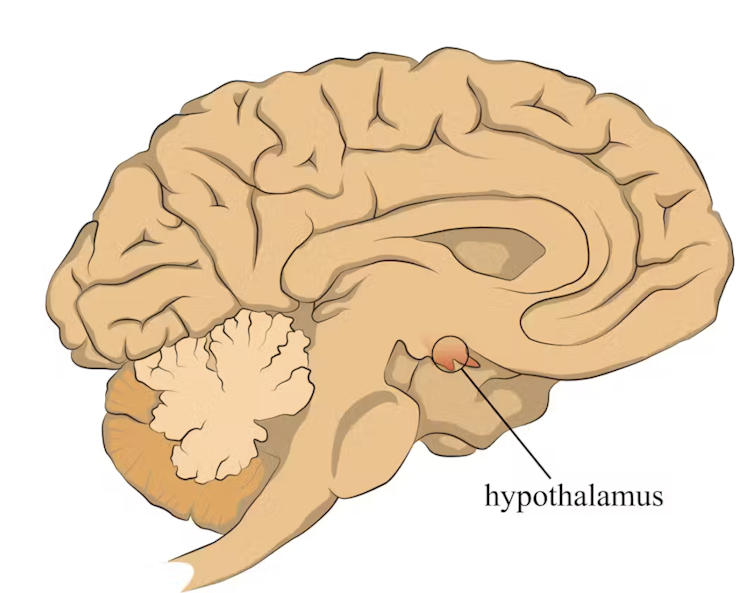
When faced with a perceived threat, psychological or physical, the hypothalamus region of the brain sets off an alarm system. This signals the release of a surge of hormones, including adrenaline and cortisol.
The hypothalamus sets off an alarm system in response to a real or perceived threat. stefan3andrei/Shutterstock In a typical stress response, cortisol levels quickly increase when stress occurs, and then rapidly drop back to normal once the stress has subsided. In the short term, cortisol suppresses inflammation, to ensure the body has enough energy available to respond to an immediate threat.
But in the longer term, chronic stress can be harmful. A Harvard University study from 2022 showed that people suffering from psychological distress in the lead up to their COVID infection had a greater chance of experiencing long COVID. They classified this distress as depression, probable anxiety, perceived stress, worry about COVID and loneliness.
Those suffering distress had close to a 50% greater risk of long COVID compared to other participants. Cortisol has been shown to be high in the most severe cases of COVID.
Stress causes inflammation
Inflammation is a short-term reaction to an injury or infection. It is responsible for trafficking immune cells in your body so the right cells are present in the right locations at the right times and at the right levels.
The immune cells also store a memory of that threat to respond faster and more effectively the next time.
Initially, circulating immune cells detect and flock to the site of infection. Messenger proteins, known as pro-inflammatory cytokines, are released by immune cells, to signal the danger and recruit help, and our immune system responds to neutralise the threat.
During this response to the infection, if the immune system produces too much of these inflammatory chemicals, it can trigger symptoms such as nasal congestion and runny nose.
Our immune response can trigger symptoms such as a runny nose. Alyona Mandrik/Shutterstock What about chronic stress?
Chronic stress causes persistently high cortisol secretion, which remains high even in the absence of an immediate stressor.
The immune system becomes desensitised and unresponsive to this cortisol suppression, increasing low-grade “silent” inflammation and the production of pro-inflammatory cytokines (the messenger proteins).
Immune cells become exhausted and start to malfunction. The body loses the ability to turn down the inflammatory response.
Over time, the immune system changes the way it responds by reprogramming to a “low surveillance mode”. The immune system misses early opportunities to destroy threats, and the process of recovery can take longer.
So how can you manage your stress?
We can actively strengthen our immunity and natural defences by managing our stress levels. Rather than letting stress build up, try to address it early and frequently by:
1) Getting enough sleep
Getting enough sleep reduces cortisol levels and inflammation. During sleep, the immune system releases cytokines, which help fight infections and inflammation.
2) Taking regular exercise
Exercising helps the lymphatic system (which balances bodily fluids as part of the immune system) circulate and allows immune cells to monitor for threats, while sweating flushes toxins. Physical activity also lowers stress hormone levels through the release of positive brain signals.
3) Eating a healthy diet
Ensuring your diet contains enough nutrients – such as the B vitamins, and the full breadth of minerals like magnesium, iron and zinc – during times of stress has a positive impact on overall stress levels. Staying hydrated helps the body to flush out toxins.
4) Socialising and practising meditation or mindfulness
These activities increase endorphins and serotonin, which improve mood and have anti-inflammatory effects. Breathing exercises and meditation stimulate the parasympathetic nervous system, which calms down our stress responses so we can “reset” and reduce cortisol levels.
Sathana Dushyanthen, Academic Specialist & Lecturer in Cancer Sciences & Digital Health| Superstar of STEM| Science Communicator, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Hope: A research-based explainer
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This year, more than 60 countries, representing more than 4 billion people, will hold major elections. News headlines already are reporting that voters are hanging on to hope. When things get tough or don’t go our way, we’re told to hang on to hope. HOPE was the only word printed on President Barack Obama’s iconic campaign poster in 2008.
Research on hope has flourished only in recent decades. There’s now a growing recognition that hope has a role in physical, social, and mental health outcomes, including promoting resilience. As we embark on a challenging year of news, it’s important for journalists to learn about hope.
So what is hope? And what does the research say about it?
Merriam-Webster defines hope as a “desire accompanied by expectation of or belief in fulfillment.” This definition highlights the two basic dimensions of hope: a desire and a belief in the possibility of attaining that desire.
Hope is not Pollyannaish optimism, writes psychologist Everett Worthington in a 2020 article for The Conversation. “Instead, hope is a motivation to persevere toward a goal or end state, even if we’re skeptical that a positive outcome is likely.”
There are several scientific theories about hope.
One of the first, and most well-known, theories on hope was introduced in 1991 by American psychologist Charles R. Snyder.
In a paper published in the Journal of Personality and Social Psychology, Snyder defined hope as a cognitive trait centered on the pursuit of goals and built on two components: a sense of agency in achieving a goal, and a perceived ability to create pathways to achieve that goal. He defined hope as something individualistic.
Snyder also introduced the Hope Scale, which continues to be used today, as a way to measure hope. He suggested that some people have higher levels of hope than others and there seem to be benefits to being more hopeful.
“For example, we would expect that higher as compared with lower hope people are more likely to have a healthy lifestyle, to avoid life crises, and to cope better with stressors when they are encountered,” they write.
Others have suggested broader definitions.
In 1992, Kaye Herth, a professor of nursing and a scholar on hope, defined hope as “a multidimensional dynamic life force characterized by a confident yet uncertain expectation of achieving good, which to the hoping person, is realistically possible and personally significant.” Herth also developed the Herth Hope Index, which is used in various settings, including clinical practice and research.
More recently, others have offered an even broader definition of hope.
Anthony Scioli, a clinical psychologist and author of several books on hope, defines hope “as an emotion with spiritual dimensions,” in a 2023 review published in Current Opinion in Psychology. “Hope is best viewed as an ameliorating emotion, designed to fill the liminal space between need and reality.”
Hope is also nuanced.
“Our hopes may be active or passive, patient or critical, private or collective, grounded in the evidence or resolute in spite of it, socially conservative or socially transformative,” writes Darren Webb in a 2007 study published in History of the Human Sciences. “We all hope, but we experience this most human of all mental feelings in a variety of modes.”
To be sure, a few studies have shown that hope can have negative outcomes in certain populations and situations. For example, one study highlighted in the research roundup below finds that Black college students who had higher levels of hope experienced more stress due to racial discrimination compared with Black students who had lower levels of hope.
Today, hope is one of the most well-studied constructs within the field of positive psychology, according to the journal Current Opinion in Psychology, which dedicated its August 2023 issue to the subject. (Positive psychology is a branch of psychology focused on characters and behaviors that allow people to flourish.)
We’ve gathered several studies below to help you think more deeply about hope and recognize its role in your everyday lives.
Research roundup
The Role of Hope in Subsequent Health and Well-Being For Older Adults: An Outcome-Wide Longitudinal Approach
Katelyn N.G. Long, et al. Global Epidemiology, November 2020.The study: To explore the potential public health implications of hope, researchers examine the relationship between hope and physical, behavioral and psychosocial outcomes in 12,998 older adults in the U.S. with a mean age of 66.
Researchers note that most investigations on hope have focused on psychological and social well-being outcomes and less attention has been paid to its impact on physical and behavioral health, particularly among older adults.
The findings: Results show a positive association between an increased sense of hope and a variety of behavioral and psychosocial outcomes, such as fewer sleep problems, more physical activity, optimism and satisfaction with life. However, there wasn’t a clear association between hope and all physical health outcomes. For instance, hope was associated with a reduced number of chronic conditions, but not with stroke, diabetes and hypertension.
The takeaway: “The later stages of life are often defined by loss: the loss of health, loved ones, social support networks, independence, and (eventually) loss of life itself,” the authors write. “Our results suggest that standard public health promotion activities, which often focus solely on physical health, might be expanded to include a wider range of factors that may lead to gains in hope. For example, alongside community-based health and nutrition programs aimed at reducing chronic conditions like hypertension, programs that help strengthen marital relations (e.g., closeness with a spouse), provide opportunities to volunteer, help lower anxiety, or increase connection with friends may potentially increase levels of hope, which in turn, may improve levels of health and well-being in a variety of domains.”
Associated Factors of Hope in Cancer Patients During Treatment: A Systematic Literature Review
Corine Nierop-van Baalen, Maria Grypdonck, Ann van Hecke and Sofie Verhaeghe. Journal of Advanced Nursing, March 2020.The study: The authors review 33 studies, written in English or Dutch and published in the past decade, on the relationship between hope and the quality of life and well-being of patients with cancer. Studies have shown that many cancer patients respond to their diagnosis by nurturing hope, while many health professionals feel uneasy when patients’ hopes go far beyond their prognosis, the authors write.
The findings: Quality of life, social support and spiritual well-being were positively associated with hope, as measured with various scales. Whereas symptoms, psychological distress and depression had a negative association with hope. Hope didn’t seem to be affected by the type or stage of cancer or the patient’s demographics.
The takeaway: “Hope seems to be a process that is determined by a person’s inner being rather than influenced from the outside,” the authors write. “These factors are typically given meaning by the patients themselves. Social support, for example, is not about how many patients experience support, but that this support has real meaning for them.”
Characterizing Hope: An Interdisciplinary Overview of the Characteristics of Hope
Emma Pleeging, Job van Exel and Martijn Burger. Applied Research in Quality of Life, September 2021.The study: This systematic review provides an overview of the concept of hope based on 66 academic papers in ten academic fields, including economics and business studies, environmental studies, health studies, history, humanities, philosophy, political science, psychology, social science, theology and youth studies, resulting in seven themes and 41 sub-themes.
The findings: The authors boil down their findings to seven components: internal and external sources, the individual and social experience of hope, internal and external effects, and the object of hope, which can be “just about anything we can imagine,” the authors write.
The takeaway: “An important implication of these results lies in the way hope is measured in applied and scientific research,” researchers write. “When measuring hope or developing instruments to measure it, researchers could be well-advised to take note of the broader understanding of the topic, to prevent that important characteristics might be overlooked.”
Revisiting the Paradox of Hope: The Role of Discrimination Among First-Year Black College Students
Ryon C. McDermott, et al. Journal of Counseling Psychology, March 2020.The study: Researchers examine the moderating effects of hope on the association between experiencing racial discrimination, stress and academic well-being among 203 first-year U.S. Black college students. They build on a small body of evidence that suggests high levels of hope might have a negative effect on Black college students who experience racial discrimination.
The authors use data gathered as part of an annual paper-and-pencil survey of first-year college students at a university on the Gulf Coast, which the study doesn’t identify.
The findings: Researchers find that Black students who had higher levels of hope experienced more stress due to racial discrimination compared with students who had lower levels of hope. On the other hand, Black students with low levels of hope may be less likely to experience stress when they encounter discrimination.
Meanwhile, Black students who had high levels of hope were more successful in academic integration — which researchers define as satisfaction with and integration into the academic aspects of college life — despite facing discrimination. But low levels of hope had a negative impact on students’ academic well-being.
“The present study found evidence that a core construct in positive psychology, hope, may not always protect Black students from experiencing the psychological sting of discrimination, but it was still beneficial to their academic well-being,” the authors write.
The takeaway: “Our findings also highlight an urgent need to reduce discrimination on college campuses,” the researchers write. “Reducing discrimination could help Black students (and other racial minorities) avoid additional stress, as well as help them realize the full psychological and academic benefits of having high levels of hope.”
Additional reading
Hope Across Cultural Groups Lisa M. Edwards and Kat McConnell. Current Opinion in Psychology, February 2023.
The Psychology of Hope: A Diagnostic and Prescriptive Account Anthony Scioli. “Historical and Multidisciplinary Perspectives on Hope,” July 2020.
Hope Theory: Rainbows in the Mind C.R. Snyder. Psychological Inquiry, 2002
This article first appeared on The Journalist’s Resource and is republished here under a Creative Commons license.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: