Most adults will gain half a kilo this year – and every year. Here’s how to stop ‘weight creep’
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
As we enter a new year armed with resolutions to improve our lives, there’s a good chance we’ll also be carrying something less helpful: extra kilos. At least half a kilogram, to be precise.
“Weight creep” doesn’t have to be inevitable. Here’s what’s behind this sneaky annual occurrence and some practical steps to prevent it.

Small gains add up
Adults tend to gain weight progressively as they age and typically gain an average of 0.5 to 1kg every year.
While this doesn’t seem like much each year, it amounts to 5kg over a decade. The slow-but-steady nature of weight creep is why many of us won’t notice the extra weight gained until we’re in our fifties.
Why do we gain weight?
Subtle, gradual lifestyle shifts as we progress through life and age-related biological changes cause us to gain weight. Our:
- activity levels decline. Longer work hours and family commitments can see us become more sedentary and have less time for exercise, which means we burn fewer calories
- diets worsen. With frenetic work and family schedules, we sometimes turn to pre-packaged and fast foods. These processed and discretionary foods are loaded with hidden sugars, salts and unhealthy fats. A better financial position later in life can also result in more dining out, which is associated with a higher total energy intake
- sleep decreases. Busy lives and screen use can mean we don’t get enough sleep. This disturbs our body’s energy balance, increasing our feelings of hunger, triggering cravings and decreasing our energy

- stress increases. Financial, relationship and work-related stress increases our body’s production of cortisol, triggering food cravings and promoting fat storage
- metabolism slows. Around the age of 40, our muscle mass naturally declines, and our body fat starts increasing. Muscle mass helps determine our metabolic rate, so when our muscle mass decreases, our bodies start to burn fewer calories at rest.
We also tend to gain a small amount of weight during festive periods – times filled with calorie-rich foods and drinks, when exercise and sleep are often overlooked. One study of Australian adults found participants gained 0.5 kilograms on average over the Christmas/New Year period and an average of 0.25 kilograms around Easter.
Why we need to prevent weight creep
It’s important to prevent weight creep for two key reasons:
1. Weight creep resets our body’s set point
Set-point theory suggests we each have a predetermined weight or set point. Our body works to keep our weight around this set point, adjusting our biological systems to regulate how much we eat, how we store fat and expend energy.
When we gain weight, our set point resets to the new, higher weight. Our body adapts to protect this new weight, making it challenging to lose the weight we’ve gained.
But it’s also possible to lower your set point if you lose weight gradually and with an interval weight loss approach. Specifically, losing weight in small manageable chunks you can sustain – periods of weight loss, followed by periods of weight maintenance, and so on, until you achieve your goal weight.

2. Weight creep can lead to obesity and health issues
Undetected and unmanaged weight creep can result in obesity which can increase our risk of heart disease, strokes, type 2 diabetes, osteoporosis and several types of cancers (including breast, colorectal, oesophageal, kidney, gallbladder, uterine, pancreatic and liver).
A large study examined the link between weight gain from early to middle adulthood and health outcomes later in life, following people for around 15 years. It found those who gained 2.5 to 10kg over this period had an increased incidence of type 2 diabetes, heart disease, strokes, obesity-related cancer and death compared to participants who had maintained a stable weight.
Fortunately, there are steps we can take to build lasting habits that will make weight creep a thing of the past.
7 practical steps to prevent weight creep
1. Eat from big to small
Aim to consume most of your food earlier in the day and taper your meal sizes to ensure dinner is the smallest meal you eat.
A low-calorie or small breakfast leads to increased feelings of hunger, specifically appetite for sweets, across the course of the day.
We burn the calories from a meal 2.5 times more efficiently in the morning than in the evening. So emphasising breakfast over dinner is also good for weight management.

2. Use chopsticks, a teaspoon or an oyster fork
Sit at the table for dinner and use different utensils to encourage eating more slowly.
This gives your brain time to recognise and adapt to signals from your stomach telling you you’re full.
3. Eat the full rainbow
Fill your plate with vegetables and fruits of different colours first to support eating a high-fibre, nutrient-dense diet that will keep you feeling full and satisfied.
Meals also need to be balanced and include a source of protein, wholegrain carbohydrates and healthy fat to meet our dietary needs – for example, eggs on wholegrain toast with avocado.
4. Reach for nature first
Retrain your brain to rely on nature’s treats – fresh vegetables, fruit, honey, nuts and seeds. In their natural state, these foods release the same pleasure response in the brain as ultra-processed and fast foods, helping you avoid unnecessary calories, sugar, salt and unhealthy fats.
5. Choose to move
Look for ways to incorporate incidental activity into your daily routine – such as taking the stairs instead of the lift – and boost your exercise by challenging yourself to try a new activity.
Just be sure to include variety, as doing the same activities every day often results in boredom and avoidance.

6. Prioritise sleep
Set yourself a goal of getting a minimum of seven hours of uninterrupted sleep each night, and help yourself achieve it by avoiding screens for an hour or two before bed.
7. Weigh yourself regularly
Getting into the habit of weighing yourself weekly is a guaranteed way to help avoid the kilos creeping up on us. Aim to weigh yourself on the same day, at the same time and in the same environment each week and use the best quality scales you can afford.
At the Boden Group, Charles Perkins Centre, we are studying the science of obesity and running clinical trials for weight loss. You can register here to express your interest.
Nick Fuller, Clinical Trials Director, Department of Endocrinology, RPA Hospital, University of Sydney
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Recommended
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Healing Arthritis – by Dr. Susan Blum
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We previously reviewed another book by this author, her Immune System Recovery Plan, and today it’s more specific: healing arthritis
Of course, not all arthritis is rooted in immune dysfunction, but a) all of it is made worse by immune dysfunction and b) rheumatoid arthritis, which is an autoimmune disease, affects 1% of the population.
This book tackles all kinds of arthritis, by focusing on addressing the underlying causes and treating those, and (whether it was the cause or not) reducing inflammation without medication, because that will always help.
The “3 steps” mentioned in the subtitle are three stages of a plan to improve the gut microbiome in such a way that it not only stops worsening your arthritis, but starts making it better.
The style here is on the hard end of pop-science, so if you want something more conversational/personable, then this won’t be so much for you, but if you just want the information and explanation, then this does it just fine, and it has frequent references to the science to back it up, with a reassuringly extensive bibliography.
Bottom line: if you have arthritis and want a book that will help you to get either symptom-free or as close to that as is possible from your current condition (bearing in mind that arthritis is generally degenerative), then this is a great book for that.
Share This Post
-
Hate Sit-Ups? Try This 10-Minute Standing Abs Routine!
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Abdominal muscles are important to many people for aesthetics; they also fulfil the important role of keeping your innards in, as well as being a critical part of core stability (and you cannot have a truly healthy back without healthy abs on the other side). However, not everyone loves sit-ups and their many variations, so here’s an all-standing workout instead:
On your feet!
The exercise are as follows:
- High knees: engage core to work abs; do slow for low impact. Great for speeding up the metabolism. Jog during rest to keep moving.
- Extend & twist: raise arms high, drive them down while raising one leg into a twist. No rest, switch sides immediately.
- Extend & vertical crunch: extend leg back, drive knee forward into a crunch. Swap sides with no breaks.
- Oblique jacks: jump or slow version; targeting the obliques.
- Front toe-touch: engage core for effectiveness.
- Crossover toe-touch: no break; move into this directly from the front toe-touch.
- Wood chop: lift arms up, twist, chop down. Great for obliques. No rest between sides.
- Heisman: step side to side, bringing your other knee up towards the opposite side. Focus on core engagement rather than speed.
- Side leg raise & side bent: raise leg to side with slight bend; works obliques. No rest between sides.
That’s it!
For a visual demonstration, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Is A Visible Six-Pack Obtainable Regardless Of Genetic Predisposition?
Take care!
Share This Post
-
Heavy Metal Detox In A Pill?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
We have previous discussed assorted approaches to “detoxing”:
Detox: What’s Real, What’s Not, What’s Useful, What’s Dangerous?
Today we’re going to be looking at one we didn’t cover there, which is zeolite.
What is zeolite?
Zeolite is a mineral that occurs naturally and can also be synthesized, and it’s famous for absorbing other stuff from around it. Because of this property, it’s used in many things, including:
- Petrochemical catalysis
- Water treatment
- Nuclear waste reprocessing
- Cat litter
- Supplements (for detox purposes)
That’s, uh… An interesting list, isn’t it? So, we were curious as to whether this mineral that’s also used in fish tank filters is, in fact, overpriced gravel being sold to the gullible as a health supplement.
We had to do some digging on this one
Our journey didn’t start well, with this very dubious-looking paper being cited by a company selling zeolite supplements:
This immediately prompted two questions:
- Who is eating graphene?!* That stuff does not occur in nature (or at least; it hasn’t ever been found; the universe is a big place so it might exist elsewhere), has only relatively recently been synthesized, is very difficult to produce, is two-dimensional while being hard as diamonds, and exists only in truly tiny lab-made quantities worldwide. It would be orders of magnitude easier to find and eat uranium.
- Is this a reputable journal? Which question was easier to answer than the former one, and the answer is “no”; we hadn’t heard of this journal (ACTA Scientific), and neither it seems had most of the Internet, but we did find it on a list of predatory journals, here.
*The citation given in the above paper should by rights answer the question of who is eating graphene, since by rights they must have demonstrated it somehow, but it just doesn’t. Instead, it links to what it claims is a paper titled “Oxygenated Zeolite (Clinoptilite) Efficiently Removes Aluminum & Graphene Oxide”, but is in reality just someone’s blog post with a screenshot of an actual paper entitled “Novel, oxygenated clinoptilolite material efficiently removes aluminium from aluminium chloride-intoxicated rats in vivo”). Looking up this real paper in its real journal, it does not mention graphene.
All this to say: sometimes, unscrupulous people will just plain lie to you, which is why peer review is important, as is sourcing data from reputable journals. Which is what we do for you so that you don’t have to 🙂
It does, actually, work though (for heavy metal detox)
Notwithstanding the aforementioned bunk, we found this from a more reputable publisher:
❝In this study, we have presented clinical evidence supporting the use of an activated clinoptilolite (zeolite) suspension to safely and effectively increase the urinary excretion of potentially toxic heavy metals in healthy volunteers without negatively impacting the electrolyte profiles of the participants.
Significant increases in the urinary excretion of aluminum, antimony, arsenic, bismuth, cadmium, lead, mercury, nickel and tin were observed in the subjects participating in the two study groups as compared to placebo controls.❞
Also good for the gut and against inflammation
Specifically, it’s good for gut barrier integrity, i.e., against “leaky gut syndrome”:
❝Twelve weeks of zeolite supplementation exerted beneficial effects on intestinal wall integrity as indicated via decreased concentrations of the tight junction modulator zonulin.
This was accompanied by mild anti-inflammatory effects in this cohort of aerobically trained subjects.❞
May also be good against neurodegenerative diseases
If it is (which is plausible), it’ll probably because of removing heavy metals and improving gut barrier integrity—in other words, the things we just looked at in the two reputable peer-reviewed studies we examined above.
But the science is young for this one; here’s the current state of things:
Zeolite and Neurodegenerative Diseases
Is it safe?
Safety reviews have found it to be safe, for example:
Critical Review on Zeolite Clinoptilolite Safety and Medical Applications in vivo
However, if you are taking regular medications, we recommend checking with your pharmacist or doctor to ensure that zeolite will not also remove those medications from your system!
Want to try some?
We don’t sell it, but here for your convenience is an example product on Amazon 😎
Enjoy!
Share This Post
Related Posts
-
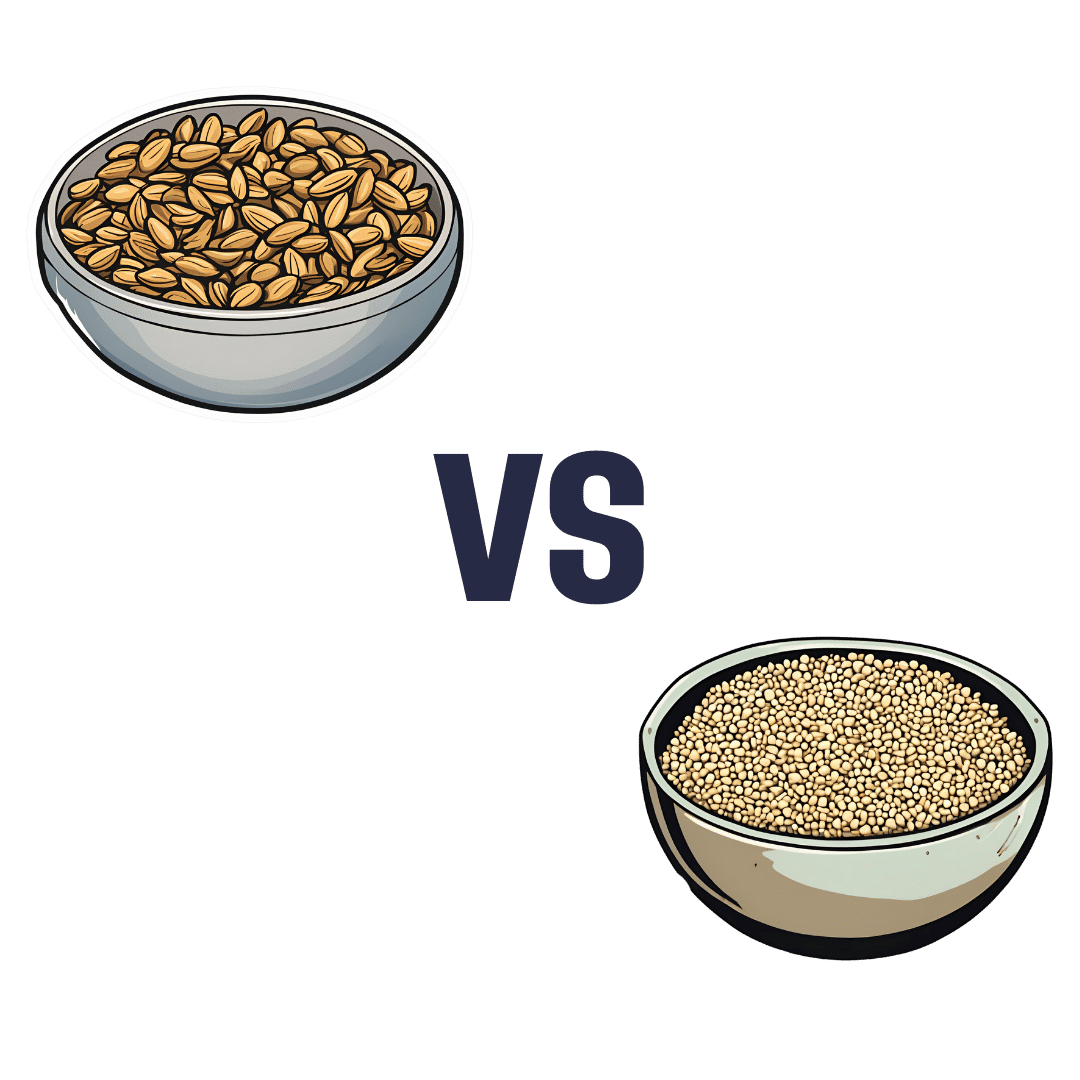
Sunflower Seeds vs Sesame Seeds – Which is Healthier?
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Our Verdict
When comparing sunflower seeds to sesame seeds, we picked the sunflower.
Why?
In moderation, both are very healthy. We say “in moderation” because they’re both about 50% fat and such fats, while vital for life, are generally best enjoyed in small portions. Of that fat, sunflower has the slightly better fat profile; they’re both mostly poly- and monounsaturated fats, but sunflower has 10% saturated fat while sesame has 15%. Aside from fats, sunflower has slightly more protein and sesame has slightly more carbs. While sesame has slightly more fiber, because of the carb profile sunflower still has the lower glycemic index. All in all, a moderate win for sunflower in the macros category.
You may be wondering, with all that discussion of fats, what they’re like for omega-3, and sesame seeds have more omega-3, though sunflower seeds contain it too. Still, a point in sesame’s favor here.
When it comes to vitamins, sunflower has more of vitamins A, B1, B2, B3, B5, B6, B9, C, E, and choline, while sesame is not higher in any vitamins.
In the category of minerals, sunflower has more phosphorus, potassium, and selenium, while sesame has more calcium, copper, iron, and zinc. This is nominally a marginal win for sesame, but it should be noted that sunflower is still very rich in copper, iron, and zinc too (but not calcium).
Adding up the categories makes for a moderate win for sunflower seeds, but as ever, enjoy both; diversity is best!
Want to learn more?
You might like to read:
Sunflower Seeds vs Pumpkin Seeds – Which is Healthier?
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Eating For Energy (In Ways That Actually Work)
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
Snacks & Hacks: The Real Energy Boosters
Declining energy levels are a common complaint of people getting older, and this specific kind of “getting older” is starting earlier and earlier (even Gen-Z are already getting in line for this one). For people of all ages, however, diet is often a large part of the issue.
The problem:
It can sometimes seem, when it comes to food and energy levels, that we have a choice:
- Don’t eat (energy levels decline)
- Eat quick-release energy snacks (energy spikes and crashes)
- Eat slow-release energy meals (oh hi, post-dinner slump)
But, this minefield can be avoided! Advice follows…
Skip the quasi-injectables
Anything the supermarket recommends for rapid energy can be immediately thrown out (e.g. sugary energy drinks, glucose tablets, and the like).
Same goes for candy of most sorts (if the first ingredient is sugar, it’s not good for your energy levels).
Unless you are diabetic and need an emergency option to keep with you in case of a hypo, the above things have no place on a healthy shopping list.
Aside from that, if you have been leaning on these heavily, you might want to check out yesterday’s main feature:
The Not-So-Sweet Science Of Sugar Addiction
…and if your knee-jerk response is “I’m not addicted; I just enjoy…” then ok, test that! Skip it for this month.
- If you succeed, you’ll be in better health.
- If you don’t, you’ll be aware of something that might benefit from more attention.
Fruit and nuts are your best friends
Unless you are allergic, in which case, obviously skip your allergen(s).
But for most of us, we were born to eat fruit and nuts. Literally, those two things are amongst the oldest and most well-established parts of human diet, which means that our bodies have had a very long time to evolve the perfect fruit-and-nut-enjoying abilities, and reap the nutritional benefits.
Nuts are high in fat (healthy fats) and that fat is a great source of energy’s easy for the body to get from the food, and/but doesn’t result in blood sugar spikes (and thus crashes) because, well, it’s not a sugar.
See also: Why You Should Diversify Your Nuts
Fruit is high in sugars, and/but high in fiber that slows the absorption into a nice gentle curve, and also contains highly bioavailable vitamins to perk you up and polyphenols to take care of your long-term health too.
Be warned though: fruit juice does not work the same as actual fruit; because the fiber has been stripped and it’s a liquid, those sugars are zipping straight in exactly the same as a sugary energy drink.
See also: Which Sugars Are Healthier, And Which Are Just The Same?
Slow release carbs yes, but…
Eating a bowl of wholegrain pasta is great if you don’t have to do anything much immediately afterwards, but it won’t brighten your immediately available energy much—on the contrary, energy will be being used for digestion for a while.
So if you want to eat slow-release carbs, make it a smaller portion of something more-nutrient dense, like oats or lentils. This way, the metabolic load will be smaller (because the portion was smaller) but the higher protein content will prompt satiety sooner (so you addressed your hunger with a smaller portion) and the iron and B vitamins will be good for your energy too.
See also: Should You Go Light Or Heavy On Carbs?
Animal, vegetable, or mineral?
At the mention of iron and B vitamins, you might be thinking about various animal products that might work too.
If you are vegetarian or vegan: stick to that; it’s what your gut microbiome is used to now, and putting an animal product in will likely make you feel ill.
If you have them in your diet already, here’s a quick rundown of how broad categories of animal product work (or not) for energy:
- Meat: nope. Well, the fat, if applicable, will give you some energy, but less than you need just to digest the meat. This, by the way, is a likely part of why the paleo diet is good for short term weight loss. But it’s not very healthy.
- Fish: healthier than the above, but for energy purposes, just the same.
- Dairy: high-fat dairy, such as cream and butter, are good sources of quick energy. Be aware if they contain lactose though, that this is a sugar and can be back to spiking blood sugars.
- As an aside for diabetics: this is why milk can be quite good for correcting a hypo: the lactose provides immediate sugar, and the fat keeps it more balanced afterwards
- Eggs: again the fat is a good source of quick energy, and the protein is easier to digest than that of meat (after all, egg protein is literally made to be consumed by an embryo, while meat protein is made to be a functional muscle of an animal), so the metabolic load isn’t too strenuous. Assuming you’re doing a moderate consumption (under 3 eggs per day) and not Sylvester Stallone-style 12-egg smoothies, you’re good to go.
See also: Do We Need Animal Products To Be Healthy?
…and while you’re at it, check out:
Eggs: Nutritional Powerhouse
or Heart-Health Timebomb?(spoiler: it’s the former; the title was because it was a mythbusting edition)
Hydration considerations
Lastly, food that is hydrating will be more energizing than food that is not, so how does your snack/meal rank on a scale of watermelon to saltines?
You may be thinking: “But you said to eat nuts! They’re not hydrating at all!”, in which case, indeed, drink water with them, or better yet, enjoy them alongside fruit (hydration from food is better than hydration from drinking water).
And as for those saltines? Salt is not your friend (unless you are low on sodium, because then that can sap your energy)
How to tell if you are low on sodium: put a little bit (e.g. ¼ tsp) of salt into a teaspoon and taste it; does it taste unpleasantly salty? If not, you were low on sodium. Have a little more at five minute intervals, until it tastes unpleasantly salty. Alternatively have a healthy snack that nonetheless contains a little salt.
If you otherwise eat salty food as an energy-giving snack, you risk becoming dehydrated and bloated, neither of which are energizing conditions.
Dehydrated and bloated at once? Yes, the two often come together, even though it usually doesn’t feel like it. Basically, if we consume too much salty food, our homeostatic system goes into overdrive to try to fix it, borrows a portion of our body’s water reserves to save us from the salt, and leaves us dehydrated, bloated, and sluggish.
For more on salt in general, check out:
How Too Much Salt Can Lead To Organ Failure: Lesser-Known Salt Health Risks
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails:
-
Top 5 Anti-Aging Exercises
10almonds is reader-supported. We may, at no cost to you, receive a portion of sales if you purchase a product through a link in this article.
There are some exercises that get called such things as “The King of Exercises!”, but how well-earned is that title and could it be that actually a mix of the top few is best?
The Exercises
While you don’t have to do all 5, your body will thank you if you are able to:
- Plank: strengthens most of the body, and can reduce back pain while improving posture.
- Squats: another core-strengthening exercise, this time with an emphasis on the lower body, which makes for strong foundations (including strong ankles, knees, and hips). Improves circulation also, and what’s good for circulation is good for the organs, including the brain!
- Push-ups: promotes very functional strength and fitness; great for alternating with planks, as despite their similar appearance, they work the abs and back more, respectively.
- Lunges: these are great for lower body strength and stability, and doing these greatly reduces the risk of falling.
- Glute Bridges: this nicely rounds off one’s core strength, increasing stability and improving posture, as well as reducing lower back pain too.
If the benefits of these seem to overlap a little, it’s because they do! But each does some things that the others don’t, so put together, they make for a very well-balanced workout.
For advice on how to do each of them, plus more about the muscles being used and the benefits, enjoy:
Click Here If The Embedded Video Doesn’t Load Automatically!
Want to learn more?
You might also like to read:
Take care!
Don’t Forget…
Did you arrive here from our newsletter? Don’t forget to return to the email to continue learning!
Learn to Age Gracefully
Join the 98k+ American women taking control of their health & aging with our 100% free (and fun!) daily emails: