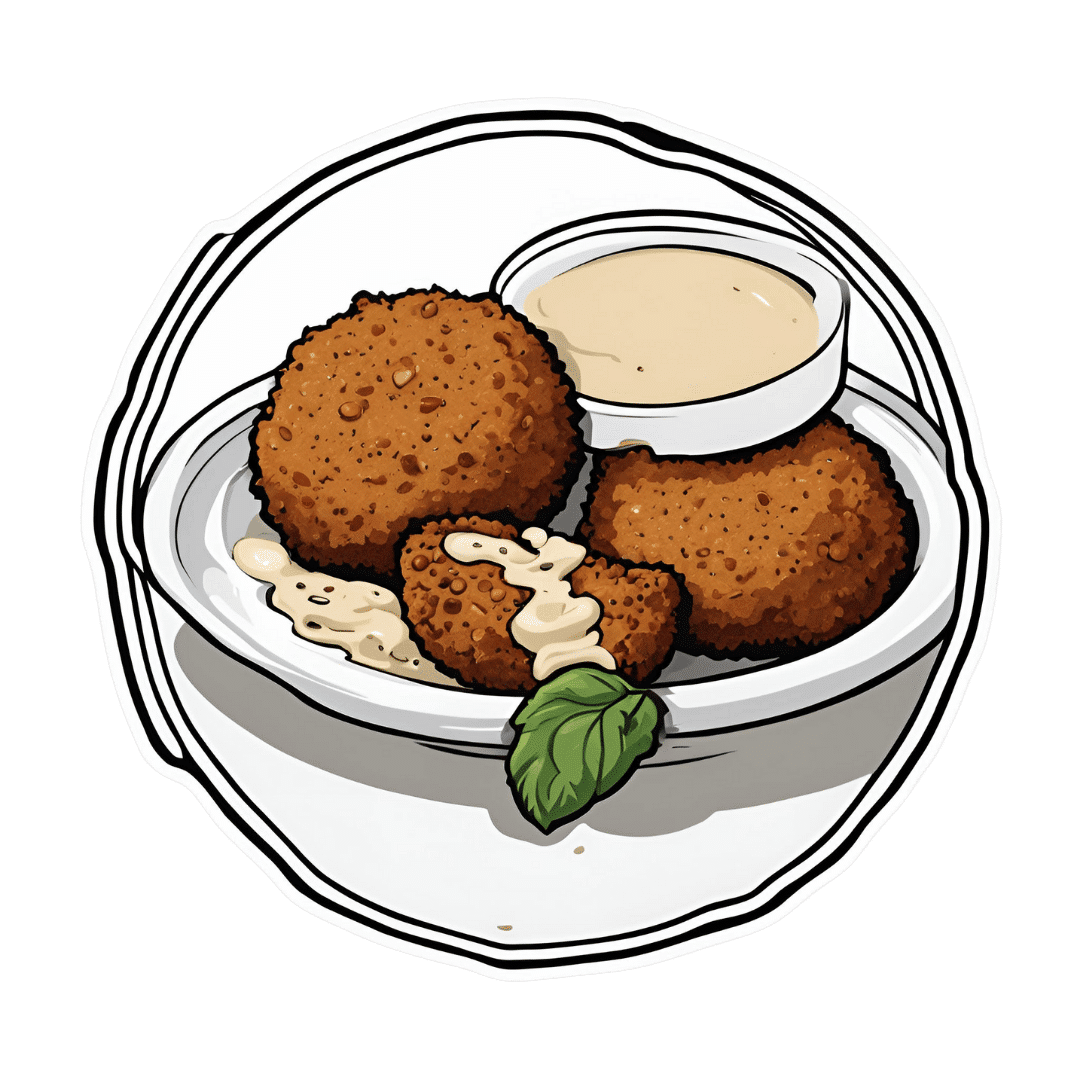
Mouthwatering Protein Falafel
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Baking falafel, rather than frying it, has a strength and a weakness. The strength: it is less effort and you can do more at once. The weakness: it can easily get dry. This recipe calls for baking them in a way that won’t get dry, and the secret is one of its protein ingredients: peas! Add to this the spices and a tahini sauce, and you’ve a mouthwatering feast that’s full of protein, fiber, polyphenols, and even healthy fats.
You will need
- 1 cup peas, cooked
- 1 can chickpeas, drained and rinsed (keep the chickpea water—also called aquafaba—aside, as we’ll be using some of it later)
- ½ small red onion, chopped
- 1 handful fresh mint, chopped
- 1 tbsp fresh parsley, chopped
- ½ bulb garlic, crushed
- 1 tbsp lemon juice
- 1 tbsp chickpea flour (also called gram flour, besan flour, or garbanzo bean flour) plus more for dusting
- 2 tsp red chili flakes (adjust per heat preferences)
- 2 tsp black pepper, coarse ground
- 1 tsp ground turmeric
- ½ tsp MSG or 1 tsp low-sodium salt
- Extra virgin olive oil
For the tahini sauce:
- 2 tbsp tahini
- 2 tbsp lemon juice
- ¼ bulb garlic, crushed
- 5 tbsp aquafaba (if for some reason you don’t have it, such as for example you substituted 1 cup chickpeas that you cooked yourself, substitute with water here)
To serve:
- Flatbreads (you can use our Healthy Homemade Flatbreads recipe if you like)
- Leafy salad
Method
(we suggest you read everything at least once before doing anything)
1) Preheat the oven to 350℉ / 180℃.
2) Blend the peas and chickpeas in a food processor for a few seconds. You want a coarse mixture, not a paste.
3) Add the rest of the main section ingredients except the olive oil, and blend again for a few more seconds. It should still have a chunky texture, or else you will have made hummus. If you accidentally make hummus, set your hummus aside and start again on the falafels.
4) Shape the mixture into balls; if it lacks structural integrity, fold in a little more chickpea flour until the balls stay in shape. Either way, once you have done that, dust the balls in chickpea flour.
5) Brush the balls in a little olive oil, as you put them on a baking tray lined with baking paper. Bake for 15–18 minutes until golden, turning partway through.
6) While you are waiting, making the tahini sauce by combining the tahini sauce ingredients in a high-speed blender and processing on high until smooth. If you do not have a small enough blender (a bullet-style blender should work for this), then do it manually, which means you’ll have to crush the garlic all the way into a smooth paste, such as with a pestle and mortar, or alternatively, use ready-made garlic paste—and then simply whisk the ingredients together until smooth.
7) Serve the falafels warm or cold, on flatbreads with leafy salad and the tahini sauce.

Enjoy!
Want to learn more?
For those interested in some of the science of what we have going on today:
- Tahini vs Hummus – Which is Healthier?
- Our Top 5 Spices: How Much Is Enough For Benefits? ← we scored 4/5 today!
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Dandelion Greens vs Collard Greens – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing dandelion greens to collard greens, we picked the dandelion greens.
Why?
Collard greens are great—they even beat kale in one of our previous “This or That” articles!—but dandelion greens simply pack more of a nutritional punch:
In terms of macros, dandelions have slightly more carbs (+3g/100g) for the same protein and fiber, and/but the glycemic index is equal (zero), so those carbs aren’t anything to worry about. Nobody is getting metabolic disease by getting their carbs from dandelion leaves. In short, we’re calling it a tie on macros, though it could nominally swing either way if you have an opinion (one way or the other) about the extra 3g of carbs.
In the category of vitamins, things are more exciting: dandelion greens have more of vitamins A, B1, B2, B3, B6, B7, B9, C, E, and K, while collard greens have more vitamin B5. An easy and clear win for dandelions.
Looking at the minerals tells a similar story; dandelion greens have much more calcium, copper, iron, magnesium, phosphorus, potassium, and zinc, while collard greens have slightly more manganese. Another overwhelming win for dandelions.
One more category, polyphenols. We’d be here until next week if we listed all the polyphenols that dandelion greens have, but suffice it to say, dandelion greens have a total of 385.55mg/100g polyphenols, while collard greens have a total of 0.08mg/100g polyphenols. Grabbing a calculator, we see that this means dandelions have more than 4819x the polyphenol content that collard greens do.
So, “eat leafy greens” is great advice, but they are definitely not all created equal!
Let us take this moment to exhort: if you have any space at home where you can grow dandelions, grow them!
Not only are they great for pollinators, but also they beat the collard greens that beat kale. And you can have as much as you want, for free, right there.
Want to learn more?
You might like to read:
Collard Greens vs Kale – Which is Healthier?
Enjoy!
Share This Post
-
Every Body Should Know This – by Dr. Federica Amati
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
This book is very much a primer on how to eat healthily. The science is high-quality (the author is the head nutritionist at ZOE) and well-explained, and the advice is reasonable.
Limitations: this book is not very deep, which we might expect from a book with this title. So, if you’ve been a long-time 10almonds reader, you might not learn a lot here, and this book might make a better gift for someone else.
In particular, the book may be well-suited for someone who is thinking of having children soon, as there is an unusual amount of focus on fertility and young motherhood—perhaps because the author herself has young children and so was preoccupied with this when writing. For those of us who are definitely not having any more children, the focus on young motherhood is a little superfluous.
The writing style is very readable pop-science, and nobody who is able to read English is likely to struggle with this one. It’s also quite conversational in parts, as the author discusses her own experiences with implementing the science at hand.
Bottom line: if you want a good, solid, primer of how to eat well for a lifetime of health, especially if you are (or are thinking of becoming) a young mother, then this is a very good book. Otherwise, it’s probably a better to give it as a gift.
Click here to check out Every Body Should Know This, and know the things!
Share This Post
-
Genius Foods – by Max Lugavere
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There is a lot of seemingly conflicting (or sometimes: actually conflicting!) information out there with regard to nutrition and various aspects of health. Why, for example, are we told:
- Be sure to get plenty of good healthy fats from nuts and seeds, for metabolic health and brain health too!
- But these terrible nut and seed oils lead to heart disease and dementia! Avoid them at all costs!
Max Lugavere demystifies this and more.
His science-led approach is primarily focused on avoiding dementia, and/but is at least not bad when it comes to other areas of health too.
He takes us on a tour of different parts of our nutrition, including:
- Perhaps the clearest explanation of “healthy” vs “unhealthy” fats this reviewer has read
- Managing carbs (simple and complex) for healthy glucose management—essential for good brain health
- What foods to improve or reduce—a lot you might guess, but this is a comprehensive guide to brain health so it’d be remiss to skip it
- The role that intermittent fasting can play as a bonus extra
While the main thrust of the book is about avoiding cognitive impairment in the long-term (including later-life dementia), he makes good, evidence-based arguments for how this same dietary plan improves cognitive function in the short-term, too.
Speaking of that dietary plan: he does give a step-by-step guide in a “make this change first, then this, then this” fashion, and offers some sample recipes too. This is by no means a recipe book though—most of the book is taking us through the science, not the kitchen.
Bottom line: this is the book for getting unconfused with regard to diet and brain health, making a lot of good science easy to understand. Which we love!
Click here to check out “Genius Foods” on Amazon today, give your brain a boost!
Share This Post
Related Posts
-
The Brain’s Way of Healing – by Dr. Norman Doidge
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
First, what this book isn’t: any sort of wishy-washy “think yourself better” fluff, and nor is it a “tapping into your Universal Divine Essence” thing.
In contrast, Dr. Norman Doidge sticks with science, and the only “vibrational frequencies” involved are the sort that come from an MRI machine or similar.
The author makes bold claims of the potential for leveraging neuroplasticity to heal many chronic diseases. All of them are neurological in whole or in part, ranging from chronic pain to Parkinson’s.
How well are these claims backed up, you ask?
The book makes heavy use of case studies. In science, case studies rarely prove anything, so much as indicate a potential proof of principle. Clinical trials are what’s needed to become more certain, and for Dr. Doidge’s claims, these are so far sadly lacking, or as yet inconclusive.
Where the book’s strengths lie is in describing exactly what is done, and how, to effect each recovery. Specific exercises to do, and explanations of the mechanism of action. To that end, it makes them very repeatable for any would-be “citizen scientist” who wishes to try (in the cases that they don’t require special equipment).
Bottom line: this book would be more reassuring if its putative techniques had enjoyed more clinical studies… But in the meantime, it’s a fair collection of promising therapeutic approaches for a number of neurological disorders.
Click here to check out The Brain’s Way of Healing, and learn more!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Food for Thought – by Lorraine Perretta
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
What are “brain foods”? If you think for a moment, you can probably list a few. What this book does is better.
As well as providing the promised 50 recipes (which themselves are varied, good, and easy), Perretta explains the science of very many brain-healthy ingredients. Not just that, but also the science of a lot of brain-unhealthy ingredients. In the latter case, probably things you already knew to stay away from, but still, it’s a good reminder of one more reason why.
Nor does she merely sort things into brain-healthy (or brain-unhealthy, or brain-neutral), but rather she gives lists of “this for memory” and “this against depression” and “this for cognition” and “this against stress” and so forth.
Perhaps the greatest value of this book is in that; her clear explanations with science that’s simplified but not dumbed down. The recipes are definitely great too, though!
Bottom line: if you’d like to eat more for brain health, this book will give you many ways of doing so
Click here to check out Food for Thought, and upgrade your recipes!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Track Your Blood Sugars For Better Personalized Health
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There Will Be Blood
Are you counting steps? Counting calories? Monitoring your sleep? Heart rate zones? These all have their merits:
- Steps: One More Resource Against Osteoporosis!
- Calories: Is Cutting Calories The Key To Healthy Long Life?
- Sleep: A Head-To-Head Of Google and Apple’s Top Apps For Getting Your Head Down
- Heart Rate Zones: Heart Rate Zones, Oxalates, & More
About calories: this writer (it’s me, hi) opines that intermittent fasting has the same benefits as caloric restriction, without the hassle of counting, and is therefore superior. I also personally find fasting psychologically more pleasant. However, our goal here is to be informative, not prescriptive, and some people may have reasons to prefer CR to IF!
Examples that come to mind include ease of adherence in the case of diabetes management, especially Type 1, or if one’s schedule (and/or one’s “medications that need to be taken with food” schedule) does not suit IF.
And now for the blood…
A rising trend in health enthusiasts presently is the use of Continuous Glucose Monitors (CGMs), which do exactly what is sounds like they do: they continually monitor glucose. Specifically, the amount of it in your blood.
Of course, these have been in use in diabetes management for years; the technology is not new, but the application of the technology is.
A good example of what benefits a non-diabetic person can gain from the use of a CGM is Jessie Inchauspé, the food scientist of “Glucose Revolution” and “The Glucose Goddess Method” fame.
By wearing a CGM, she was able to notice what things did and didn’t spike her blood sugars, and found that a lot of the things were not stuff that people knew/advised about!
For example, much of diabetes management (including avoiding diabetes in the first place) is based around paying attention to carbs and little else, but she found that it made a huge difference what she ate (or didn’t) with the carbs. By taking many notes over the course of her daily life, she was eventually able to isolate these patterns, showed her working-out in The Glucose Revolution (there’s a lot of science in that book), and distilled that information into bite-size (heh) advice such as:
10 Ways To Balance Blood Sugars
That’s great, but since people like Inchauspé have done the work, I don’t have to, right?
You indeed don’t have to! But you can still benefit from it. For example, fastidious as her work was, it’s a sample size of one. If you’re not a slim white 32-year-old French woman, there may be some factors that are different for you.
All this to say: glucose responses, much like nutrition in general, are not a one-size-fits-all affair.
With a CGM, you can start building up your own picture of what your responses to various foods are like, rather than merely what they “should” be like.
This, by the way, is also one of the main aims of personalized health company ZOE, which crowdsourced a lot of scientific data about personalized metabolic responses to standardized meals:
Not knowing these things can be dangerous
We don’t like to scaremonger here, but we do like to point out potential dangers, and in this case, blindly following standardized diet advice, if your physiology is not standard, can have harmful effects, see for example:
Diabetic-level glucose spikes seen in non-diabetic people
Where can I get a CGM?
We don’t sell them, and neither does Amazon, but you can check out some options here:
The 4 Best CGM Devices For Measuring Blood Sugar in 2024
…and if your doctor is not obliging with a prescription, note that the device that came out top in the above comparisons, will be available OTC soon:
The First OTC Continuous Glucose Monitor Will Be Available Summer 2024
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: