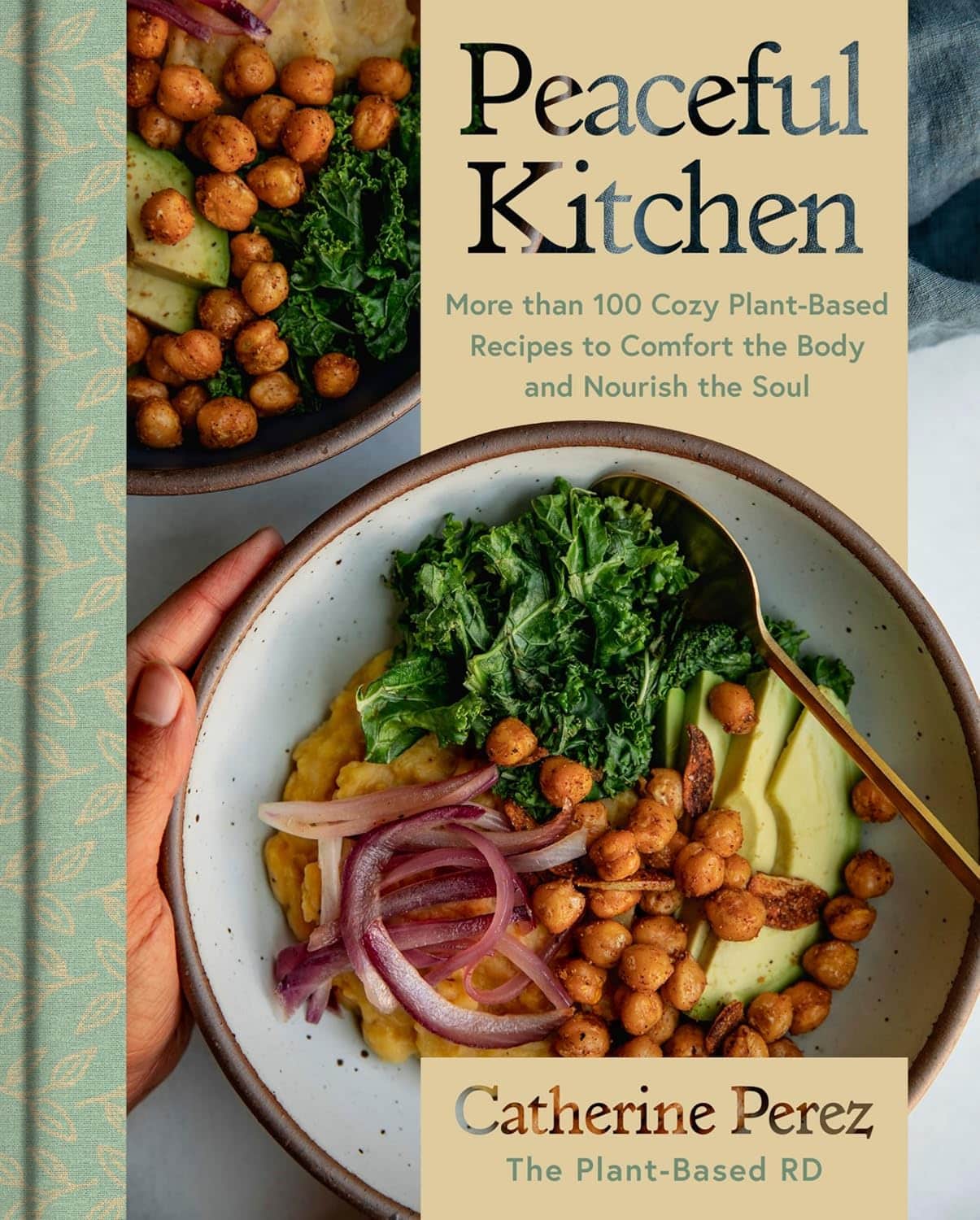
Peaceful Kitchen – by Catherine Perez
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
The author, a keen cook and Registered Dietician with a Master’s in same, covers the basics of the science of nutrition as relevant to her recipes, but first and foremost this is not a science textbook—it’s a cookbook, and its pages contain more love for the art than citations for the (perfectly respectable) science.
Mexican and Dominican cuisine are the main influences in this book, but there are dishes from around the world too.
The recipes themselves are… Comparable in difficulty to the things we often feature in our recipes section here at 10almonds. They’re probably not winning any restaurants Michelin stars, but they’re not exactly student survival recipes either. They’re made from mostly non-obscure whole foods, nutritionally-dense ingredients at that, with minimal processed foods involved.
That said, she does take a “add, don’t subtract” approach to nutrition, i.e. focussing more on adding in diversity of plants than on “don’t eat this; don’t eat that” mandates.
If there’s any criticism to be levelled at the book, it’s that in most cases we’d multiply the spices severalfold, but that’s not a big problem as readers can always judge that individually; she’s given the basic information of which spices in which proportions, which is the key knowledge.
Bottom line: if you’re looking to expand your plant-based cooking repertoire, this one is a fine choice.
Click here to check out Peaceful Kitchen, and try some new things!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
The Path to a Better Tuberculosis Vaccine Runs Through Montana
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
A team of Montana researchers is playing a key role in the development of a more effective vaccine against tuberculosis, an infectious disease that has killed more people than any other.
The BCG (Bacille Calmette-Guérin) vaccine, created in 1921, remains the sole TB vaccine. While it is 40% to 80% effective in young children, its efficacy is very low in adolescents and adults, leading to a worldwide push to create a more powerful vaccine.
One effort is underway at the University of Montana Center for Translational Medicine. The center specializes in improving and creating vaccines by adding what are called novel adjuvants. An adjuvant is a substance included in the vaccine, such as fat molecules or aluminum salts, that enhances the immune response, and novel adjuvants are those that have not yet been used in humans. Scientists are finding that adjuvants make for stronger, more precise, and more durable immunity than antigens, which create antibodies, would alone.
Eliciting specific responses from the immune system and deepening and broadening the response with adjuvants is known as precision vaccination. “It’s not one-size-fits-all,” said Ofer Levy, a professor of pediatrics at Harvard University and the head of the Precision Vaccines Program at Boston Children’s Hospital. “A vaccine might work differently in a newborn versus an older adult and a middle-aged person.”
The ultimate precision vaccine, said Levy, would be lifelong protection from a disease with one jab. “A single-shot protection against influenza or a single-shot protection against covid, that would be the holy grail,” Levy said.
Jay Evans, the director of the University of Montana center and the chief scientific and strategy officer and a co-founder of Inimmune, a privately held biotechnology company in Missoula, said his team has been working on a TB vaccine for 15 years. The private-public partnership is developing vaccines and trying to improve existing vaccines, and he said it’s still five years off before the TB vaccine might be distributed widely.
It has not gone unnoticed at the center that this state-of-the-art vaccine research and production is located in a state that passed one of the nation’s most extreme anti-vaccination laws during the pandemic in 2021. The law prohibits businesses and governments from discriminating against people who aren’t vaccinated against covid-19 or other diseases, effectively banning both public and private employers from requiring workers to get vaccinated against covid or any other disease. A federal judge later ruled that the law cannot be enforced in health care settings, such as hospitals and doctors’ offices.
In mid-March, the Bill & Melinda Gates Medical Research Institute announced it had begun the third and final phase of clinical trials for the new vaccine in seven countries. The trials should take about five years to complete. Research and production are being done in several places, including at a manufacturing facility in Hamilton owned by GSK, a giant pharmaceutical company.
Known as the forgotten pandemic, TB kills up to 1.6 million people a year, mostly in impoverished areas in Asia and Africa, despite its being both preventable and treatable. The U.S. has seen an increase in tuberculosis over the past decade, especially with the influx of migrants, and the number of cases rose by 16% from 2022 to 2023. Tuberculosis is the leading cause of death among people living with HIV, whose risk of contracting a TB infection is 20 times as great as people without HIV.
“TB is a complex pathogen that has been with human beings for ages,” said Alemnew Dagnew, who heads the program for the new vaccine for the Gates Medical Research Institute. “Because it has been with human beings for many years, it has evolved and has a mechanism to escape the immune system. And the immunology of TB is not fully understood.”
The University of Montana Center for Translational Medicine and Inimmune together have 80 employees who specialize in researching a range of adjuvants to understand the specifics of immune responses to different substances. “You have to tailor it like tools in a toolbox towards the pathogen you are vaccinating against,” Evans said. “We have a whole library of adjuvant molecules and formulations.”
Vaccines are made more precise largely by using adjuvants. There are three basic types of natural adjuvants: aluminum salts; squalene, which is made from shark liver; and some kinds of saponins, which are fat molecules. It’s not fully understood how they stimulate the immune system. The center in Missoula has also created and patented a synthetic adjuvant, UM-1098, that drives a specific type of immune response and will be added to new vaccines.
One of the most promising molecules being used to juice up the immune system response to vaccines is a saponin molecule from the bark of the quillay tree, gathered in Chile from trees at least 10 years old. Such molecules were used by Novavax in its covid vaccine and by GSK in its widely used shingles vaccine, Shingrix. These molecules are also a key component in the new tuberculosis vaccine, known as the M72 vaccine.
But there is room for improvement.
“The vaccine shows 50% efficacy, which doesn’t sound like much, but basically there is no effective vaccine currently, so 50% is better than what’s out there,” Evans said. “We’re looking to take what we learned from that vaccine development with additional adjuvants to try and make it even better and move 50% to 80% or more.”
By contrast, measles vaccines are 95% effective.
According to Medscape, around 15 vaccine candidates are being developed to replace the BCG vaccine, and three of them are in phase 3 clinical trials.
One approach Evans’ center is researching to improve the new vaccine’s efficacy is taking a piece of the bacterium that causes TB, synthesizing it, and combining it with the adjuvant QS-21, made from the quillay tree. “It stimulates the immune system in a way that is specific to TB and it drives an immune response that is even closer to what we get from natural infections,” Evans said.
The University of Montana center is researching the treatment of several problems not commonly thought of as treatable with vaccines. They are entering the first phase of clinical trials for a vaccine for allergies, for instance, and first-phase trials for a cancer vaccine. And later this year, clinical trials will begin for vaccines to block the effects of opioids like heroin and fentanyl. The University of Montana received the largest grant in its history, $33 million, for anti-opioid vaccine research. It works by creating an antibody that binds with the drug in the bloodstream, which keeps it from entering the brain and creating the high.
For now, though, the eyes of health care experts around the world are on the trials for the new TB vaccines, which, if they are successful, could help save countless lives in the world’s poorest places.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
Subscribe to KFF Health News’ free Morning Briefing.
Share This Post
-
Health Tips for Males Too
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? You can always hit “reply” to any of our emails, or use the feedback widget at the bottom!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Articles are very informative and helpful. Maybe it’s me but things seem to lean more toward females. That being said don’t forget us males❞
Rest assured, we could never forget you! We try to make as much as possible of our content applicable to as many as possible of our readers, but of course not everything can be relevant for everyone.
This is, presumably, in response to our recent feature on menopausal health, because previous to that, our next-most-recent main feature that centred women’s health was a month ago—that was about breast cancer, and did have a section on breast cancer in men too. You might also enjoy the book we reviewed recently about prostate health, or our regular sponsor offering testosterone therapy. Please feel free to check out our articles on saw palmetto against male pattern baldness and BPH, as well as mental health issues that disproportionally affect men.
And of course, if you have specific questions/requests about men’s health (or any other health topic) we’re only ever an email away (or use the handy feedback widget, as you did to make this request)!
Share This Post
-
Why is pain so exhausting?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
One of the most common feelings associated with persisting pain is fatigue and this fatigue can become overwhelming. People with chronic pain can report being drained of energy and motivation to engage with others or the world around them.
In fact, a study from the United Kingdom on people with long-term health conditions found pain and fatigue are the two biggest barriers to an active and meaningful life.
But why is long-term pain so exhausting? One clue is the nature of pain and its powerful effect on our thoughts and behaviours.
simona pilolla 2/Shutterstock Short-term pain can protect you
Modern ways of thinking about pain emphasise its protective effect – the way it grabs your attention and compels you to change your behaviour to keep a body part safe.
Try this. Slowly pinch your skin. As you increase the pressure, you’ll notice the feeling changes until, at some point, it becomes painful. It is the pain that stops you squeezing harder, right? In this way, pain protects us.
When we are injured, tissue damage or inflammation makes our pain system become more sensitive. This pain stops us from mechanically loading the damaged tissue while it heals. For instance, the pain of a broken leg or a cut under our foot means we avoid walking on it.
The concept that “pain protects us and promotes healing” is one of the most important things people who were in chronic pain tell us they learned that helped them recover.
But long-term pain can overprotect you
In the short term, pain does a terrific job of protecting us and the longer our pain system is active, the more protective it becomes.
But persistent pain can overprotect us and prevent recovery. People in pain have called this “pain system hypersensitivity”. Think of this as your pain system being on red alert. And this is where exhaustion comes in.
When pain becomes a daily experience, triggered or amplified by a widening range of activities, contexts and cues, it becomes a constant drain on one’s resources. Going about life with pain requires substantial and constant effort, and this makes us fatigued.
About 80% of us are lucky enough to not know what it is like to have pain, day in day out, for months or years. But take a moment to imagine what it would be like.
Imagine having to concentrate hard, to muster energy and use distraction techniques, just to go about your everyday tasks, let alone to complete work, caring or other duties.
Whenever you are in pain, you are faced with a choice of whether, and how, to act on it. Constantly making this choice requires thought, effort and strategy.
Mentioning your pain, or explaining its impact on each moment, task or activity, is also tiring and difficult to get across when no-one else can see or feel your pain. For those who do listen, it can become tedious, draining or worrying.
Concentrating hard, mustering energy and using distraction techniques can make everyday life exhausting. PRPicturesProduction/Shutterstock No wonder pain is exhausting
In chronic pain, it’s not just the pain system on red alert. Increased inflammation throughout the body (the immune system on red alert), disrupted output of the hormone cortisol (the endocrine system on red alert), and stiff and guarded movements (the motor system on red alert) also go hand in hand with chronic pain.
Each of these adds to fatigue and exhaustion. So learning how to manage and resolve chronic pain often includes learning how to best manage the over-activation of these systems.
Loss of sleep is also a factor in both fatigue and pain. Pain causes disruptions to sleep, and loss of sleep contributes to pain.
In other words, chronic pain is seldom “just” pain. No wonder being in long-term pain can become all-consuming and exhausting.
What actually works?
People with chronic pain are stigmatised, dismissed and misunderstood, which can lead to them not getting the care they need. Ongoing pain may prevent people working, limit their socialising and impact their relationships. This can lead to a descending spiral of social, personal and economic disadvantage.
So we need better access to evidence-based care, with high-quality education for people with chronic pain.
There is good news here though. Modern care for chronic pain, which is grounded in first gaining a modern understanding of the underlying biology of chronic pain, helps.
The key seems to be recognising, and accepting, that a hypersensitive pain system is a key player in chronic pain. This makes a quick fix highly unlikely but a program of gradual change – perhaps over months or even years – promising.
Understanding how pain works, how persisting pain becomes overprotective, how our brains and bodies adapt to training, and then learning new skills and strategies to gradually retrain both brain and body, offers scientifically based hope; there’s strong supportive evidence from clinical trials.
Every bit of support helps
The best treatments we have for chronic pain take effort, patience, persistence, courage and often a good coach. All that is a pretty overwhelming proposition for someone already exhausted.
So, if you are in the 80% of the population without chronic pain, spare a thought for what’s required and support your colleague, friend, partner, child or parent as they take on the journey.
More information about chronic pain is available from Pain Revolution.
Michael Henry, Physiotherapist and PhD candidate, Body in Mind Research Group, University of South Australia and Lorimer Moseley, Professor of Clinical Neurosciences and Foundation Chair in Physiotherapy, University of South Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Share This Post
Related Posts
-
Once-A-Week Strategy to Stop Procrastination – by Brad Meir
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Procrastination is perhaps the most frustrating bad habit to kick!
We know we should do the things. We know why we should do the things. We want to do the things. We’re afraid of what will happen if we don’t do the things. And then we… don’t do the things? What is going on?!
Brad Meir has answers, and—what a relief—solutions. But enough about him, because first he wants to focus a little on you:
Why do you procrastinate? No, you’re probably not “just lazy”, and he’ll guide you through figuring out what it is that makes you procrastinate. There’s an exploration of various emotions here, as well as working out: what type of procrastinator are you?
Then, per what you figured out with his guidance, exercises, and tests, it’s time for an action plan.
But, importantly: one you can actually do, because it won’t fall foul of the problems you’ve been encountering so far. The exact mechanism you’ll use may vary a bit based on you, but some tools here are good for everyone—as well as an outline of the mistakes you could easily make, and how to avoid falling into those traps. And, last but very definitely not least, his “once a week plan”, per the title.
All in all, a highly recommendable and potentially life-changing book.
Grab Your Copy of “Once-A-Week Strategy to Stop Procrastination” NOW (don’t put it off!)
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Death by Food Pyramid – by Denise Minger
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This one is less about “here’s the perfect way of eating” or even “these specific foods are ontologically evil”, but more about teaching science literacy.
The author explores various health trends from the 70s until time of writing (the book was published in 2014), what rationales originally prompted them, and what social phenomena either helped them to persist, or caused them to get dropped quite quickly.
Of course, even in the case of fads that are societally dropped quite quickly, on an individual level there will always be someone just learning about it for the first time, reading some older material, and thinking “that sounds like just the miracle life-changer I need!”
What she teaches the reader to do is largely what we do a lot of here at 10almonds—examine the claims, go to the actual source material (studies! Not just books about studies!), and see whether the study conclusions actually support the claim, to start with, and then further examine to see if there’s some way (or sometimes, a plurality of ways) in which the study itself is methodologically flawed.
Which does happen sometimes, do actually watch out for that!
The style is quite personal and entertaining for the most part, and yet even moving sometimes (the title is not hyperbole; deaths will be discussed). As one might expect of a book teaching science literacy, it’s very easy to read, with copious footnotes (well, actually they are at the back of the book doubling up as a bibliography, but they are linked-to throughout) for those who wish to delve deeper—something the author, of course, encourages.
Bottom line: if you’d like to be able to sort the real science from the hype yourself, then this book can set you on the right track!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Scarcity Brain – by Michael Easter
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
After a brief overview of theevolutionary psychology underpinnings of the scarcity brain, the author grounds the rest of this book firmly in the present. He explains how the scarcity loop hooks us and why we crave more, and what factors can increase or lessen its hold over us.
As for what things we are wired to consider “potentially scarce any time now” no matter how saturated we are in them, he looks at an array of categories, each with their nuances. From the obvious such as “food” and “stuff“, to understandable “information” and “happiness“, to abstractions like “influence“, he goes to many sources—experts of various kinds from around the world—to explore how we can know “how much is enough”, and—which can be harder—act accordingly.
The key, he argues, is not in simply wanting less, but in understanding why we crave more in the first place, get rid of our worst habits, and use what we already have, better.
Bottom line: if you feel a gnawing sense of needing more “to be on the safe side”, this book can help you to be a little more strategic (and at the same time, less stressed!) about that.
Click here to check out Scarcity Brain, and manage yours more mindfully!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: