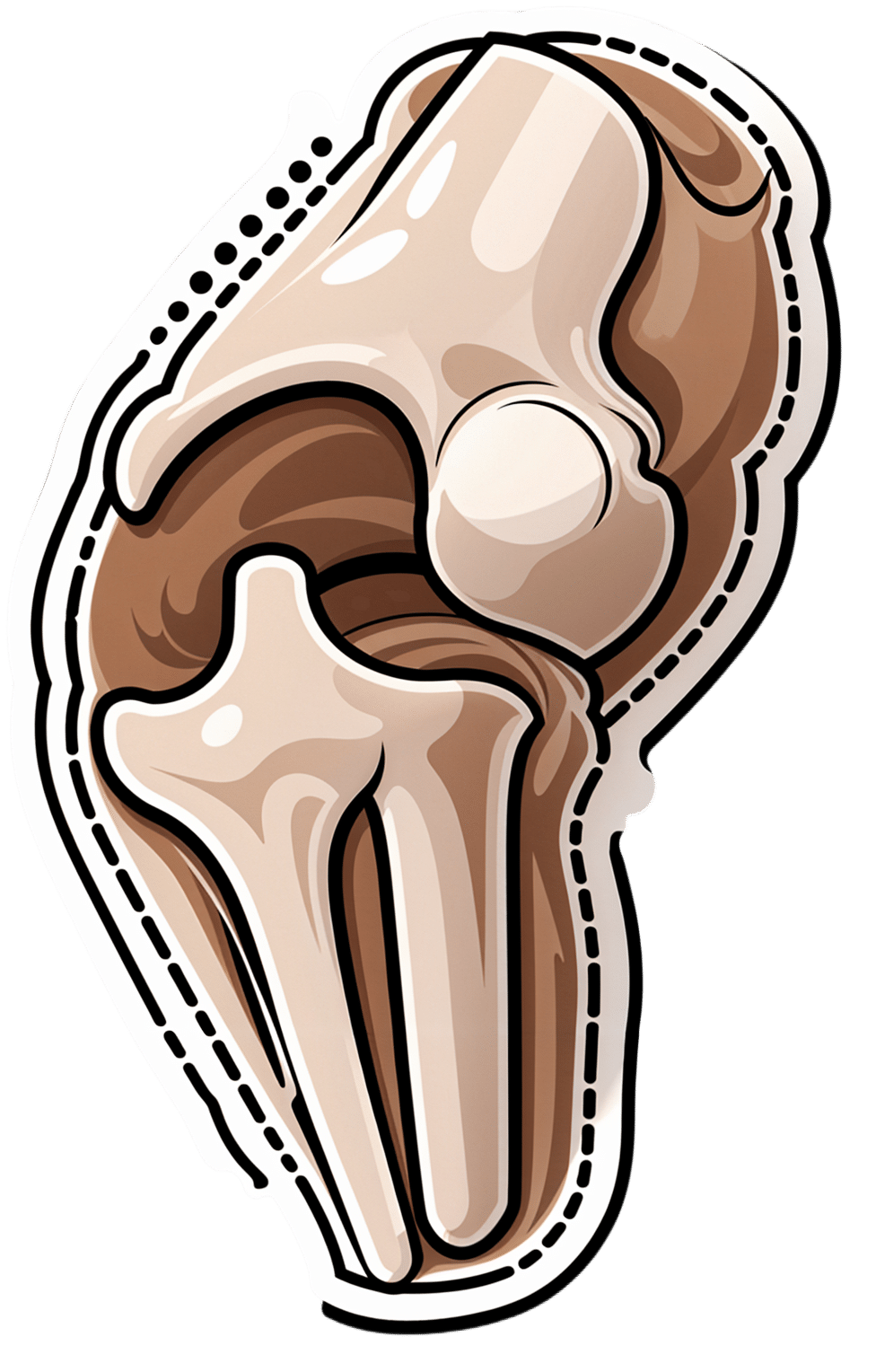
Osteoarthritis Of The Knee
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
It’s Q&A Day at 10almonds!
Have a question or a request? We love to hear from you!
In cases where we’ve already covered something, we might link to what we wrote before, but will always be happy to revisit any of our topics again in the future too—there’s always more to say!
As ever: if the question/request can be answered briefly, we’ll do it here in our Q&A Thursday edition. If not, we’ll make a main feature of it shortly afterwards!
So, no question/request too big or small
❝Very informative thank you. And made me think. I am a 72 yr old whitewoman, have never used ( or even been offered) HRT since menopause ~15 yrs ago. Now I’m wondering if it would have delayed the onset of osteoarthritis ( knee) and give me more energy in general. And is it wise to start taking hrt after being without those hormones for so long?❞
(this was in response to our article about menopausal HRT)
Thanks for writing! To answer your first question, obviously we can never know for sure now, but it certainly is possible, per for example a large-ish (n=1003) study of women aged 45–64, in which:
- Those with HRT were significantly less likely to have knee arthritis than those without
- However, to enjoy this benefit depended on continued use (those who used it for a bit and then stopped did not enjoy the same results)
- While it made a big difference to knee arthritis, it made only a small (but still beneficial) difference to wrist/hand arthritis.
We could hypothesize that this is because the mechanism of action is more about strengthening the bones (proofing against osteoporosis is one of the main reasons many people take HRT) and cartilage than it is against inflammation directly.
Since the knee is load-bearing and the hand/wrist joints usually are not, this would mean the HRT strengthening the bones makes a big difference to the “wear and tear” aspect of potential osteoarthritis of the knee, but not the same level of benefit for the hand/wrist, which is less about wear and tear and more about inflammatory factors. But that latter, about it being load-bearing, is just this writer’s hypothesis as to why the big difference.
The researchers do mention:
❝In OA the mechanisms by which HRT might act are highly speculative, but could entail changes in cartilage repair or bone turnover, perhaps with cytokines such as interleukin 6, for example.❞
What is clear though, is that it does indeed appear to have a protective effect against osteoarthritis of the knee.
With regard to the timing, the researchers do note:
❝Why as little as three years of HRT should have a demonstrable effect is unclear. Given the difficulty in ascertaining when the disease starts, it is hard to be sure of the importance of the timing of HRT, and whether early or subclinical disease was present.
These results taken together suggest that HRT has a metabolic action that is only effective if given continuously, perhaps by preventing disease initiation; once HRT is stopped there might be a ‘rebound’ effect, explaining the rapid return to normal risk❞
~ Ibid.
You can read the study here:
On whether it is worth it now…
Again, do speak with an endocrinologist because your situation may vary, but:
- hormones are simply messengers, and your body categorically will respond to those messages regardless of age, or time elapsed without having received such a message. Whether it will repair all damage done is another matter entirely, but it would take a biological miracle for it to have no effect at all.
- anecdotally, many women do enjoy life-changing benefits upon starting HRT at your age and older!
(We don’t like to rely on “anecdotally”, but we couldn’t find studies isolating according to “length of time since menopause”—we’ll keep an eye out and if we find something in the future, we’ll mention it!)
Meanwhile, take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Chickpeas vs Black Beans – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing chickpeas to black beans, we picked the black beans.
Why?
They’re both great! But we consider the nutritional profile of black beans to be better:
In terms of macros, black beans have a little more protein, while chickpeas have more carbohydrates. Generally speaking, people are not usually short of carbs in their diet, so we’ll go with the one with more protein. Black beans also have more fiber, which is important for heart health and more.
In the category of micronutrients, black beans have twice as much potassium and twice as much calcium, as well as twice as much magnesium. Chickpeas, meanwhile are better for manganese and slightly higher in B vitamins, but B vitamins are everywhere (especially vitamin B5, pantothenic acid; that’s literally where its name comes from, it means “from everywhere”), so we don’t consider that as much of a plus as the black beans doubling up on potassium, calcium, and magnesium.
So, do enjoy both, but if you’re going to pick, or lean more heavily on one, we recommend the black beans
Further reading
See also:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Easily Digestible Vegetarian Protein Sources
- What Matters Most For Your Heart? Eat More (Of This) For Lower Blood Pressure
Enjoy!
Share This Post
-
The 5 Resets – by Dr. Aditi Nerurkar
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What this book isn’t: an advice to go on a relaxing meditation retreat, or something like that.
What this is: a science-based guide to what actually works.
There’s no need to be mysterious, so we’ll mention that the titular “5 resets” are:
- What matters most
- Quiet in a noisy world
- Leveraging the brain-body connection
- Coming up for air (regaining perspective)
- Bringing your best self forward
All of these are things we can easily lose sight of in the hustle and bustle of daily life, so having a system for keeping them on track can make a huge difference!
The style is personable and accessible, while providing a lot of strongly science-backed tips and tricks along the way.
Bottom line: if life gets away from you a little too often for comfort, this book can help you keep on top of things with a lot less stress.
Click here to check out “The 5 Resets”, and take control with conscious calm!
Share This Post
-
Plum vs Nectarine – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing plums to nectarines, we picked the nectarines.
Why?
Both are great! But nectarines win at least marginally in each category we look at.
In terms of macros, plums have more carbs while nectarines have more fiber, resulting of course in a lower glycemic index. Plums do have a low GI also; just, nectarines have it better.
When it comes to vitamins, plums have more of vitamins A, B6, C, and K, while nectarines have more of vitamins B1, B2, B3, B5, E, and choline.
In the category of minerals, plums are great but not higher in any mineral than nectarines; nectarines meanwhile have more copper, iron, magnesium, manganese, phosphorus, potassium, and zinc.
All in all, enjoy both. And if having dried fruit, then prunes (dried plums) are generally more widely available than dried nectarines. But if you’re choosing one fruit or the other, nectarine is the way to go.
Want to learn more?
You might like to read:
- Why You’re Probably Not Getting Enough Fiber (And How To Fix It)
- Replacing Sugar: Top 10 Anti-Inflammatory Sweet Foods
- Top 8 Fruits That Prevent & Kill Cancer
Take care!
Share This Post
Related Posts
-
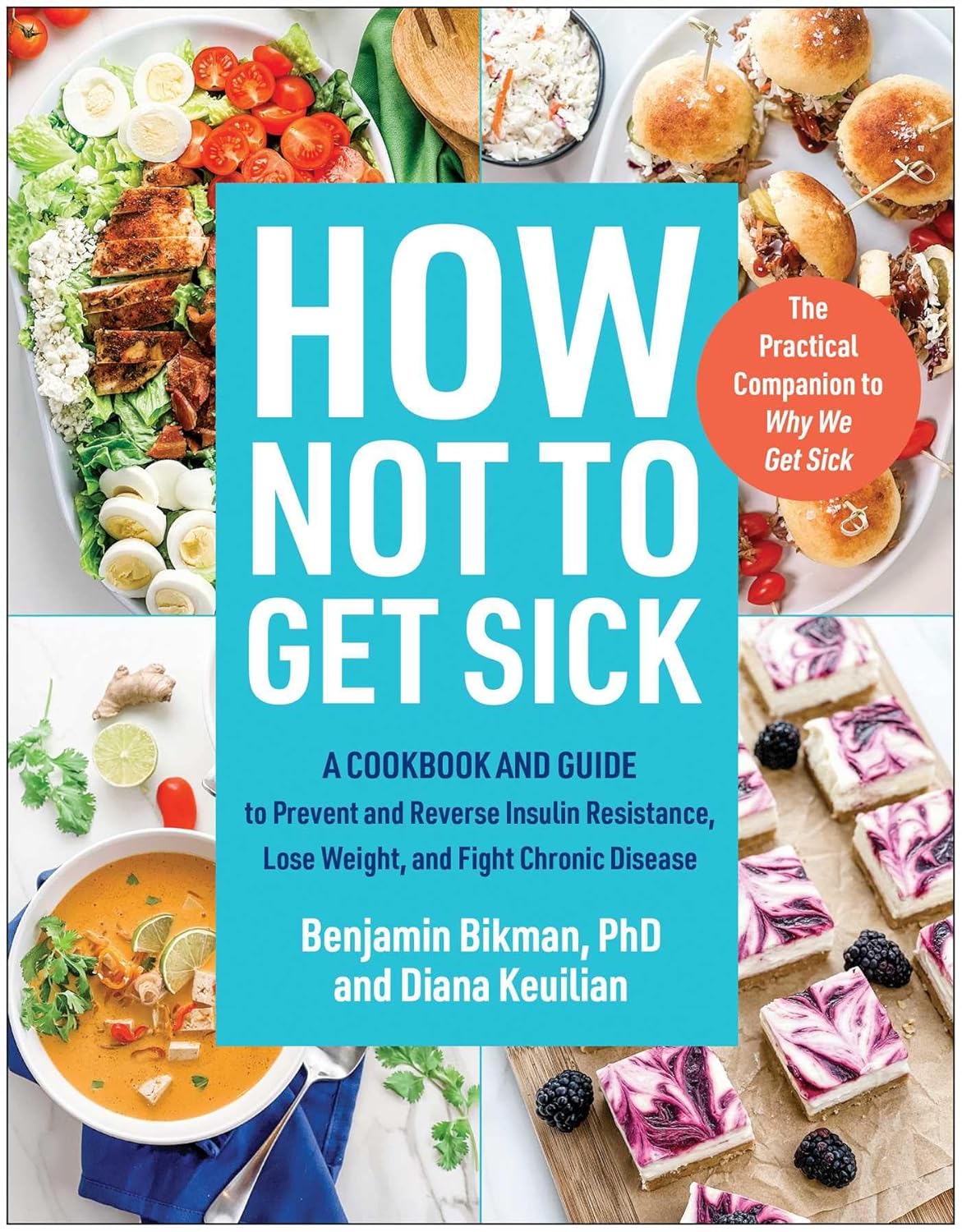
How Not To Get Sick: A Cookbook – by Dr. Benjamin Bikman and Diana Keuilian
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We’ve previously reviewed Dr. Bikman’s excellent “Why We Get Sick”, and if you haven’t read that yet, we recommend doing so.
Nevertheless, you don’t need to have read it to benefit from this one, which is about cooking with those learnings (from the other book) in mind.
Before getting to the recipes, we get a section recapping what we learned previously, as well as adding some more general lifestyle advices beyond the kitchen. The science is also expanded a bit, to include such things as the two-way relationship between insulin and aging, as well as the interplay with other metrics of health, including blood lipids, for example.
The authors then provide a plan, in the three stages: reverse (insulin resistance), prevent (insulin resistance), maintain (insulin sensitivity).
The recipes themselves, of which there are 70, are of course tailored to do the above three things; they’re also quite diverse, albeit if you are vegetarian or vegan, you should know in advance that most of these recipes are not.
Bottom line: if the above doesn’t apply to you, and you would like to improve your insulin sensitivity, this book can indeed help.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
People with dementia aren’t currently eligible for voluntary assisted dying. Should they be?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Dementia is the second leading cause of death for Australians aged over 65. More than 421,000 Australians currently live with dementia and this figure is expected to almost double in the next 30 years.
There is ongoing public discussion about whether dementia should be a qualifying illness under Australian voluntary assisted dying laws. Voluntary assisted dying is now lawful in all six states, but is not available for a person living with dementia.
The Australian Capital Territory has begun debating its voluntary assisted dying bill in parliament but the government has ruled out access for dementia. Its view is that a person should retain decision-making capacity throughout the process. But the bill includes a requirement to revisit the issue in three years.
The Northern Territory is also considering reform and has invited views on access to voluntary assisted dying for dementia.
Several public figures have also entered the debate. Most recently, former Australian Chief Scientist, Ian Chubb, called for the law to be widened to allow access.
Others argue permitting voluntary assisted dying for dementia would present unacceptable risks to this vulnerable group.
Inside Creative House/Shutterstock Australian laws exclude access for dementia
Current Australian voluntary assisted dying laws exclude access for people who seek to qualify because they have dementia.
In New South Wales, the law specifically states this.
In the other states, this occurs through a combination of the eligibility criteria: a person whose dementia is so advanced that they are likely to die within the 12 month timeframe would be highly unlikely to retain the necessary decision-making capacity to request voluntary assisted dying.
This does not mean people who have dementia cannot access voluntary assisted dying if they also have a terminal illness. For example, a person who retains decision-making capacity in the early stages of Alzheimer’s disease with terminal cancer may access voluntary assisted dying.
What happens internationally?
Voluntary assisted dying laws in some other countries allow access for people living with dementia.
One mechanism, used in the Netherlands, is through advance directives or advance requests. This means a person can specify in advance the conditions under which they would want to have voluntary assisted dying when they no longer have decision-making capacity. This approach depends on the person’s family identifying when those conditions have been satisfied, generally in consultation with the person’s doctor.
Another approach to accessing voluntary assisted dying is to allow a person with dementia to choose to access it while they still have capacity. This involves regularly assessing capacity so that just before the person is predicted to lose the ability to make a decision about voluntary assisted dying, they can seek assistance to die. In Canada, this has been referred to as the “ten minutes to midnight” approach.
But these approaches have challenges
International experience reveals these approaches have limitations. For advance directives, it can be difficult to specify the conditions for activating the advance directive accurately. It also requires a family member to initiate this with the doctor. Evidence also shows doctors are reluctant to act on advance directives.
Particularly challenging are scenarios where a person with dementia who requested voluntary assisted dying in an advance directive later appears happy and content, or no longer expresses a desire to access voluntary assisted dying.
What if the person changes their mind? Jokiewalker/Shutterstock Allowing access for people with dementia who retain decision-making capacity also has practical problems. Despite regular assessments, a person may lose capacity in between them, meaning they miss the window before midnight to choose voluntary assisted dying. These capacity assessments can also be very complex.
Also, under this approach, a person is required to make such a decision at an early stage in their illness and may lose years of otherwise enjoyable life.
Some also argue that regardless of the approach taken, allowing access to voluntary assisted dying would involve unacceptable risks to a vulnerable group.
More thought is needed before changing our laws
There is public demand to allow access to voluntary assisted dying for dementia in Australia. The mandatory reviews of voluntary assisted dying legislation present an opportunity to consider such reform. These reviews generally happen after three to five years, and in some states they will occur regularly.
The scope of these reviews can vary and sometimes governments may not wish to consider changes to the legislation. But the Queensland review “must include a review of the eligibility criteria”. And the ACT bill requires the review to consider “advanced care planning”.
Both reviews would require consideration of who is able to access voluntary assisted dying, which opens the door for people living with dementia. This is particularly so for the ACT review, as advance care planning means allowing people to request voluntary assisted dying in the future when they have lost capacity.
The legislation undergoes a mandatory review. Jenny Sturm/Shutterstock This is a complex issue, and more thinking is needed about whether this public desire for voluntary assisted dying for dementia should be implemented. And, if so, how the practice could occur safely, and in a way that is acceptable to the health professionals who will be asked to provide it.
This will require a careful review of existing international models and their practical implementation as well as what would be feasible and appropriate in Australia.
Any future law reform should be evidence-based and draw on the views of people living with dementia, their family caregivers, and the health professionals who would be relied on to support these decisions.
Ben White, Professor of End-of-Life Law and Regulation, Australian Centre for Health Law Research, Queensland University of Technology; Casey Haining, Research Fellow, Australian Centre for Health Law Research, Queensland University of Technology; Lindy Willmott, Professor of Law, Australian Centre for Health Law Research, Queensland University of Technology, Queensland University of Technology, and Rachel Feeney, Postdoctoral research fellow, Queensland University of Technology
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Coffee, From A Blood Sugar Management Perspective
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our favorite French biochemist (Jessie Inchauspé) is back, and this time, she’s tackling a topic near and dear to this writer’s heart: coffee ☕💕
What to consider
Depending on how you like your coffee, some or all of these may apply to you:
- Is coffee healthy? Coffee is generally healthy, reducing the risk of type 2 diabetes by improving fat burning in the liver and protecting beta cells in the pancreas.
- Does it spike blood sugars? Usually not so long as it’s black and unsweetened. Black coffee can cause small glucose spikes in some people due to stress-induced glucose release, but only if it contains caffeine.
- When is it best to drink it? Drinking coffee after breakfast, especially after a poor night’s sleep, can actually reduce glucose and insulin spikes.
- What about milk? All milks cause some glucose and insulin spikes. While oat milk is generally healthy, for blood sugar purposes unsweetened nut milks or even whole cow’s milk (but not skimmed; it needs the fat) are better options as they cause smaller spikes.
- What about sweetening? Adding sugar to coffee, especially on an empty stomach, obviously leads to large glucose spikes. Alternative sweeteners like stevia or sweet cinnamon are fine substitutes.
For more details on all of those things, plus why Kenyan coffee specifically may be the best for blood sugars, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
- The Bitter Truth About Coffee (or is it?)
- Caffeine: Cognitive Enhancer Or Brain-Wrecker?
- 10 Ways To Balance Blood Sugars
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: